Abstract
Residual coronary heart disease remains a significant problem even after adequate statin therapy for cardiovascular risk reduction as currently recommended by the Adult Treatment Panel III (ATP-III) of the National Cholesterol Education Program (NCEP). This is particularly true for the high risk patients as defined by ATP-III that includes those patients who have a greater than 20% 10-year risk of adverse cardiac events. For such patients the current goal of a low-density lipoprotein cholesterol (LDL-cholesterol) maintenance level of ≤100 mg/dL plasma appears to be suboptimal. Accumulating data from several recent randomized studies of more aggressive LDL-cholesterol reduction to levels below 70 mg/dL in the high risk patients favor acceptance of such a new lower target for LDL-cholesterol using more intensive statin therapy which would affect the treatment strategy for patients with coronary heart disease pre-percutaneous intervention, metabolic syndrome, diabetes mellitus, congestive heart failure, cerebrovascular disease and chronic kidney disease.
Introduction
Cardiovascular disease (CVD) continues to be the leading cause of mortality and morbidity in the United States. The cost of CVD care surpassed US$450 billion in 2008 according to the National Heart, Lung, and Blood Institute (NHLBI). Although the strategy of aggressively lowering the low-density lipoprotein cholesterol (LDL-cholesterol) with statins has significantly decreased the cardiac events, a substantial number of CVD events still occur, as seen in the majority of trials of aggressive versus standard statin therapy. This is especially true for the patients who are generally classified as being high risk according to the National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III). Several randomized trials have evaluated increasingly aggressive lipid-lowering therapy in these patients, and therefore the lipid treatment strategy needs to go beyond the current recommendation for the high risk patients. Institution of very aggressive secondary prevention strategy, and aggressive reduction of LDL-cholesterol levels to below 70 mg/dL, are rightly recommended for the very high risk patients. This group includes patients with coronary heart disease (CHD) and presentation with acute myocardial infarction (AMI) or acute coronary syndromes (ACS) as per the 2004 update of the initial 2001 NCEP-ATP III report. However, these recommendations fall short of addressing a variety of CHD patients at high risk who continue to exhibit an acceptable level of residual risk for recurrent acute coronary events. Several recent trials, such as the Treating to New Targets (TNT) trial, the Collaborative Atorvastatin Diabetes Study (CARDS), the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL), and the Lipid-Lowering Arm of the Anglo-Scandinavian Cardiac Outcomes Study (ASCOT-LLA) trial, lend support to the idea that greater LDL-cholesterol lowering than that achieved with standard dose of statins may be warranted in high risk patients as well. Such evidence-based studies in high risk patients supporting the use of high dose statins are discussed in this review.
High risk patients
High risk patients are defined as those who already have had manifest CHD or CHD equivalents, such as diabetes mellitus (DM), peripheral vascular disease (PVD), cerebrovascular disease (C-VD), or abdominal aortic aneurysm (Figure ).Citation1 Chronic kidney disease (CKD) is also considered a CHD equivalent condition by some authors. These patients have greater than 20% 10-year risk of acute cardiac events according to the Framingham Heart Study risk score calculations. Patients with features of metabolic syndrome (MS) exhibit similar high risk prognosis. In addition, patients presenting with acute coronary syndrome (ACS), or those pre-percutaneous intervention (pre-PCI), also form a group of high risk patients who appear to derive greater benefit with increasingly more aggressive statin therapy and reduction of LDL-cholesterol to ∼70 mg/dL range.
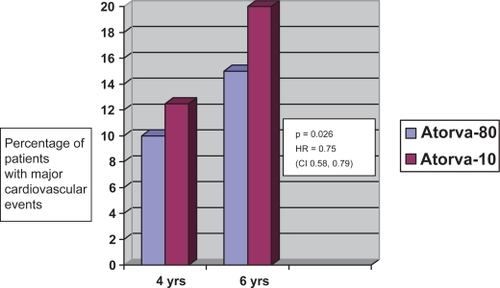
Figure 1 Kaplan-Meier estimates of the incidence of major cardiovascular events in patients with diabetes mellitus (includes congestive heart failure death, non-fatal nonprocedure-related acute myocardial infarction, resuscitated cardiac arrest, and fatal or non-fatal stroke).
Institution of similar aggressive treatment strategy for these high risk patients as has been recommended for the very high risk group was recently studied in a randomized clinical trial called the Treating to New Targets (TNT) trial that randomized 10,001 patients. It unequivocally showed that for these high risk patients, an additional highly aggressive reduction of LDL-cholesterol level to under 70 mg/dL through the use of a high dose of atorvastatin (80 mg daily) did decrease the cardiac risk even more significantly than the current strategy of moderate LDL-cholesterol reduction to a level just below 100 mg/dL generally achievable with low dose of atorvastatin (10 mg daily). In the Scandinavian Simvastatin Survival Study (4S) with 5 years of follow-up, twice as much risk reduction was seen in the patients with diabetes as in those without diabetes. These and other similar studies are reviewed in detail below.
Trials of aggressive statin therapy
Ever since the introduction of statin agents for the treatment of hypercholesterolemia for reduction of CHD, increasingly more aggressive treatment has, over the years, shown increasingly more significant proportionat benefit. The target LDL-cholesterol has continued to slide down to lower levels as more evidence has accumulated through the randomized trials of the past decade. In the Pravastatin and Atorvastatin Evaluation and Infection Therapy (PROVE-IT TIMI 32) study, much more aggressive reduction of LDL than recommended by NCEP-ATP III guidelines was undertaken using high dose statins, and increasingly greater reduction in cardiovascular events was observed in the patients with CHD who presented with ACS/non-ST-elevation myocardial infarction (NSTEMI).Citation2 The LDL-cholesterol level decreased to 62 mg/dL in the patients who took a high dose of atorvastatin (80 mg daily) compared with those who took simvastatin (40 mg daily). The LDL-cholesterol level in the simvastatin group was reduced to only ∼95 mg/dL. Even though this level was consistent with NCEP recommendations, the atorvastatin group with more aggressive LDL reduction showed an additional ∼25% decrease in the cardiovascular event rate. The Heart Protection Study (HPS) exhibited similar results in all participants, including the subjects whose baseline LDL-cholesterol level was under 100 mg/dL, and who were treated with simvastatin.Citation3 The treated subgroup showed a significantly lower event rate of 16.4% than the placebo group, at 21%. Following the release of the data from these studies, the NCEP-ATP III panel met in 2004, and updated its 2001-guidelines by adding an optional LDL goal of 70 mg/dl for CHD patients who fell in the “very high risk” category, such as the patients who present with AMI or ACS/NSTEMI).Citation1,Citation4 For all other CHD patients or those with CHD “risk equivalent” features the recommended LDL target level is still 100 mg/dL. It should be noted that these patients consistently continue to exhibit a “high” (≥20%) 10-year risk as predicted by the Framingham Risk score tables for both men and women. Such a high residual risk and recurrent event rate should be unacceptable, and strategies must be developed to decrease this risk.
Over the past several years, new trials have generated a wealth of evidence supporting a new strategy for increasingly aggressive risk reduction even in the yet neglected subgroup of non-acute CHD patients who are at higher risk because of the presence of multiple risk factors, and who, too, may benefit from more intense LDL-cholesterol reduction. The TNT trial randomized 10,001 patients with stable CHD and baseline LDL-cholesterol level under 130 mg/dL into two groups – first, an aggressive strategy group, to be treated with high dose atorvastatin (80 mg/day) with goal LDL ≤ 70 mg/dL)) and the other, a moderate strategy group, to be treated with regular dose atorvastatin (10 mg per day) with goal LDL-cholesterol ≤100 mg/dL.Citation5 After a 5-year follow up, the results from the TNT study convincingly exhibited an additional ∼35% decrease in the level of LDL-cholesterol and a proportionate reduction in cardiac event rate in the aggressive strategy cohort compared with the moderate strategy cohort. Subsequent examination of various subgroups, such as those with DM, MS, congestive heart failure (CHF), and renal insufficiency, unequivocally showed statistically significant additional event reduction in the aggressive LDL-cholesterol treatment group (goal: 62 mg/dL with 80 mg of atorvastatin daily) over and above the currently recommended ≤100 mg/dL LDL-cholesterol level generally achievable with 10 mg of atorvastatin daily.Citation6–Citation9 Several other trials have recently added more evidence to the literature demonstrating similar benefit of increasingly aggressive reduction in the level of LDL-cholesterol even in patients with average baseline cholesterol levels who do not yet have manifest CHD, but are at a relatively higher risk owing to the concomitant presence of risk factors. ASCOT-LLA showed reliable evidence for the use of statins in patients with so-called normal cholesterol levels who have hypertension and three other additional cardiac risk factors.Citation51 In CARDS, primary prevention of cardiovascular events with 10 mg of atorvastatin daily was undertaken in patients with type 2 diabetes but without manifest CHD.Citation50 High dose atorvastatin was shown to be safe and significantly effective in decreasing the risk of cardiovascular events, including stroke. Furthermore, in the SPARCL trial, atorvastatin given as 80 mg daily to patients with history of prior stroke or transient ischemic attack (TIA) but with normal cholesterol levels and without CHD resulted in significant improvement in the clinical outcomes. Citation52
Thus, it has now become abundantly clear from these randomized trials that there now exists an evidence-base supporting the clinical indications for high dose atorvastatin for treating high risk patients. Such increasingly aggressive LDL-cholesterol reduction as part of a secondary prevention strategy in patients with already diagnosed CHD, and for primary prevention in patients with various risk factors including DM, MS, CHF and renal insufficiency, appears to be the next step in decreasing the cardiac risk even further. We will now review and discuss the evidence-based data from such randomized studies in CHD and CHD equivalent conditions that constitute the high risk patients.
Table 1 Goals and end points for lipid-lowering therapy (modified from NCEP ATP III recommendations)
Diabetes mellitus (DM)
Patients with DM are considered high risk since DM constitutes a CHD equivalent condition as described in the NCEP-ATP III report.Citation4 According to the Framingham risk score calculations, patients with adult-onset diabetes, even those without clinically manifest CHD, fall in the high risk category with a 20% 10-year risk for recurrent or adverse coronary events.Citation28,Citation29 Diabetics who experience an AMI fair worse than non-diabetic patients.Citation30 A major underlying risk factor in diabetes patients is the atherogenic dyslipidemia generally manifested by high triglyceride, low values for high-density lipoprotein cholesterol (HDL-cholesterol), and an abundance of smaller, denser, and highly atherogenic LDL particles.Citation31 Lowering the elevated level of LDL-cholesterol with statins to the current goal of ≤100 mg/dL causes significant reductions in cardiovascular events in patients with diabetes and CHD.Citation32,Citation33 However, high residual risk persists. Newer studies suggest the need for further lowering the goal LDL-cholesterol level for patients with CHD who have high risk co-morbidities.Citation1,Citation2 DM is one such co-morbid state. While the American Diabetes Association (ADA) still recommends an LDL-cholesterol target of ≤100 mg/dL, the potential for a more aggressive LDL-cholesterol reduction to a goal level of ≤70 mg/dL may be additionally beneficial.Citation34 The recently concluded TNT study supports such a strategy for diabetic patients. In this trial increasingly aggressive LDL-cholesterol reduction in patients with established CHD was evaluated in a randomized fashion.Citation5 Decrement of the mean LDL-cholesterol level to approximately 77 mg/dL using 80 mg of atorvastatin daily resulted in additional 22% risk reduction compared with the currently recommended strategy involving decrement to a mean LDL-cholesterol level of about 101 mg/dL using 10 mg of atorvastatin per day.Citation27 Further sub-analysis of the diabetic patients in the TNT study was carried out to see whether similar magnitude of clinical benefits of lowering LDL-cholesterol levels to new levels below what is currently recommended can be achieved, and whether that would translate into actual improvement in the clinical outcome. This sub-analysis included 1501 diabetic patients with mean LDL-cholesterol levels of 130 mg/dL, who had been randomized to double-blind therapy with either high dose atorvastatin (80 mg daily, n = 748) or low dose atorvastatin (10 mg daily, n = 753) and followed for 4.9 years. Primary end point of the TNT study included the time to first major cardiovascular event (ie, CHD death, non-fatal AMI, cardiac arrest, or stroke. The final mean LDL-cholesterol level was 98.6 mg/dL in the low dose atorvastatin group and 77.0 mg/dL with high dose atorvastatin. The primary end point was seen in 17.9% patients receiving atorvastatin 10 mg, compared with 13.8% receiving atorvastatin 80 mg (hazard ratio [HR] 0.75 [95% CI 0.58 −0.97], p = 0.026). This translated to a 25% reduction in the risk of major cardiovascular events in support of the high-dose strategy (HR 0.75 [95% CI 0.58–0.97], p = 0.026) (Figure ). Significant event reduction was observed in the high dose atorvastatin cohort as compared with the low dose atorvastatin group across all quintiles of age, duration of diabetes, and low or high HbA1c (HbA1c ≤ 7% or >7%, respectively). Furthermore, a significant event reduction in the group on high dose atorvastatin was also seen for time to cerebrovascular event or TIA (0.69 [0.48–0.98], p = 0.037) and any cardiovascular event (0.85 [0.73–1.00], p = 0.044). There was, however, no significant difference observed between the two groups for all cause mortality. Out of the 8,500 patients without the diagnosis of diabetes at initial screening, 865 patients (10.2%) developed DM during the course of the study – 425 in the 10-mg atorvastatin cohort and 440 in the high dose atorvastatin group (odds ratio 1.04, p = 0.59). Thus, the data from the TNT sub-analysis demonstrate that lowering the LDL-cholesterol with high dose atorvastatin therapy to levels well below 100 mg/dL is safe. It showed no significant increase in adverse events among patients with diabetes and CHD who were on high dose atorvastatin compared with the low dose atorvastatin group. For example, among the diabetes patients, the overall adverse event rate was 7.0% in the high dose atorvastatin group and 5.4% in the low dose group. The incidence of myalgia was 2.4% and 3.6% in the high dose and low dose cohorts respectively, and the difference was not statistically significant. Persistent elevations in alanine aminotransferase (ALT) and/or aspartate aminotransferase (AST) above the 3 times the upper limit of normal were seen in 0.9% of patients receiving 80 mg of atorvastatin daily and in 0.4% in those receiving 10 mg of atorvastatin daily (p = ns). No incidents of rhabdomyolysis were encountered.
Similarly, a subgroup analysis of the 4S study indicated that cholesterol lowering with simvastatin improves prognosis in diabetic patients with CHD.Citation32 An analysis of the 202 diabetic patients and 4242 non-diabetic patients with previous MI or angina pectoris, and raised serum cholesterol level, was performed and the findings were compared. At the end of the 5.4-year median follow-up, while the simvastatin-treated group showed similar mean changes in serum lipids in diabetic and non-diabetic patients, the relative risk (RR) of the principal endpoints in the simvastatin-treated diabetic patients was significantly lower. The risk ratio for total mortality was 0.57 (95% CI, 0.30–1.08; p = 0.087), for major coronary events 0.45 (95% CI, 0.27–0.74; p = 0.002), and that for any atherosclerotic event 0.63 (95% CI, 0.43–0.92; p = 0.018). The corresponding RRs in non-diabetic patients were 0.71 (95% CI, 0.58–0.87; p = 0.001), 0.68 (95% CI, 0.60–0.77; p < 0.0001), and 0.74 (95% CI, 0.68–0.82; p < 0.0001), respectively. These results indicate that the absolute clinical benefit achieved by cholesterol lowering may be greater in diabetic than in non-diabetic patients with CHD because diabetic patients have a higher absolute risk of recurrent coronary events and other atherosclerotic events to begin with. The ADA, in 2005, updated the clinical practice recommendations for the diabetics with CHD, with clear emphasis on the fact that diabetic patients are at very high risk for future clinical events.Citation34 On the basis of the data from the randomized trials of moderate versus aggressive lipid lowering in populations at very high risk, the ADA now recommends the use of high dose statins for reducing the LDL-cholesterol to a new goal, ie, under 70 mg/dL as a therapeutic option.Citation1,Citation5,Citation27,Citation35 The analysis of the diabetic patients in the TNT study also provides strong evidence of significant cardiovascular risk reduction with high dose statin therapy irrespective of their initial LDL-cholesterol level, age, duration of diabetes, or the intensity of glycemic control when compared with low dose treatment.
A primary prevention strategy of cardiovascular risk reduction with atorvastatin was studied in the CARDS trial, involving patients with adult-onset diabetes mellitus who had normal levels of baseline LDL-cholesterol.Citation50 The study included 2838 patients aged 40 to 75 years who were randomized to placebo (n = 1410) or atorvastatin 10 mg daily (n = 1428). It was conducted at 132 centers throughout the UK and Ireland. Study participants had no prior history of CHD, abnormally high LDL-cholesterol level, retinopathy, albuminuria, tobacco abuse, or hypertension. Primary endpoints included time to first occurrence of acute coronary events, coronary revascularization, or stroke. The CARDS trial was terminated 2 years earlier than expected because of the strongly positively result, ie, higher efficacy in the atorvastatin-treated patients. At the median duration of follow-up of 3.9 years, at least one major cardiovascular event occurred in 127 patients receiving placebo (2.46 per 100 person-years at risk) versus 83 who received atorvastatin (1.54 per 100 person-years at risk) with rate reduction of 37% (95% CI −52 to −17, p = 0.001). Treatment would be expected to prevent at least 37 major vascular events per 1000 patients over 4 years. Acute coronary heart disease events were reduced by 36% (−55 to −9), coronary revascularizations by 31% (−59 to 16), and stroke by 48% (−69 to −11). Atorvastatin reduced the overall mortality by 27% (−48 to 1, p = 0.059). Adverse event rates were not statistically different in the atorvastatin group compared with placebo. In other words, in patients with type 2 diabetes without elevated baseline LDL-cholesterol, atorvastatin 10 mg daily was found to be safe and effective in reducing the risk of first cardiovascular events and stroke. These data strongly support the fact that all diabetics should receive statin treatment irrespective of their LDL-cholesterol concentration.
Metabolic syndrome (MS)
Over the past decade abundant evidence has accumulated to the fact that presence of metabolic syndrome significantly predicts the cardiovascular events, and has become an important prognostic factor. MS, unlike individual risk factors, is an interesting combination of related risk factors. It is generally described as a multiplex risk factor that essentially encompasses a synergistic clustering of a number of several cardiovascular risk factors that in many ways are interrelated and highly predictive of future events.Citation10–Citation15 The organizations, such as the NCEP-ATP and the International Diabetes Federation (IDF), have defined MS as a condition that includes coexistence of at least three of the following five risk factors: (1) hypertension, (2) hyperglycemia, (3) hypertriglyceridemia, (4) hypo-alphalipoproteinemia, and (5) increased waist circumference as surrogate for central obesity (men >40 inches [100 cm]; women >35 inches [90 cm]).Citation3,Citation4,Citation17 The third report of the NCEP-ATP, in 2001, emphasized the importance of treating metabolic risk factors as the next target second only to the primary target, ie, LDL-cholesterol.Citation4 These guidelines were updated in 2004 when NCEP added an optional LDL-cholesterol goal of less than 70 mg/dL in high risk patients, including patients who present with AMI or ACS. This stricter goal is now being considered as the new target level for LDL-cholesterol for the patients with established CHD who have associated high risk co-morbidities, such as MS.Citation3 These suggestions are consistent with the guidelines on prevention of cardiovascular disease already published by the Joint British Societies (desired LDL-cholesterol ≤ 80 mg/dL) and the secondary prevention guidelines of the American Heart Association (AHA) and American College of Cardiology (ACC) sanctioned by the NHLBI (LDL-cholesterol ≤ 70 mg/dL considered desirable).Citation18
The agreement among various international guidelines for CHD risk reduction emphasizing the fact that the various risk factors need to be considered together as a multi-factorial risk-complex for prognostic as well as for therapeutic purposes is on the increase. The knowledge that MS is a significantly predictive and relatively treatable multi-factorial risk factor for heart disease is now becoming more commonplace.Citation19–Citation20 Recently, in a joint statement, the ADA and the AHA reiterated the significance of diagnosing and managing the critical set of risk factors that constitute MS (pre-diabetes, hypertension, dyslipidemia, and obesity) in order to curtail the ballooning burden of CHD and diabetes mellitus.Citation21
Notwithstanding the plentiful evidence of the importance of MS for predicting cardiovascular events, not many trials have looked at the benefits of statin drugs on cardiovascular morbidity and mortality in persons with MS and CHD. A sub-analysis of the TNT trial evaluated whether aggressive lowering of LDL-cholesterol with high dose atorvastatin provides superior cardiovascular benefit for patients with both CHD and MS than the current strategy of mere moderate LDL-cholesterol reduction with regular dose atorvastatin.
The sub-analysis of the TNT study looking at the patients with and without MS included 5584 patients who were randomized to low dose atorvastatin (10 mg per day; n = 2820) or high dose atorvastatin (80 mg per day; n = 2764). The primary endpoint included the time to first major cardiovascular event – defined as death from CHD, non-fatal non-procedure-related MI, resuscitated cardiac arrest, or fatal or non-fatal stroke. In the patients with CHD and MS, mean on-treatment LDL-cholesterol concentrations at 3 months were 99.3 mg/dL with low dose atorvastatin, and 72.6 mg/dL with high-dose atorvastatin. At a median follow-up of 4.9 years, major cardiovascular events occurred in 13% patients receiving atorvastatin 10 mg, compared with 9.5% receiving atorvastatin 80 mg (HR 0.71; 95% CI 0.61–0.84; p < 0.0001). Irrespective of treatment assignment, significantly more patients with MS (11.3%) had a major cardiovascular event than those without MS (8.0%; HR1.44; 95% CI 1.26–1.64; p < 0.0001). This increased risk was significantly reduced by 29% in those on intensive therapy with atorvastatin 80 mg beyond that achieved with regular dose atorvastatin 10 mg (Table ). Statistically significant differences between the groups in favor of high dose atorvastatin 80 mg were also seen for the secondary end points, such as time to any cardiovascular event (0.78, 0.71–0.85; p < 0.0001), major coronary event (0.72, 0.60–0.86; p = 0.0004), any coronary even (0.75, 0.67–0.83; p < 0.0001), cerebrovascular event (0.74, 0.59–0.93; p =0.011), and hospitalization for CHF (0.73, 0.55–0.96; p = 0.027). There was no significant difference between the two treatments for all-cause mortality. In the subgroup of MS patients without diabetes, while only 8.2% persons receiving atorvastatin 80 mg had a primary event, a much larger number, ie, 11.6% receiving atorvastatin 10 mg, experienced the primary event. These findings represent a 30% relative reduction in the risk of a major cardiovascular event in favor of the high dose atorvas-tatin subset (0.70, 0.57–0.84; p = 0.0002). One of the important facts is that there exists a 44% greater absolute risk in CHD patients with MS than in the CHD patients without MS. This fact adds justification and provides a particularly compelling rationale for more intensive LDL-lowering therapy in CHD patients with MS.Citation22
Table 2 Cardiovascular events in patients with metabolic syndrome at various doses of atorvastatin
Aggressive therapy with high dose atorvastatin seems to be safe as well. The adverse events rate elated to treatment was similar between the two groups. A total of 153 patients (5.4%) assigned to atorvastatin 10 mg discontinued the drug because of adverse events related to treatment compared with 178 patients (6.4%) randomly assigned atorvastatin 80 mg (not statistically significant). Persistent elevations in liver enzymes greater than three times the upper limit of normal (3 × ULN) obtained a week apart were reported in 0.2% of patients receiving atorvastatin 10 mg and 1.1% of those receiving atorvastatin 80 mg. None of the patients a exhibited persistent rise in the concentration of creatine phosphokinase (CPK) or rhabdomyolysis.
There are, though, a few limitations to the extrapolation of these results from the TNT study. First, the study enrolled only those with clinically evident CHD. Thus, the added benefits of treating patients with MS beyond the current LDL-cholesterol goal of under 100 mg/dL may not be extrapolated to the MS patients without CHD.Citation20 Second, there is yet no universally accepted definition of MS. Although waist circumference might be more closely linked to cardiovascular risk factors than body-mass index (BMI), the two parameters are closely correlated. Generally, a BMI > 28 in men has shown close agreement with obesity prevalence estimated by using waist circumference.Citation24,Citation25 For this reason, the MS subset of the TNT study was also analyzed with a definition of MS incorporating a BMI > 30, but no differences were seen in the outcome. In the 4S study, a standard dose of simvastatin (20 or 40 mg) was compared with placebo in patients with established CHD.Citation27 A post-hoc analysis showed that patients with MS benefited from simvastatin therapy by at least as much as those without MS. It should be noted that the MS patients entered 4S with a mean LDL-cholesterol of 190 mg/dL, which was reduced to around 120 mg/dL by simvastatin therapy. By contrast, in the TNT study, MS patients entered the double-blind treatment phase with a mean LDL-cholesterol of 98 mg/dL, representing a normal baseline LDL-cholesterol level. An aggressive atorvastatin therapy regimen further reduced LDL-cholesterol to 73 mg/dL, and it was correlated with additional significant clinical benefit.
There has been some debate on the strategic importance of MS in clinical practice.Citation23 The TNT study clearly shows that the relative risk for major cardiovascular events rises as the number of components of MS increase, particularly when three or more synergistically cluster together. The latter essentially constitutes the definition of MS.Citation3,Citation17 The patients with MS and CHD in the TNT study were at greater risk at baseline than those without. Thus, despite a similar drop in the relative risk with statin therapy in patients with and without MS, the absolute benefit was greater in those with MS because of their higher baseline absolute risk than those without MS. In conclusion, the TNT study provides the much-needed evidence that patients with CHD and MS are good candidates for aggressive lipid-lowering therapy with statins.Citation3,Citation19 It is even more important if they also have DM.
Chronic kidney disease (CKD)
Patients with CKD are at increased risk for adverse cardiovascular outcomes. In the past several years, a significant amount of data has been published suggesting that CKD is also one of the CHD-disease equivalent conditions. In the US, about 8 million individuals carry a diagnosis of CKD of at least stage III severity (a glomerular filtration rate [GFR] of <60 mL/min/1.73 m2).Citation44 Furthermore, approximately 500,000 Americans have end-stage renal disease. The elevated risk of cardiovascular mortality and morbidity in patients with advanced CKD is already well known. Studies over the past decade have given further evidence that the renal dysfunction is a significant independent predictor of CHD including the patients with just mild renal insufficiency.Citation45 Subgroup analyses of several recent randomized studies show that statins may have a protective effect on renal function.Citation46 In the Heart Protection Study, involving 15,696 patients with CHD, peripheral arterial disease, or DM, randomization to simvastatin 40 mg/day was associated with a smaller fall in the estimated GFR (eGFR) compared with placebo after an average follow-up of 4.6 years.Citation47 In the Cholesterol And Recurrent Events (CARE) study in the patients with hyperlipidemia and previous AMI, pravastatin 40 mg daily led to a significant protection manifested by the reduction in the rate of decline of eGFR among subjects with baseline chronic renal insufficiency (eGFR of <40 mL/min/1.73 m2) compared with placebo. Furthermore, in the Aggressive Lipid-Lowering Initiation Abates New Cardiac Events (ALLIANCE) study, a strategy of aggressive atorvastatin treatment led to the prevention of the otherwise anticipated decline in the renal function over the 4 years of follow-up, and it tended to modify or slow the progression of CKD compared with usual care.Citation48 The safety data for atorvastatin in CKD patients are also acceptable. In both primary and secondary cardiovascular prevention trials, atorvastatin has been shown to reduce the CHD risk without any significant safety concerns.Citation1,Citation35,Citation49,Citation50
The subgroup analysis of the TNT study further evaluated the renoprotective effect with higher dose atorvastatin treatment to see whether such an effect was graded and dose-dependent. eGFR using the Modification of Diet in Renal Disease (MDRD) equation was compared at baseline and at the end of follow-up. Mean eGFR at baseline was 65.6 ± 11.4 mL/min/1.73 m2 in the atorvastatin 10 mg group and 65.0 ± 11.2 mL/min/1.73 m2 in the atorvastatin 80 mg group. At the end of follow-up, mean eGFR increased by 5.2 ± 0.14 mL/min/1.73 m2 in the atorvastatin 80 mg group as compared with only modest 3.5 ± 0.14 mL/min/1.73 m2 increase in the atorvastatin 10 mg group representing the increases of 8.3% and 5.6%, respectively (p < 0.0001). In the high dose atorvastatin cohort, eGFR improved to >60 mL/min/1.73 m2 in significantly more subjects (45.6% vs 37.8%) and declined to <60 mL/min/1.73 m2 in significantly fewer subjects (6.6% vs 9.2%) than in the low dose atorvastatin cohort. Among the participants with a baseline eGFR > 60 mL/min/1.73 m2, significantly fewer subjects showed a decline to <60 mL/min/1.73 m2 in the atorvastatin 80 mg group than in the atorvastatin 10 mg group (6.6% vs 9.2% (p < 0.0001) (Table ). Furthermore, out of those patients with a baseline eGFR < 60 mL/min/1.73 m2, significantly more in the high dose atorvastatin group improved to >60 mL/min/1.73 m2 at the end of the study than in the lowdose atorvastatin group (45.6% vs 37.8%; p = 0.0001) (Table ). Among the participants who already had a diagnosis of CKD at baseline (eGFR < 60 mL/min/1.73 m2), 80 (5.3%) assigned to atorvastatin 10 mg and 54 (3.4%) assigned to atorvastatin 80 mg experienced a decline in eGFR of 25% or greater (p = 0.0077). The TNT study essentially exhibited significant cardiovascular benefits of aggressive LDL-cholesterol lowering to the new low targets that are below the current target recommended by the guidelines.Citation27 The analysis among patients with impaired renal function demonstrated that in addition to the cardiac effects, the benefits of an aggressive atorvastatin treatment strategy extended to significant improvement in the renal function with high dose statin therapy over that achieved with low dose atorvastatin treatment regimen. The expected decline in renal function was eliminated over the 5 years of the TNT study. It should, however, be noted that the absence of an untreated control arm is an acknowledged limitation of the TNT trial. Nonetheless, such renoprotective effects are of particular importance in patients with GFR < 60 mL/min/1.73 m2 who, with additional loss of renal function, are at significantly greater risk for future cardiovascular events.Citation45 The observation that eGFR showed an improvement in the TNT study appears to have been related to the aggressiveness of the statin therapy. These data demonstrating renal benefits with high dose atorvastatin over those achieved with low dose atorvastatin add to the growing evidence base for non-cardiac benefits (pleotropic effects) of statins. Although the mechanisms responsible for nephroprotection with statins have yet to be defined, the strategy of lowering LDL-cholesterol levels to well below 100 mg/dL with high dose atorvastatin appears to maximize renal benefits in high risk patients with CHD, and is indicated even in the patients with moderate CKD. There were no unexpected safety concerns identified even in the high dose atorvastatin arm. Equivalent rates of adverse events were seen in each of the treatment groups (p = ns). The percentage of participants who had persistent elevations in liver function enzymes (two measurements of ALT and/or AST > 3 × ULN obtained a week apart) was numerically larger in the atorvastatin 80 mg group than in the atorvas-tatin 10 mg group, but was generally low and similar to that observed in the overall TNT population for both participants with CKD (1.4% vs 0.1%) and those with normal eGFR (1.2% vs 0.2%). No subject had clinically persistent elevated CPK values (two measurements of CPK > 10 × ULN).
Table 3 Percentage of patients with decline or improvement from baseline eGFR
Cerebro-vascular disease (C-VD)
Atherosclerosis is a systemic disease, and statin therapy benefits atherosclerosis as a whole. Several clinical trials involving the use of statins have demonstrated that lowering cholesterol with statins reduces the risk of stroke as well as providing cardiac benefits in patients with CHD or even in those without manifest CHD, but with presence of major risk factors. A meta-analysis of 26 trials showed a relative risk reduction of 21% for all varieties of stroke without significant increase in hemorrhagic stroke. Fatal strokes were reduced by 9%. The statin effect was closely associated with a reduction in LDL-cholesterol. Each 10% reduction in LDL-cholesterol decreased the risk of all strokes by 13.2%.
Currently, in patients with ischemic stroke but no prior history of a coronary event, no clear recommendation for use of statins has been available, even though such patients make up 80% of the stroke population. A recent study, the SPARCL study, was the first study that set out to evaluate prospectively the effects of statin therapy in patients who previously had a stroke or TIA and who had no known CHD.Citation52 The main entry criteria for men and women included the following: (i) Previously documented stroke (ischemic or hemorrhagic) or TIA, 1 to 6 months before randomization, (ii) LDL-cholesterol ≥ 100 mg/dL and ≤190 mg/dL, and (iii) Modified Rankin score ≤3 (ie, functionally independent). Patients were excluded if they already had a history of CHD, significant peripheral vascular disease, atrial fibrillation, prosthetic heart valve, clinically significant mitral stenosis, sinus node dysfunction, uncontrolled hypertension, stroke caused by a revascularization procedure or trauma, subarachnoid hemorrhage, or liver or renal disease. A total of 4731 patients were enrolled into the trial. The mean age (approximately 62.5 years) and male/female ratio (60%/40%) meant that the SPARCL patients were more representative of the true stroke population, with a substantially higher percentage of women and a mean age approximately 5 years older than the populations of major CHD statin trials. Approximately 20% of the SPARCL patients were current smokers, 62% were hypertensive, 16% had diabetes, and 20% had carotid stenosis. Thirty percent of the patients had history of prior TIA and 70% a prior stroke, of which about 3% were hemorrhagic. Within 30 days of initial screening, patients were randomized to receive either atorvastatin 80 mg/day (2365 patients) or placebo (2366 patients). The patients were followed for a mean of 4.9 years (maximum 6.6 years). The average baseline LDL-cholesterol was 133 mg/dL, which fell by 38% in the atorvastatin group over the average 4.4-year follow-up, versus a 7% fall in the placebo group. This appeared to translate into a significant reduction in the primary end point of recurrent stroke, with an adjusted hazard ratio of 0.84 in the atorvastatin group. The treated group also showed significant reductions in fatal stroke and ischemic stroke and there was a trend toward fewer non-fatal strokes. There was, however, a significant increase in the rate of hemorrhagic stroke. The number of patients who need to be treated for 5 years with atorvastatin to prevent 1 stroke is 46; to prevent 1 major cardiovascular event, 29; and to prevent 1 revascularization procedure, 32. Despite the slight increase in the incidence of hemorrhagic stroke in the treatment cohort, the benefit versus risk ratio favored atorvastatin for stroke reduction (11.2% vs 13.1%, respectively, p = 0.03), as well as for stroke plus major coronary events reduction (14.1% vs 17.2%, p = 0.002). These data, thus, clearly support the recommendation that atorvastatin 80 mg/day should be started in all patients with stroke or TIA soon after the episode for future risk reduction.
Congestive heart failure (CHF)
CHF constitutes another high risk group of patients. It should be noted that CHF is the only cardiac diagnosis for which the incidence as well as prevalence has been on the rise. This may be a reflection of better treatment of acute events, the survivors of which may be at a greater risk of developing a chronic disabling condition such as CHF. Statins have been shown to reduce cardiovascular events in patients with and without known CHD in many randomized clinical trials. Patients with CHF were usually not included in these trials. It should also be noted that CHD and CHF commonly coexist, as described above. Recently, a few randomized trials have ventured to address this issue. Some older observations have shown that statins have a potential benefit in the treatment for CHF. As we know, CHF is a pathophysiologic condition commonly driven by neuro-hormonal activation, inflammation, and endothelial dysfunction. In small studies, statins have been shown to improve endothelial functionCitation2 and to lower plasma levels of pro-inflammatory cytokines in patients with CHD who also have dyslipidemia. Statins generally have multiple pleotropic effects including antihypertrophic, antioxidant, and antifibrotic influences on the myocardium. Thus, they may affect immune function, macrophage metabolism, and cell proliferation independently of changes in LDL-cholesterol concentration.Citation16,Citation37,Citation38 In addition, by preventing recurrent ischemia in patients with CHD, statins may prevent the development or deterioration of CHF. On the other hand, there are valid concerns about the fact that statins may cause higher rates of adverse effects in such patients.Citation39 Some observational studies have indicated that there exists an association between low cholesterol levels and adverse outcomes in advanced CHF, and lowering the levels too low may be deleterious.Citation40 It has been suggested that the decrease in ubiquinone levels caused by statin therapy may be responsible for these deleterious consequences because ubiquinone is a potential antioxidant and CHF is a condition of pro-oxidant stress.Citation41 The TNT trial was the first randomized clinical trial to demonstrate the benefits of aggressive LDL-cholesterol lowering in patients with CHD. The intensive treatment regimen consisted of a high dose’regimen (80 mg daily of atorvastatin), which was compared with a low dose regimen (10 mg atorvastatin daily) in 10,001 patients with the diagnosis of stable CHD, defined as prior MI, prior or current angina with evidence of coronary artery disease, or prior history of coronary revascularization. Patients with advanced heart failure (New York Heart Association [NYHA] class IIIb or IV or left ventricular ejection fraction <30%) were excluded from the trial. Over a mean follow-up of 4.9 years, the high dose of atorvastatin lowered LDL-cholesterol to a mean of ∼77 mg/dL vs a mean of ∼101 mg/dL with the low dose. This additional more aggressive drop in LDL-cholesterol levels lowered the risk for a major cardiovascular event, the primary end point of the trial, by 22% compared with the low dose regimen. One of the predefined secondary end points, hospitalization for CHF, occurred in 2.4% of the 80 mg dose group compared with 3.3% of the 10 mg dose group – a relative risk reduction of 26% (HR 0.74, 95% CI 0.59–0.94, p < 0.012) (Figure ). These findings add to the increasing evidence of benefit with statins in the treatment of patients with CHF.
Even though the patients with advanced CHF were not included in the TNT trial, 7.5% of the high dose group and 8.1% of the low dose group had a history of CHF at baseline (self-reported). When the TNT patients were divided into those with or without history of CHF, the effect of the high dose statin on CHF hospitalization became even more marked in the patients reporting a history of CHF at baseline. These patients showed a 41% reduction in risk compared with a 13% reduction in hospitalizations in the group without a history of CHF. Compared with patients with no CHF hospitalizations, those who were hospitalized with CHF during the trial had lower rates of beta-blocker (45.1% vs 54.0%) and aspirin (74.1% vs 86.9%) use at baseline and higher rates of angiotensin-converting enzyme inhibitor (50.3% vs 26.5%), angiotensin receptor blocker (10.5% vs 5.1%), aldosterone antagonist (1.4% vs 0.3%), and diuretic use (50.3% vs 13.3%). The benefit did not appear to be mediated by a reduction in preceding ischemic events in most cases and appeared to be related to the degree of LDL-cholesterol lowering. There was a 0.6% reduction in risk of CHF hospitalization for each 1 mg/dL (0.259 mmol/L) reduction in LDL-cholesterol (p = 0.007). Regardless of the statistical correlation with lower LDL-cholesterol in the high dose group, however, it appears that the benefit on CHF hospitalization is not only due to LDL-cholesterol lowering but also due to some other pleotropic effects of atorvastatin. Furthermore, aggressive therapy with atorvastatin even in patients with stable CHD significantly reduces subsequent hospitalizations for CHF compared with regular less aggressive therapy. This benefit was most pronounced in patients with a baseline history of CHF. Also, the CHF hospitalizations were not usually preceded by an ischemic coronary event, suggesting that the 80 mg atorvastatin therapy may confer increased benefit through other mechanisms as yet undefined.
Pre-percutaneous intervention (pre-PCI) patients
Patients who are going to undergo PCI, especially those who present with ACS, clearly appear to have lower recurrent cardiovascular events with intensive statin therapy as demonstrated by the PROVE-IT trial. Furthermore, patients with stable and unstable coronary syndromes do better if pre-treated with high dose statins prior to PCI as shown in the Atorvastatin for Reduction of Myocardial Damage during Angioplasty (ARMYDA)Citation55 and ARMYDA-ACSCitation56 trials. In the ARMYDA trial, 153 patients with stable CHD and chronic stable angina were enrolled and were pre-treted with atorvastatin 40 mg/day for 7 days prior to PCI. This strategy significantly reduced ‘procedural’ myocardial injury in such patients undergoing elective coronary intervention. Post-procedural peak levels of troponin-I were 0.09 ± 0.2 vs 0.47 ± 0.13 for patients with and without atorvastatin pre-treatment respectively (p = 0.0008). In the Atorvastatin for Reduction of Myocardial Damage During Angioplasty-Acute Coronary Syndromes (ARMYDA-ACS) trial, patients were randomized in a double-blind manner to pretreatment with atorvastatin (80 mg 12 hours prior to PCI and 40 mg immediately pre-PCI; n = 86) or matching placebo (n = 85). After the procedure, all patients were treated with atorvastatin 40 mg indefinitely. Blood samples for biomarker evaluation were drawn immediately pre-PCI and at 8 and 24 hours post-PCI. Among patients with ACS undergoing PCI, pretreatment with atorvastatin 80 mg was associated with a reduction in major adverse cardiac events at 30 days compared with placebo, driven exclusively by a reduction in periprocedural MI. Results of the present study are similar to the original ARMYDA study, which also showed a reduction in periprocedural MI with atorvastatin pretreatment but in a low-risk, stable angina, elective PCI population. When feasible, treatment with a loading dose of atorvastatin pre-PCI appears promising. In another study, Herrmann et al stratified 296 consecutive patients who were undergoing stenting of a de novo stenosis according to the pre-procedural status of statin therapy (229 statin-treated and 67 control patients). Incidence of periprocedural myocardial injury was assessed by analysis of creatine kinase (CK; ULN 70 IU/L for women, 80 IU/L for men) and cardiac troponin T (cTnT; bedside test; threshold 0.1 ng/mL) before and 6, 12, and 24 hours after the intervention. Relative to control patients, the incidence of CK elevation >3 × ULN was more than 90% lower in statin-treated patients (0.4% vs 6.0%, p = 0.01). Statin therapy was the only factor independently associated with a lower risk of CK elevation >3 × ULN (odds ratio 0.08, 95% CI 0.01–0.75; p = 0.03). The overall incidences of CK and cardiac troponin T elevation were slightly lower in statin-treated than in control patients (14.4% vs 20.9%, p = 0.3, and 17.9% vs 22.4%, p = 0.5, respectively). Therefore, pre-procedural statin therapy was demonstrated to reduce the incidence of larger-sized, post-PCI MI.Citation57
Newer trials of statin therapy in high risk patients
The strategy of aggressive lipid lowering with high dose statins in patients with high risk of CHD appears to be gaining momentum. These suggestions are also supported by data from morphological studies, such as REVERSAL and the Study To Evaluate the Effect of Rosuvastatin on Intravascular Ultrasound-Derived Coronary Atheroma Burden (ASTEROID), which used high doses of potent statins, ie, atorvastatin and rosuvastatin respectively. The REVERSing Atherosclerosis with Aggressive Lipid Lowering (REVERSAL) study measured changes in atheroma burden as assessed by intravascular ultrasound (IVUS) in 654 patients aged 35 to 78 years with symptomatic CHD and at least ≥20% stenosis by coronary angiography. Baseline LDL-cholesterol was between 125 and 210 mg/dL after an 8-week washout period. Patients were randomized to moderate lipid lowering with pravastatin 40 mg or intensive lipid lowering with atorvastatin 80 mg for 18 months. By the end of the treatment period, LDL-cholesterol was significantly lower among patients who had received atorvastatin compared with those on pravastatin. The primary prespecified endpoint of the trial was change in IVUS-determined atheroma volume, which showed a significant increase in the pravastatin arm compared with baseline (progression), versus no overall change (absence of increase) in atheroma volume in patients in the atorvastatin arm. An unpaired comparison of the treatment arms showed a significant difference in progression rate (p = 0.02). Although no net regression of atheroma was found for the atorvastatin group, individual patients in this group experienced significant regression.Citation53 The intensive statin therapy regimen was also tested in ASTEROID. The treatment group similarly showed significant regression of atherosclerosis as measured by IVUS.Citation54
Conclusion
CVD continues to be the leading cause of mortality and morbidity. Over the past several years, although the strategy of aggressively lowering the LDL-cholesterol with statins has significantly decreased cardiac events, an unacceptable number of CVD events still occur in treated patients, as is apparent from the majority of the studies of aggressive versus standard statin therapy. This is especially true for the patients who are generally classified as being high risk. The data from several of the randomized trials now strongly favor the use of high dose atorvastatin, and recommend aggressive versus usual LDL-cholesterol reduction as part of new strategy for the CHD patients as well as those with various CHD risk-equivalent conditions such as DM, MS, CKD and peripheral/cerebrovascular disease, as well as those who are pre-PCI.
Disclosures
The authors declare no conflicts of interest.
References
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in AdultsExecutive summary of the third report of the national cholesterol education program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)JAMA20012852486249711368702
- CannonCPIntensive versus moderate lipid lowering with statins after acute coronary syndromes (PROVE-IT Study)N Engl J Med20043501495150415007110
- Heart Protection Study Collaborative GroupMRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomized placebo-controlled trialLancet200236072212114036
- GrundySMImplications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelinesCirculation200411022723915249516
- WatersDDTreating to New Targets (TNT) Study: does lowering low-density lipoprotein cholesterol levels below currently recommended guidelines yield incremental clinical benefit?Am J Cardiol20049315415814715339
- DeedwaniaPReduction of low-density lipoprotein cholesterol in patients with coronary heart disease and metabolic syndrome: analysis of the Treating to New Targets studyLancet200636891992816962881
- ShepherdJEffect of lowering LDL cholesterol substantially below currently recommended levels in patients with coronary heart disease and diabetes: The Treating to New Targets (TNT) studyDiabetes Care2006291220122616731999
- KhushKEffect of high-dose atorvastatin on hospitalizations for heart failure: subgroup analysis of the Treating to New Targets studyCirculation200711557658317261662
- ShepherdJEffect of intensive lipid lowering with atorvastatin on renal function in patients with coronary heart disease: the Treating to New Targets (TNT) studyClin J Am Soc Nephrol200721131113917942759
- WingardDLClustering of heart disease risk factors in diabetic compared to nondiabetic adultsAm J Epidemiol198311719266823949
- SternMPBody fat distribution and hyperinsulinemia as risk factors for diabetes and cardiovascular diseaseArteriosclerosis198661231303513749
- ReavenGMBanting lecture 1988. Role of insulin resistance in human diseaseDiabetes198837159516073056758
- SattarNMetabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention StudyCirculation200310841441912860911
- DeedwaniaPCMetabolic syndrome and vascular disease: is nature or nurture leading the new epidemic of cardiovascular disease?Circulation20041092414707015
- GirmanCJThe metabolic syndrome and risk of major coronary events in the Scandinavian Simvastatin Survival Study (4S) and the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS)Am J Cardiol20049313614114715336
- OiSLovastatin prevents angiotensin II–induced cardiac hypertrophy in cultured neonatal rat heart cellsEur J Pharmacol199937613914810440099
- AlbertiKGThe metabolic syndrome – a new worldwide definitionLancet20053661059106216182882
- British Cardiac Society, British Hypertension Society, Diabetes UK, HEART UK, Primary Care Cardiovascular Society, Stroke AssociationJBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practiceHeart200591Suppl 5v1v5216365341
- SmithSCJrAHA/ACC guidelines for secondary prevention for patients with coronary and other atheroscle-rotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood InstituteCirculation20061132363237216702489
- GrundySMDiagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific StatementCirculation20051122735275216157765
- EckelRHPreventing cardiovascular disease and diabetes A call to action from the American Diabetes Association and the American Heart AssociationCirculation20061132943294616801475
- BaigentCEfficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statinsLancet20053661267127816214597
- KahnRThe metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of DiabetesDiabetes Care2005282289230416123508
- ZhuSWaist circumference and obesity-associated risk factors among whites in the third National Health and Nutrition Examination Survey: clinical action thresholdsAm J Clin Nutr20027674374912324286
- FordESIncreasing prevalence of the metabolic syndrome among US adultsDiabetes Care2004272444244915451914
- Scandinavian Simvastatin Survival Study GroupRandomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S)Lancet1994344138313897968073
- LaRosaJCIntensive lipid lowering with atorvastatin in patients with stable coronary diseaseN Engl J Med3521425143515755765
- AlmdalTThe independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death: a population based study of 13,000 men and women with 20 years of follow-upArch Intern Med20041641422142615249351
- StamlerJDiabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention TrialDiabetes Care1993164344448432214
- HaffnerSMMortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarctionN Engl J Med19983392292349673301
- HaffnerSMMortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarctionN Engl J Med19983392292349673301
- PyoralaKCholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease: a subgroup analysis of the Scandinavian Simvastatin Survival Study (4S)Diabetes Care206146209096989
- KeechASecondary prevention of cardiovascular events with long-term pravastatin in patients with diabetes or impaired fasting glucose: results from the LIPID trialDiabetes Care2003262713272114514569
- American Diabetes Association: Standards of medical care in diabetes (Position Statement)Diabetes Care200528Suppl 1S4S3615618112
- KorenMJClinical outcomes in managed-care patients with coronary heart disease treated aggressively in lipid-lowering disease management clinics: the ALLIANCE studyJ Am Coll Cardiol2004441772177915519006
- TreasureCBBeneficial effects of cholesterol-lowering therapy on the coronary endothelium in patients with coronary artery diseaseN Engl J Med19953324814877830728
- LaufsUUpregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitorsCirculation199897112911359537338
- VaughanCJStatins do more than just lower cholesterolLancet1996348107910828874463
- KrumHStatins and chronic heart failure: do we need a large-scale outcome trial?J Am Coll Cardiol2002391567157312020481
- HorwichTBLow serum total cholesterol is associated with marked increase in mortality in advanced heart failureJ Card Fail2002821622412397569
- MortensenSADose-related decrease of serum coenzyme Q10 during treatment with HMG-CoA reductase inhibitorsMol Aspects Med199718SupplS137S1449266515
- KjekshusJA statin in the treatment of heart failure? Controlled rosuvastatin multinational study in heart failure (CORONA): study design and baseline characteristicsEur J Heart Fail200571059106916227145
- TavazziLRationale and design of the GISSI heart failure trial: a large trial to assess the effects of n-3 polyunsaturated fatty acids and rosuvastatin in symptomatic congestive heart failureEur J Heart Fail2004663564115302013
- CoreshJPrevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination SurveyAm J Kidney Dis20034111212500213
- GoASChronic kidney disease and the risks of death, cardiovascular events, and hospitalizationN Engl J Med20043511296130515385656
- FriedLFEffect of lipid reduction on the progression of renal disease: a meta-analysisKidney Int20015926026911135079
- CollinsRMRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo controlled trialLancet20033612005201612814710
- KorenMJALLIANCE InvestigatorsFocused atorvastatin therapy in managed-care patients with coronary heart disease and CKDAm J Kidney Dis20095374175019216014
- SeverPSPrevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA): a multicentre randomized controlled trialLancet20033611149115812686036
- ColhounHMPrimary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trialLancet200436468569615325833
- SeverPSPrevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA): a multicentre randomized controlled trialLancet20033611149115812686036
- Stroke Prevention by Aggressive Reduction in Cholestrol Levels (SPARCL) InvestigatorsKaramJGHigh-dose atorvastatin after stroke or transient ischemic attackJ Cardiometab Syndr20083686918326981
- NissenS(REVERSAL) A prospective, randomized, double blind, multi-center study comparing the effects of atorvastatin vs pravastatin on the progression of coronary atherosclerotic lesions as measured by intravascular ultrasoundAmerican Heart Association Scientific Sessions 2003November 9–12, 2003Orlando, FloridaPlenary Session XI: Late Breaking Clinical Trials.
- NissenSEfor the ASTEROID InvestigatorsEffect of very high-intensity statin therapy on regression of coronary atherosclerosis: The ASTEROID trialJAMA20062951556156516533939
- PasceriVRandomized Trial of Atorvastatin for Reduction of Myocardial Damage during Angioplasty/Coronary Intervention (ARMYDA) TrialCirculation200411067467815277322
- PattiGAtorvastatin pretreatment improves outcomes in patients with acute coronary syndromes undergoing early percutaneous coronary intervention: results of the ARMYDA-ACS randomized trialJ Am Coll Cardiol2007491272127817394957
- HerrmannJPreprocedural statin medication reduces the extent of periprocedural non-Q-wave myocardial infarctionCirculation2002106172180218312390944