Abstract
The prognosis of patients with chronic heart failure (CHF) still remains poor, despite the recent advances in medical and surgical treatment. Furthermore, CHF is a major public health problem in most industrialized countries where the elderly population is rapidly increasing. Although the prevalence and mortality of CHF used to be relatively low in Japan, the disorder has been markedly increasing due to the rapid aging of the society and the Westernization of lifestyle that facilitates the development of coronary artery disease. The Chronic Heart Failure Analysis and Registry in the Tohoku District (CHART)-1 study was one of the largest cohorts in Japan. The study has clarified the characteristics and prognosis of Japanese patients with CHF, demonstrating that their prognosis was similarly poor compared with those in Western countries. However, we still need evidence for the prevention and treatment of CHF based on the large cohort studies or randomized treatment trials in the Japanese population. Since the strategy for CHF management is now changing from treatment to prevention, a larger-size prospective cohort, called the CHART-2 study, has been initiated to evaluate the risk factors of CHF in Japan. This review summarizes the current status of CHF studies in Japan and discusses their future perspectives.
Keywords:
Introduction
Chronic heart failure (CHF) is the leading cause of mortality in most developed countries (CitationHunt et al 2001). The prevalence and mortality rates of CHF used to be relatively lower in Japan compared with other Western countries. In Japan, approximately 1 to 2 million patients have CHF and nearly 170,000 patients die due to heart diseases each year (approximately 130 per 100,000 person-years) (CitationSummary of Vital Statistics 2005). However, the prevalence and death rates of cardiovascular diseases and CHF have been rapidly increasing in Japan, due to the Westernization of lifestyle, including dietary habits, and the aging population (The Status of Aging 2007). The Chronic Heart Failure Analysis and Registry in the Tohoku District (CHART)-1 study was one of the largest cohort studies with Japanese CHF patients (N = 1,278), which was designed to evaluate the characteristics and prognosis of those patients. We have also started a new cohort study, named the CHART-2 study (N = 10,000, expected) aiming to elucidate the effective preventive measures for CHF. This review briefly summarizes the major socio-medical issues of Japanese patients with CHF, their clinical characteristics and prognosis found in our CHART-1 study, and the current status of CHF studies in Japan.
Socio-medical status of Japanese patients with CHF
Rapid aging of Japanese population
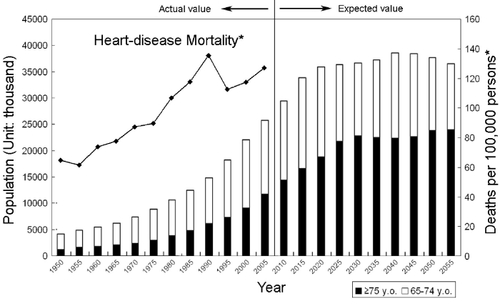
Until the 1980s, Japan had a lower percentage of elderly citizens compared with any other developed countries. However Japan is now one of the countries in which the population is aging rapidly. shows the time-course of aging and population projections between 1950 and 2055, which is assembled using the data reported by the Japanese Cabinet Office (The Status of Aging 2007). As of October 1, 2006, the total population of Japan was 127.8 million and the number of elderly aged 65 or older was 26.6 million, accounting for 21% of the total population. The elderly population is expected to continue to increase rapidly and the percentage of the elderly will reach 35.8 million (27%) in 2055 (The Status of Aging 2007). Life expectancy in Japan at birth has also drastically increased since World War II to 78.6 years for males and 85.5 years for females in 2005 (Life Expectancies at Specified Ages 2006). The Japanese Cabinet Office expects that it will reach 83.7 years for males and 90.3 years for female in 2055. Thus, in the near future, Japanese society will encounter more difficult medical problems due to rapid aging, which other developed countries have never before experienced.
Changing causes of death in Japan
Infectious diseases such as pneumonia, tuberculosis, and gastroenteritis were the leading causes of death in Japan until the mid 1900s. The major health problems in Japanese society have drastically changed since World War II. The morbidity and mortality rates of lifestyle-related diseases such as cancer, heart disease, stroke, and diabetes mellitus have dramatically increased. Approximately 60% of the mortality is now attributed to lifestyle-related diseases (cancer, 31%; ischemic heart disease 16%; cerebrovascular disease 13%; diabetes mellitus 1%; and hypertensive disease 0.6%) and the medical costs for these diseases amounts to 10.2 trillion yen (87.8 billion US dollars), accounting for approximately 30% of the total cost of the Japanese health insurance in 2003 (CitationExercise and Physical Activity Reference for Health Promotion 2006). Currently, heart disease is the second most frequent cause of death in Japan. shows the trend of the mortality due to heart diseases, which is constructed using the reports of death certificates in Japan (CitationSummary of Vital Statistics 2005). There is a clear trend for the increase in death due to heart disease since 1950s (there was a temporary sharp decline in 1995 due to the tenth revision of the International Classification of Diseases regarding the description of diagnosis in death certificates).
Health insurance system and future economic burden in Japan
In Japan, all citizens are enrolled in the mandatory health insurance system based on employment and residential status. The average number of visits to a doctor per year is 16 in Japan, versus 5.8 visits in the United States (CitationItoh 2004). As elderly patients tend to visit doctors more frequently and to have more medication or high-cost medical care, medical expenditure for the elderly is already taking one-third of the national health expenditure, and is projected to reach a half of the expenditure by the year 2025 (CitationItoh 2004). Progressive aging of the society and the consequent increase in the number of patients with CHF will cause more financial burden within Japanese society, which could lower the quality of medical services in the future.
An overview of heart failure studies in Japan
In Japan, medical treatment for patients with CHF is mainly based on the evidence obtained from randomized trials in the United States and Europe. There have been no sufficient randomized treatment trials or prospective cohort studies in Japan to clarify the real characteristics of Japanese patients with CHF or to improve their prognosis and quality of life. The mandatory health insurance system, the shortage of the budget to fulfill mega-trials, and the absence of trained research nurse system may all be responsible for the current situation. This section describes several cohort studies with Japanese CHF patients, major outcomes of the CHART-1 study, and randomized treatment trials for CHF performed with Japanese patients, either those that have already been published or are currently in progress. Finally, racial differences will be discussed, because this issue may also influence the impact of risk factors and/or the effects of treatments for CHF.
Prospective cohort studies in Japan
There are few multi-institutional prospective cohort studies with CHF patients in Japan (). The Chronic Heart Failure Analysis and Registry in the Tohoku District (CHART)-1 study was the first cohort study in Japan, including more than 1,000 Japanese patients with stable CHF, who were registered at 26 hospitals in the Tohoku district with a population of approximately 9.8 million (CitationShiba et al 2004). The CHART-1 study was initiated in February 2000 and was completed in December 2005. The total number of CHF patients enrolled was 1,278 and the mean follow-up period was 3.5 years. Details of design and the main outcome will be presented at the following part in this article. The Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD) is a registry of hospitalized patients with worsening CHF at 164 hospitals throughout the country between January 2004 and June 2005 (CitationTsutsui et al 2006). Death and hospital admission of the patients were followed through 2006 with the mean follow-up period of at least 1 year. Results of this study will appear in the near future. The Japanese Cardiac Registry of Heart Failure in General Practice (JCARE-GENERAL) is a registry of outpatients with CHF managed by cardiologists in hospitals and primary care physicians in general practice (CitationTsutsui et al 2007). Baseline data of totally 2,685 patients were collected during November 2004 and follow-up data were collected for 1 year after the enrolment. During the mean follow-up period of 427 days, the crude mortality rate was 6.7% in patients managed by cardiologists and 5.9% in those managed by general physicians. The Chronic Heart Failure Analysis and Registry in the Tohoku District (CHART)-2 study is currently the largest prospective and hospital-based cohort study with patients with CHF in Japan. This study was designed to investigate the characteristics and prognosis of a total of 10,000 patients with symptomatic CHF (Stage C/D in the ACC/AHA classification) and those with structural heart disease but without signs or symptoms of CHF (Stage-B in the AHA/ACC classification) (CitationHunt et al 2001). This study will elucidate the incidence and prognostic impact of metabolic syndrome in those patients, especially on the development of the first symptomatic CHF. The CHART-2 study was started in October 2006 and will be completed in September 2011.
Table 1 Multicenter prospective cohort study for patients with chronic heart failure in Japan
The CHART-1 Study
Risk stratification is the first line strategy to improve the prognosis and quality of life of patients with CHF. A number of factors have been found to correlate with the mortality of patients with CHF (CitationRector et al 1994; CitationDeedwania 2003; CitationBettencourt et al 2000). The CHART-1 study was started to register patients with stable CHF in February 2000 to clarify the characteristics and prognosis and to seek for prognostic factors in Japanese CHF patients (CitationShiba et al 2004, Citation2005). Patients were enrolled when at least one of the following criteria was met: (1) left ventricular ejection fraction (LVEF) <50%, (2) left ventricular end-diastolic dimension >55 mm, or (3) at least one episode of congestive heart failure. Patients less than 18 years old or those with clinically unstable conditions were excluded. Baseline data, including laboratory findings, results of echocardiography, and medical treatments for CHF, were recorded and annual surveillance was performed until the end of 2005.
Characteristics and prognosis of patients with CHF in Japan
A total of 1,278 patients were enrolled in the CHART-1 cohort. The mean age of the study population was 68.3 years, and male accounted for 66% of the total study population. The prevalence of diabetes mellitus and hypertension was 19% and 47%, respectively. Other baseline characteristics of patients are shown in . Ischemic etiology accounted for only 25% and the percentage of patients older than 65 years was 66%. Patients with preserved systolic function (defined as LVEF >50%) accounted for 45% of the total population. During the mean follow-up period of 3.5 years, all-cause mortality rate at 1-, 2-, and 3-year was 7%, 16%, and 22%, respectively (). Multivariate Cox analysis showed that several covariates, such as age, diabetes mellitus, ventricular tachycardia, serum level of B-type natriuretic peptide (BNP), rural residence, and NYHA functional class, were significantly associated with all-cause mortality (CitationShiba et al 2004). shows the Kaplan-Meier analyses of freedom from all-cause mortality in patients stratified by serum level of BNP or LVEF. Patients with higher BNP concentration had a significantly poorer prognosis (CitationWatanabe et al 2005), however, the prognostic impact was not significantly different between patients with 200–500 pg/mL of BNP level and those with >500 pg/mL (). The all-cause mortality of patients with preserved systolic function (LVEF > 50%) was not significantly different than that of patients with moderately decreased LVEF (30%–50%). However the prognosis of those with severely low LVEF (<30%) was the lowest with frequent episodes of sudden cardiac death (). The 3-year incidence of sudden death was higher in patients with LVEF <30% than those with LVEF ≥30% (15% vs 4%, respectively, p < 0.001). Primary prevention of sudden cardiac death with an implantable cardioverter defibrillator in those patients should be recommended when they meet the criteria in the authorized guidelines (CitationWatanabe et al 2006). Recently, anemia has been emphasized as an important prognostic predictor in patients with CHF (CitationEzekowitz et al 2003). Our data also showed that anemia was significantly associated with all-cause mortality, cardiac-cause mortality, and sudden death in patients with diastolic CHF (CitationTada et al 2007), as well as in those with systolic CHF, as reported by other researchers (CitationO’Meara et al 2006).
Figure 2 Prognosis of the Japanese patients with CHF in the CHART-1 study. Copyright © 2004. Reproduced with permission from CitationShiba N, Watanabe J, Shinozaki T, et al. 2004. Analysis of chronic heart failure registry in the Tohoku district: third year follow-up. Circ J, 68:427–34.
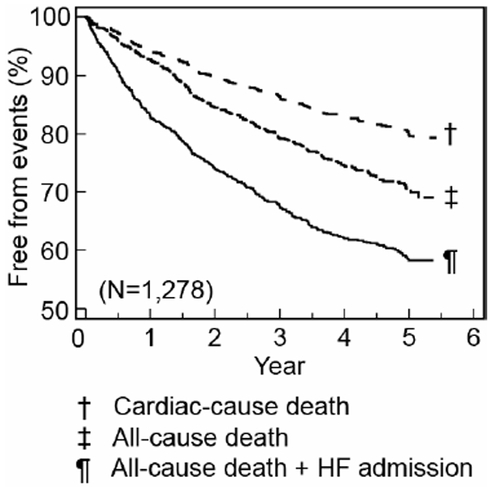
Figure 3 Kaplan-Meier curves of freedom from all-cause death stratified by (A) BNP and (B) LVEF in the CHART-1 study.
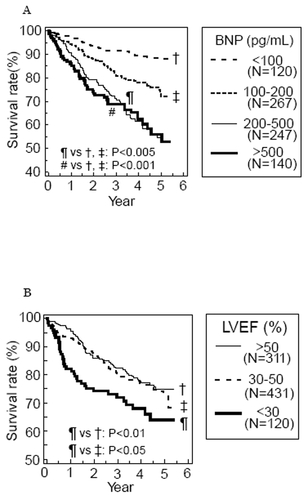
Table 2 Baseline characteristics of the Japanese patients in the CHART-1 study
Treatment of patients with CHF in Japan
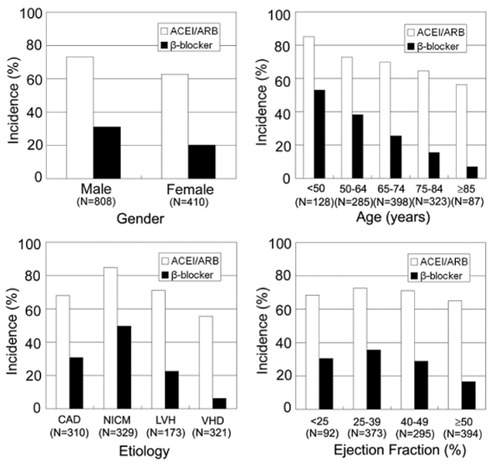
Treatments with angiotensin converting enzyme inhibitors (ACEI), angiotensin II receptor blockers (ARB), or β-blockers are recommended to improve prognosis and quality of life for patients with CHF (CitationHunt et al 2001). However it has previously been reported that such evidence-based treatments might not be sufficiently used in patients who should have had benefits of such medications (CitationMasoudi et al 2003). The overall usage rate of ACEI/ARB or β-blocker in patients enrolled in the CHART-1 study was 70% and 28%, respectively (). The penetration rate of these medications was relatively lower in female patients, elderly patients, and those with valvular heart disease or preserved LVEF, and this trend was more evident for the treatment with β-blocker than ACEI/ARB (). These results suggest that future clinical trials are still necessary for such minorities who have not usually been enrolled in major randomized treatment trials for CHF.
Figure 4 Prevalence of the use of renin-angiotensin inhibitors and β-blockers in the CHART-1 study. Copyright © 2007. Reproduced with permission from CitationShiba N, Takahashi J, Matsuki M. 2007. The CHART Study (Japanese). Naika, 99:410–14.
Clinical outcomes of Japanese patients with CHF
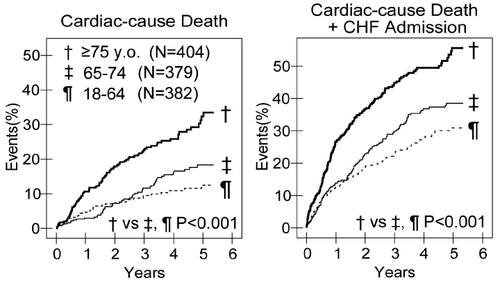
showed survival curves of placebo groups in randomized treatment trials for CHF performed in Western countries, superimposed with the result obtained in our CHART-1 study with Japanese CHF patients. One-year all-cause mortality of patients with mild-moderate CHF (NYHA II–IV and LVEF ≤40%) or moderate-severe CHF (NYHA III–IV and LVEF ≤35%) was 13% and 21%, respectively. Importantly, as is evident in , the prognosis of Japanese patients with CHF was equally poor compared with Western CHF patients. Since the Japanese society is aging rapidly, a sharp increase in the number of CHF patients will be inevitable in the near future in Japan, as CHF is a disease of the elderly. shows the event rate in CHF patients based on age at the entry, demonstrating that elderly Japanese patients with CHF had an increased incidence of cardiac death and a combination of cardiac death and admission due to congestive CHF. This is because elderly CHF patients have a higher rate of combined risk factors, such as anemia, chronic kidney disease, hypertension, and atrial fibrillation. Appropriate prevention strategies against the development and progression of CHF should be undertaken in Japan.
Figure 5 Comparison of the prognosis of patients with CHF between Western clinical trials and the CHART-1 study. Copyright © 2007. Reproduced with permission from CitationShiba N, Takahashi J, Matsuki M. 2007. The CHART Study (Japanese). Naika, 99:410–14.
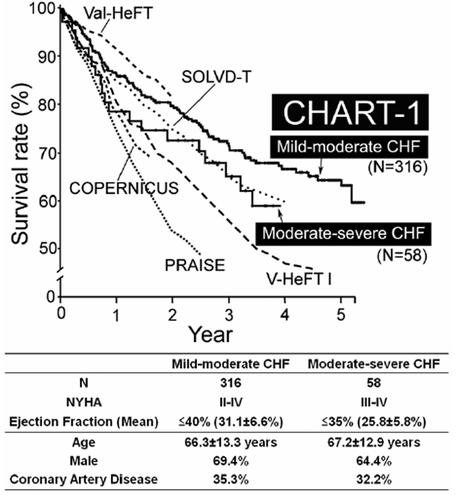
Figure 6 Prognosis of elderly patients with CHF in the CHART-1 study. Copyright © 2007. Reproduced with permission from CitationShiba N, Takahashi J, Matsuki M. 2007. The CHART Study (Japanese). Naika, 99:410–14.
Major CHF treatment trials in Japan
There are 2 published randomized treatment trials for CHF patients in Japan (). The Multicenter Carvedilol Heart Failure Dose Assessment (MUCHA) trial enrolled 174 patients with mild to moderate CHF to seek for the efficacy and optimum dose of carvedilol, with 3 treatment arms, including placebo, 5 and 20 mg of the β-blocker in daily dose (CitationHori et al 2004). During the 24–48 weeks of the treatment period, carvedilol achieved dose-related improvement of the rate of death or cardiovascular hospitalization to 25%, 9%, and 5% in the placebo, 5 mg, and 20 mg group, respectively (p = 0.002). The Assessment of Response to Candesartan in Heart Failure in Japan (ARCH-J) study investigated the efficacy of candesartan (8 mg once daily) in comparison with the placebo in 305 patients with symptomatic CHF (CitationMatsumori et al 2003). During the 6-month follow-up period, fatal cardiovascular events occurred in 2 patients in each treatment group and the incidence of progression of CHF was 7% and 22% in the candesartan and the placebo group, respectively (p = 0.0004).
Table 3 3 Multicenter randomized clinlical trials for patients with chronic heart failure in Japan
We have recently initiated a large outcome study with olmesartan in CHF patients, termed The Supplemental Benefit of Angiotensin II Receptor Blocker in Hypertensive Patients with Stable Heart Failure Using Olmesartan (SUPPORT trial), which is currently the largest outcome study in Japan (). The purpose of our SUPPORT trial is to examine whether an ARB, olmesartan, in addition to conventional treatment, reduces the mortality and morbidity of hypertensive patients with stable CHF. The primary endpoint is a combined event of all-cause death, nonfatal acute myocardial infarction, nonfatal stroke, and hospital admission due to congestive heart failure. We also aim to evaluate the beneficial effect of olmesartan on the progression of metabolic syndrome. The entry of patients was started in November 2007, and the results of the study will be obtained by the end of 2011.
There are 5 other small outcome trials that are currently in progress in Japan (). The Assessment of Beta-Blocker Treatment in Japanese Patients with Chronic Heart Failure (J-CHF) and the Japanese Diastolic Heart Failure Study (J-DHF) are investigating the effects of carvedilol in patients with systolic CHF and those with diastolic CHF, respectively. Another objective of J-CHF is to determine the optimum dose of carvedilol and to elucidate the differences in clinical characteristics between responders and nonresponders to the β-blocker. The Pitavastatin Heart Failure Study (PEARL study) is designed to evaluate the efficacy of pitavastatin for CHF with mild hypercholesterolemia. The Japanese Multicenter Evaluation of Long- versus short-acting Diuretics in Congestive Heart Failure (J-MELODIC) is designed to compare the effects of furosemide and azosemide in patients with CHF and to test the hypothesis that long-acting diuretics are superior to short-acting ones in those patients. The Japanese Heart Failure Outpatients Disease Management and Cardiac Evaluation Study (J-HOMECARE) was designed to evaluate the benefit of disease management program for prognosis, psychological status and quality of life of patients with CHF.
There are 2 large trials that have investigated the role of valsartan in Japanese patients with cardiovascular disease including CHF (). The Japanese Investigation of Kinetic Evaluation in Hypertensive Event and Remodeling Treatment (JIKEI-HEART) Study was designed to investigate whether concomitant treatment with valsartan in addition to conventional treatment improves the prognosis of Japanese patients with hypertension, ischemic heart disease, or congestive heart failure. The results of this study have recently been published (CitationMochizuki et al 2007). After a median follow-up period of 3.1 years, the incidences of stroke, transient ischemic attack, angina pectoris, and CHF were significantly lower in patients treated with valsartan compared with those with the conventional treatment. However, the benefit of the add-on valsartan treatment in a sub-population with CHF, which accounted for 11% of the total population, has not been published yet. The Add-on Effects of Valsartan on Morbi-Mortality (KYOTO-HEART) study was designed to assess the add-on effect of valsartan on the conventional treatment in terms of the morbidity and mortality in Japanese hypertensive patients with high risks of cardiovascular diseases including CHF ().
Table 4 Multicenter randomized clinlical trials for patients with cardiovascular risks including CHF in Japan
Many of the randomized clinical trials performed in Japan utilize the prospective randomized open blinded endpoint (PROBE) design, as an alternative to the randomized double-blind placebo-controlled design ( and ). This is mainly because the PROBE study tends to be more cost effective and its open-labeled medication may minimize ethical considerations (CitationHansson et al 1992).
Racial difference in morbidity and mortality due to cardiovascular diseases
Several researchers have suggested that cardiovascular risk factors have different prognostic impact among different populations. The Seven Countries Study Research Group showed a substantial heterogeneity among populations in terms of the death rate due to coronary artery disease, even at a similar level of blood pressure (CitationVan den Hoogen et al 2000). The proportion of deaths attributable to cardiovascular disease has also been reported to vary among different cohorts even at the similar serum cholesterol level. The long-term follow-up for 25 years for 12,763 men in 16 cohorts in Europe, the United States, and Japan showed that the risk factors of cardiovascular disease, such as insufficient physical activity and high serum cholesterol level, were not significantly associated with all-cause death in several countries including Japan (CitationMenotti et al 2001). Since these differences cannot be explained by other baseline characteristics, smoking habits, or genetic difference, environmental and/or behavioral factors may play an important role in the development of cardiovascular diseases. The Ni-Hon-San Study, which compared cardiovascular disease rates and risk factors in Japanese men living in Japan, Hawaii, and California, showed that the mortality rate due to coronary artery disease was lowest in Japanese men living in Japan, whereas it was highest in those living in California (CitationBenfante 1992). Racial differences may also influence the effect of medical treatment for CHF. Several studies demonstrated that genetic polymorphisms and/or a difference in β1-receptor sensitivity, which are frequently observed in the Japanese population, might change the pharmacokinetics or the clinical effect of medical drugs, such as ACEI and β-blockers (CitationKubota et al 2000; CitationXie et al 2001; CitationRanade et al 2002).
Future direction for the management of CHF in Japan
CHF is a slowly progressive disease from stage A to stage D unless appropriately treated as described in the ACC/AHA guidelines (CitationHunt et al 2001). The strategy to manage CHF has been changing recently from treatment to prevention (CitationBansal et al 2006). Japanese CHF patients have several different profiles compared with Western CHF patients as follows; (a) the prevalence of CHF of ischemic origin is lower, (b) the percentage of elderly population is remarkably high, and (c) the penetration rate of evidence-based medicine, such as ACEI/ARB or β-blockers, is not sufficiently high yet. The current situation of the management of CHF in Japan is probably caused by the fact that the number of randomized treatment trials for Japanese patients is not enough yet. Given the expected future increase in Japanese patients with CHF, effective prevention strategy is necessary. Our on-going CHART-2 and SUPPORT studies will enable us to obtain effective strategies to improve the management of CHF in Japan.
Conclusions
The prevalence of CHF will rapidly increase in the next decades in many industrialized countries, including Japan. Large cohort studies with CHF patients are useful for risk stratification and determination of preventive measures for the disorder. Large-scale, randomized treatment trials also are needed, especially in Japan, in order to obtain further evidence to improve the management of patients with CHF.
Acknowledgements
Active investigators of the CHART studies were described in the paper previously published (CitationShiba et al 2004) and at the website of the Tohoku Heart Failure Association (see http://tohoku.cardiovascular-medicine.jp). The CHART-1 study was supported by the research grants from the Ministry of Health, Labor and Welfare and Gonryo Medical Foundation. We are grateful for the assistance of research nurses who are working at the Tohoku Heart Failure Association; Mika Matsuki, Shizuka Osaki, Kiriko Yukishita, Yuuko Kidoguchi, Miho Hotta, Haruka Kohno, and Keiko Nishiura.
References
- BansalDChahoudGSmithESPrevention of heart failureCurr Opin Cardiol2006215101616900016
- BenfanteRStudies of cardiovascular disease and cause-specific mortality trends in Japanese-American men living in Hawaii and risk factor comparisons with other Japanese populations in the Pacific region: a reviewHum Biol1992647918051427739
- BettencourtPFerreiraADiasPPredictors of prognosis in patients with stable mild to moderate heart failureJ Card Fail200063061311145755
- DeedwaniaPCThe key to unraveling the mystery of mortality in heart failure: An integrated approachCirculation200310717192112682028
- Exercise and Physical Activity Reference for Health Promotion 2006Office for Lifestyle-related Diseases Control, General Affairs Division, Health Service Bureau, Ministry of Health, Labour Welfare [online] Accessed on June 10, 2007. URL: http://www.nih.go.jp/eiken/english/research/program_exercise_epar2006.html
- EzekowitzJAMcAlisterFAArmstrongPWAnemia is common in heart failure and is associated with poor outcomes: insights from a cohort of 12 065 patients with new-onset heart failureCirculation2003107223512538418
- HanssonLHednerTDahlofBProspective randomized open blinded end-point (PROBE) study. A novel design for intervention trialsBlood Press19921113191366259
- HoriMSasayamaSKitabatakeALow-dose carvedilol improves left ventricular function and reduces cardiovascular hospitalization in Japanese patients with chronic heart failure: the Multicenter Carvedilol Heart Failure Dose Assessment (MUCHA) trialAm Heart J20041473243014760332
- HuntSABakerDWChinMHACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: Executive summaryJ Am Coll Cardiol20013821011311738322
- ItoMHealth Insurance Systems in Japan: a Neurosurgeon’s ViewNeurol Med Chir (Tokyo)2004446172815684593
- KubotaTYamamuraYOhkawaNFrequencies of CYP2D6 mutant alleles in a normal Japanese population and metabolic activity of dextromethorphan O-demethylation in different CYP2D6 genotypesBr J Clin Pharmacol20005031410886115
- Life Expectancies at Specified AgesAbridged Life Tables For Japan 2006, Ministry of Health, Labour and Welfare [online] Accessed on June 10, 2007. URL: http://www.mhlw.go.jp/english/database/db-hw/lifetb06/1.html
- MasoudiFAHavranekEPWolfePMost hospitalized older persons do not meet the enrollment criteria for clinical trials in heart failureAm Heart J2003146250712891192
- MatsumoriAARCH-J study investigatorsEfficacy and safety of oral candesartan cilexetil in patients with congestive heart failureEur J Heart Fail200356697714607207
- MenottiABlackburnHKromhoutDCardiovascular Risk Factors as Determinants of 25-year All-cause Mortality in the Seven Countries StudyEur J Epidemiol2001173374611767959
- MochizukiSDahlöfBShimizuMValsartan in a Japanese population with hypertension and other cardiovascular disease (Jikei Heart Study): a randomised, open-label, blinded endpoint morbidity-mortality studyLancet20073691431917467513
- O’MearaEClaytonTMcEntegartMBClinical correlates and consequences of anemia in a broad spectrum of patients with heart failure: results of the Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity (CHARM) ProgramCirculation20061139869416476847
- RanadeKJorgensonESheuWHHA polymorphism in the beta-1 adrenergic receptor is associated with resting heart rateAm J Hum Genet2002709354211854867
- RectorTSCohnJNPrognosis in congestive heart failureAnnu Rev Med199445341508198388
- ShibaNWatanabeJShinozakiTAnalysis of chronic heart failure registry in the Tohoku district: third year follow-upCirc J2004684273415118283
- ShibaNWatanabeJShinozakiTPoor prognosis of Japanese patients with chronic heart failure following myocardial infarction – comparison with nonischemic cardiomyopathyCirc J200569143915671603
- ShibaNTakahashiJMatsukiMThe CHART Study (Japanese)Naika20079941014
- Summary of Vital StatisticsSummary of Vital Statistics. Ministry of Health, Labour and Welfare [online]2005 Accessed on July 6, 2007. URL: http://www.mhlw.go.jp/english/database/db-hw/populate/index.html
- TadaTShibaNWatanabeJPrognostic value of anemia in predicting sudden death of patients with diastolic heart failureInt J Cardiol2007In Press
- The Status of Aging and Implementation of Measures for Aging Society in FY 2005Annual Report on the Aging Society 2007, Cabinet Office [online] Accessed on June 10, 2007. URL: http://www.cao.go.jp/index-e.html
- TsutsuiHTsuchihashi-MakayaMKinugawaSClinical characteristics and outcome of hospitalized patients with heart failure in Japan. –Rationale and design of Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD)-Circ J20067016172317127810
- TsutsuiHTsuchihashi-MakayaMKinugawaSCharacteristics and outcomes of patients with heart failure in general practices and hospitals. –Japanese Cardiac Registry of Heart Failure in General Practice (JCARE-GENERAL)Circ J2007714495417384441
- Van den HoogenPFeskensEJMNagelkerkeNJDThe Relation between Blood Pressure and Mortality due to Coronary Heart Disease among Men in Different Parts of The WorldN Engl J Med20003421810620642
- WatanabeJShibaNShinozakiTPrognostic value of plasma brain natriuretic peptide combined with left ventricular dimensions in predicting sudden death of patients with chronic heart failureJ Card Fail20051150515704064
- WatanabeJShinozakiTShibaNAccumulation of risk markers predicts the incidence of sudden death in patients with chronic heart failureEur J Heart Fail200682374216185924
- XieHGKimRBWoodAJJMolecular basis of ethnic differences in drug disposition and responseAnnu Rev Pharmacol Toxicol2001418155011264478