Abstract
Background
The role of transesophageal echocardiography (TEE) in the evaluation of acute stroke patients is still ill-defined. We conducted a prospective observational study to find the prevalence of TEE findings that indicate anticoagulation as beneficial, in acute ischemic stroke patients without indication for anticoagulation based on clinical, electrocardiographic and transthoracic echocardiography (TTE) findings.
Methods
We prospectively studied all patients referred to our laboratory for TTE and TEE. Patients were excluded if the diagnosis was not acute ischemic stroke or if they had an indication for anticoagulation based on clinical, electrocardiographic, or TTE data. Patients with TEE findings that might indicate anticoagulation as beneficial were identified.
Results
A total of 84 patients with acute ischemic stroke and without indication for anticoagulation based on clinical and electrocardiographic or TTE data were included in the study. Findings indicating anticoagulation as beneficial were found in 32.1%: spontaneous echo contrast (1.2%), complex aortic atheroma (27.4%), thrombus (8.3%), and simultaneous patent foramen ovale and atrial septal aneurysm (2.4%).
Conclusions
The results of our study show that TEE can have therapy implications in 32.1% of ischemic stroke patients in sinus rhythm and with TTE with no indication for anticoagulation.
Introduction
The role of transesophageal echocardiography (TEE) in the evaluation of acute stroke patients is still ill-defined (CitationAdams et al 2003; CitationHack et al 2003).
While some studies conclude that TEE should be mandatory on all ischemic stroke patients, based on its cost-effectiveness (CitationMcNamara et al 1997) and sensitivity for findings that change clinical management (coumadin instead of aspirin) (CitationBlum et al 2004), others find that TEE abnormalities are found mostly in patients already with clinical, electrocardiographic or transthoracic echocardiography (TTE) data that would justify anticoagulation, and are rare in patients with sinus rhythm and with a normal TTE (CitationLeung et al 1995; CitationCabral et al 2001; CitationAgmom and Khandheria 2002). As a consequence, the usefulness of TEE findings for the clinical management of ischemic stroke patients has been challenged, but not defined, with some authors defending TEE only on patients with abnormal TTE (CitationLeung et al 1995), with a normal TTE (CitationNighoghossian 1995), on an individual patient basis (CitationCabral et al 2001), or questioning its usefulness in the management of any ischemic stroke patient (CitationWarner and Momah 1996).
The aim of our study was to find the prevalence of TEE findings that indicate anticoagulation as beneficial, in acute ischemic stroke patients without indication for anticoagulation based on clinical, electrocardiographic, and TTE findings.
Methods
This was a prospective observational study, carried out from April 13, 2004 to October 11, 2005. The study was approved by our hospital ethics committee. Informed consent was obtained from all patients.
Patients
All patients referred to our laboratory simultaneously for TEE and TTE were enrolled in the study. Patients were excluded if the diagnosis was not acute ischemic stroke, or if they had an indication for anticoagulation based on clinical and electrocardiographic or TTE data.
The diagnosis of stroke was made by the referring physicians, based on clinical data and brain CT.
Echography
All the echographic studies were performed by the authors, on a Vivid 3 System, General Electric.
Transthoracic echocardiography was performed using a 2.5-MHz transducer for M-mode, 2D, and Doppler, according to the recommendations of the American Echocardiography Society (CitationHenry et al 1980).
Transesophageal echocardiography was performed using a multiplane 3.5 to 6.5 MHz probe, according to standard protocols (CitationSeward et al 1988). The presence of the following potential sources of embolism was specifically examined: (a) left atrial spontaneous echo contrast and thrombus; (b) atheroma in the thoracic aorta; (c) patent foramen ovale and atrial septal aneurysm; and (d) others, including valvular vegetations and intracardiac masses. Left atrial spontaneous echo contrast was diagnosed by the presence of characteristic dynamic smokelike swirling echo in the left atrium or the atrial appendage, distinct from background white noise due to excessive gain (CitationBlack et al 1991). Left atrial thrombus was diagnosed by the presence of an echodense mass in the left atrium or the left atrial appendage, distinct from the endocardium and the pectinate muscles of the left atrial appendage (CitationBeppu et al 1984). The presence of atheroma in the thoracic aorta was examined. Atheroma that were mobile, pedunculated, or protruding ≥5 mm into the lumen were classified as complex atheroma (CitationKaralis et al 1985; CitationKatz et al 1992). All other sessile atheroma <5 mm in thickness were classified as simple atheroma. The interatrial septum was examined for patent foramen ovale, atrial septal defect, and atrial septal aneurysm. Color doppler, without and with Valsalva manoeuvre, and bubble contrast study with agitated saline, also without and with Valsalva manoeuvre, were performed in all patients to look for interatrial shunting. Bubbles appearing in the left atrium within three cardiac cycles or observed traversing the interatrial septum constituted a positive study for shunting. Atrial septal aneurysm was defined as a thin-walled area in the region of the fossa ovalis with a base of at least 1.5 cm and an excursion with the cardiac cycle of at least 1.5 cm (CitationHanley et al 1985). Care was taken to distinguish a true atrial septal aneurysm from a hypermobile interatrial septum.
Indications for anticoagulation
TTE findings that were considered to indicate anticoagulation as beneficial (CitationTribolet de Abreu et al 2005) were defined as: mitral valve stenosis with an enlarged (>55 mm) left atria, valve prosthesis, left ventricular systolic dysfunction (with an estimated ejection fraction <35%), dilated cardiopathy, previous myocardial infarction (with left ventricular wall dyskinesis), left atria or left ventricle masses.
TEE findings that were considered to indicate anticoagulation as beneficial were defined as: left atrial spontaneous echo contrast and thrombus (CitationBlum et al 2004), complex aortic atheroma (CitationAmarenco et al 1994; CitationJones et al 1995), simultaneous patent foramen ovale and atrial septal aneurysm (CitationMas et al 2001; CitationKizer et al 2005), thrombus on any heart chamber, valve, or the aorta.
Statistical analysis
The program Statistical Package for the Social Sciences version 12.0 for Windows was used as a database.
Results
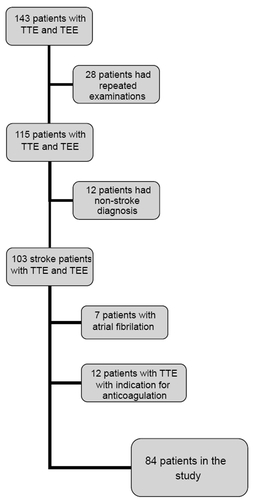
During the study period, 143 patients were sent to our laboratory for both TTE and TEE. In addition to 28 repeated examinations, a total of 31 patients were excluded for nonstroke diagnosis and for indications of anticoagulation before the performance of transesophageal echocardiography (), leaving 84 patients included in the study.
The baseline characteristics and risk factors of the study patients are shown in .
Table 1 Baseline characteristics and risk factors of the study patients
A total of 27 (32.1%) patients had TEE findings that might indicate anticoagulation as beneficial (), three of which had more than one finding (left atrial spontaneous echo contrast and complex aortic atheroma [1 patient], thrombus in the aortic artery wall and complex aortic atheroma [2 patients]).
Table 2 Transesophageal echocardiography findings indicating anticoagulation as beneficial
Of the 7 patients with thrombus, 4 had thrombus in the aortic valve leaflets, and three patients had thrombus in the aortic artery wall.
Discussion
In our study, TEE had findings that might indicate anticoagulation as beneficial in 32.1% of our population of ischemic stroke patients, without other indications for anticoagulation by clinical, electrocardiographic or TTE data.
We found seven similar published studies (CitationLeung et al 1995; CitationWarner and Momah 1996; CitationPalazzuoli 2000; CitationCabral et al 2001; CitationTatani 2001; CitationWard 2006; CitationHarloff 2006; ). Only one of them was prospective (CitationHarloff 2006), three included patients without a previous TTE (CitationWarner and Momah 1996; CitationPalazzuoli 2000; CitationTatani 2001), and two included patients with atrial fibrilation (CitationWarner and Momah 1996; CitationHarloff 2006). Only two of the studies specified the number of patients who had simultaneous patent foramen ovale and atrial septal aneurysm (CitationTatani 2001; CitationHarloff 2006). This fact is relevant, since anticoagulation is considered beneficial only in patients with both these abnormalities (CitationMas et al 2001; CitationKizer et al 2005).
Table 3 Transesophageal findings in ischemic stroke patients
The most recent of these studies, by CitationHarloff and colleagues (2006), was a prospective study in which TEE was performed on 503 out of 564 consecutive ischemic stroke patients, including patients excluded from our study, such as patients already with indications for anticoagulation, as atrial fibrilation and other types of cardioembolic stroke, and patients with contraindications against oral anticoagulation. They found spontaneous echo contrast in 11.5%, complex aortic atheroma in 19.7%, thrombus in 7.2% and simultaneous patent foramen ovale and atrial septal aneurysm in 9%. They concluded that “TEE is indispensable in all patients being candidates for oral anticoagulation”.
Our study patients were a selected group who were referred for TEE by the attending physician. During our study, a total of 855 patients were admitted to our hospital with a diagnosis of stroke (ischemic or hemorrhagic) or transient ischemic attack. Even if we consider 15% of these patients to have had an hemorrhagic stroke, the 143 patients in our study would represent approximately 20% of the remaining 727 patients. We cannot compensate for this bias.
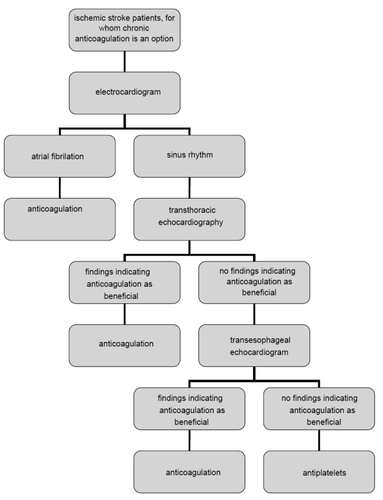
Several TEE findings that might indicate anticoagulation as beneficial for secondary prophylaxis in ischemic stroke patients have been identified (CitationAmarenco et al 1994; CitationJones et al 1995; CitationMas et al 2001; CitationBlum et al 2004; CitationKizer et al 2005). The superiority of TEE over TTE for diagnosing these abnormalities has also been demonstrated (CitationMcNamara et al 1997; CitationBlum et al 2004), and confirmed in our study. The prevalence of these abnormalities in a large unselected population of consecutive ischemic stroke patients has recently been studied by CitationHarloff and colleagues (2006). Our results seem to confirm their findings, but on a more selected population of patients with no other indication for anticoagulation. Based on our study and on the study by Harloff and colleagues, we propose an algorithm for the use of ultrasonographic studies on ischemic stroke patients without contraindications for long term anticoagulation ().
The results of our study show that TEE can have therapy implications in 32.1% of ischemic stroke patients in sinus rhythm and with a previous TTE with no indication for anticoagulation.
References
- AdamsHPJrAdamsRJBrottTStroke Council of the American Stroke AssociationGuidelines for the early management of patients with ischemic stroke: a scientific statement from the Stroke Council of the American Stroke AssociationStroke20033410568312677087
- AgmomYKhandheriaBJGentileFClinical and echocardiographic characteristics of patients with left atrial thrombus and sinus rhythmCirculation2002105273111772872
- AmarencoPCohenATzourioCAtherosclerotic disease of the aortic arch and the risk of ischemic strokeN Engl J Med1994331147497969297
- BeppuSParkYDSakakibaraHClinical features of intracardiac thrombosis based on echocardiographic observationJpn Circ J19844875826694334
- BlackIWHopkinsAPLeeLCLeft atrial spontaneous echo contrast: a clinical and echocardiographic analysisJ Am Coll Cardiol1991183984041856407
- BlumAReisnerSFarbsteinYTransesophageal echocardiography vs. transthoracic echocardiography in assessing cardio-vascular sources of emboli in patients with acute ischemic strokeMed Sci Monit200410CR521315328485
- CabralSOliveiraFPereiraSTransesophageal echocardiography in the assessment of patients presenting with ischemic cerebral events without previous evidence of a cardiac source of emboliRev Port Cardiol2001202475811417308
- HackWKasteMBogousslavskiJEuropean Stroke Initiative Executive Comittee and the EUSI Writing ComitteeEuropean Stroke Initiative Recommendations for Stroke Management: update 2003Cerebrovasc Dis2003163113714584488
- HanleyPCTajikAJHynesJKDiagnosis and classification of atrial septal aneurism by two-dimensional echocardiography: report of 80 consecutive casesJ Am Coll Cardiol198561370824067118
- HarloffAHandkeMReinhardMTherapeutic strategies after examination by transesophageal echocardiography in 503 patients with ischemic strokeStroke2006378596416439702
- HenryWLDeMariaAGramiakRReport of the American Echocardiography Society Committee on Nomenclature and Standards in Two-Dimensional EchocardiographyCirculation198062212157397962
- JonesEFKalmanJMCalafiorePProximal aortic atheroma: an independent risk factor for cerebral ischemiaStroke199526218247831691
- KaralisDGChandrasekaranKVictorMFRecognition and embolic potential of intraaortic atherosclerotic debrisJ Am Coll Cardiol1985177381987243
- KatzESTunickPARusinekHProtruding aortic atheromas predict stroke in elderly patients indergoing cardiopulmonary bypass: experience with intraoperative transesophageal echocardiographyJ Am Coll Cardiol1992207071607541
- KizerJRDevereuxRBPatent foramen ovale in young adults with unexplained strokeN Engl J Med200535323617216319385
- LeungDYBlackIWCranneyGBSelection of patients for transesophageal echocardiography after stroke and systemic embolic events: role of transthoracic echocardiographyStroke199526182047570732
- MasJ-LArquizanCLamyCRecurrent cerebrovascular events associated with patent foramen ovale, atrial septal aneurysm, or bothN Engl J Med20013451740611742048
- McNamaraRLLimaJACWheltonPKEchocardiographic identification of cardiovascular sources of emboli to guide clinical management of stroke: a cost-effectiveness analysisAnn Intern Med1997127775879382398
- NighoghossianNPerinettiMBartheletMTransesophageal echocardiography in patients less than 60 years of age without obvious cardiac souce of embolismNeurol Res199517368728584128
- PalazzuoliARicciDLenziCTransesophageal echocardiography for identifying potential cardiac sources of embolism in patients with strokeNeurol Sci20002119520211214657
- SewardJBKhandheriaBKOhJKTransesophageal echocardiography: technique, anatomic correlations, implementation and clinical applicationsMayo Clin Proc198863649803290590
- TataniSBFukujimaMMLimaJACClinical impact of transesophageal echocardiography in patients with stroke without clinical evidence of cardiovascular sources of emboliArq Bras Cardiol20017645861
- Tribolet de AbreuTMateusSCorreiaJTherapy implications of transthoracic echocardiography in acute ischemic stroke patientsStroke2005361565615947277
- WardRPDonCWFurlongKTPredictors of long-term mortality in patients with ischemic stroke referred for transesophageal echocardiographyStroke200637204816339470
- WarnerMFMomahKIRoutine transesophageal echocardiography for cerebral ischemia. Is it really necessary?Arch Intern Med19961561719238694671