Abstract
The study was conducted to evaluate the clinical and angiographic results of the implantation of the paclitaxel-eluting stent Meo:DrugStar ST in patients with symptomatic coronary artery disease. The Meo:DrugStar ST stent has a stainless steel stent platform with a homogenous non-biodegradable coating of paclitaxel mixed with a polyether-based biostable, monophase, and hemocompatible coating. Sixty patients with native coronary artery disease were included in the study. The Meo:DrugStar ST stents were implanted in 60 de novo lesions detected in these patients. Immediate and long-term clinical and angiographic follow-up results were evaluated. There was a high proportion of patients with hypertension (55%) according to JNC-VII. Mean stenosis ratio was 78 ± 13 %, mean implanted stent diameter was 3.0 ± 0.4 mm and mean length was 22 ± 5 mm. Restenosis was detected in 4 (10%) of those patients and 11 (27.5%) of 40 patients had insignificant amount of restenosis. The results of this study indicate a potential benefit of the Meo:DrugStar ST stent for the prevention of stent thrombosis and restenosis in these relatively high-risk patients.
The development and widespread use of coronary stents has probably been the single most significant advance in the field of interventional cardiology over the last decade. The use of a stent at the time of coronary artery dilatation is now carried out in more than 70% of all intra-coronary angioplasty procedures and, in many ways, coronary angioplasty has become coronary stenting. Its exact role is still being debated and there is a proliferation of stent designs, stent technologies, and stent coatings which continue to challenge the interventional cardiologist to try and utilize them to their best ability. The increased cost of stenting represents financial challenges that have been taken up to a greater or lesser extent in different health-care systems and countries (CitationSerruys et al 1994).
A breakthrough occurred in early 2000 with the development of stents that eluted pharmacology agents directly into the vessel wall by means of a controlled release from a durable polymer coating. Various drug-eluting stents (DES) were developed, each varying in delivery platform, polymer coating (or absence of coating), and drug selected for elution (CitationPompa and Tulli 2006).
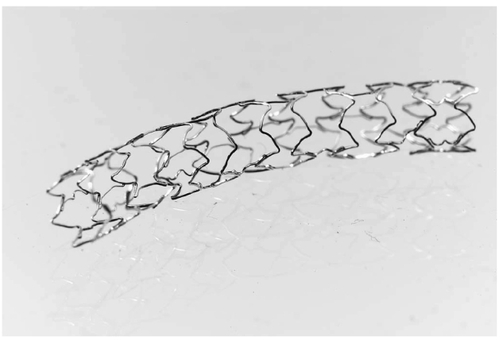
The paclitaxel eluting stent (Meo:DrugStar ST, Germany) is a new DES. It has a stainless steel stent platform and a homogenous non-biodegradable coating of paclitaxel mixed with a polyether-based biostable, monophase, and hemocompatible coating. Paclitaxel release is completed within 28 days of implantation (). This article describes the immediate and long-term clinical and angiographic results following implantation of the paxlitacel-eluting stent Meo:DrugStar ST.
The CYPHER® stent (Cordis Corporation, Miami Lakes, FL, USA) is composed of balloon-expandable stainless steel, a durable copolymer mixture of polyethylene-covinyl acetate (PEVA) and poly-n-butyl methacrylate (PBMA), and a sirolimus, which is a G1 cell cycle inhibitor that also has potent anti-inflammatory properties. Using the commercially available, slow-release polymer formulation, 90% of the sirolimus contained on the stent is released within 30 days (CitationMoses et al 2003). The CYPHER stent was approved for clinical use in Europe in April 2002 and in the United States in May 2003. This stent is used in approximately 50% of DES procedures worldwide.
Material and methods
Patients
Sixty patients were eligible for enrolment if there was symptomatic coronary artery disease or positive functional testing and angiographic evidence of single- or multi-vessel disease with a target lesion stenosis of ≥75% in a ≥2.5 mm vessel. Patients were excluded if there was left main disease (≥50%), recent myocardial infarction (MI), (≤7 days), contraindications to anti-platelet therapy, or a need for ≥3 stents for 1 target site. Every patient signed an informed consent.
Stent description and implantation
Meo:DrugStar ST is a commercially available stainless steel, paclitaxel-coated stent produced in different sizes. Before stenting, all patients were administered clopidogrel 75 mg/day for 4 days. Procedures were performed using the standard angioplasty technique with a 7 and 8 French (Fr) guiding catheter via the femoral approach. A bolus of 100 IU/kg of heparin was administered intra-arterially after insertion of the vascular access sheath. Target lesions were initially treated with appropriate balloon dilatation. The reference diameter of target vessel was estimated visually, and stent size was determined based on a stent-to-artery ratio of 1.1:1 to 1.2:1. The stents were deployed at 8–14 atmospheres (atm) and high-pressure balloon inflation (to 14 atm) was then applied with a non-compliant short balloon to avoid distal dissection.
Post-procedure medication protocol and medication and follow-up
After successful stent implantation, heparin was not routinely administered unless there was a clinical indication, such as large residual dissection. Femoral sheaths were removed 2 hours after the procedure. Aspirin 100–300 mg once daily and clopidogrel 75 mg once daily were continued 6 months. Electrocardiograms (ECGs) were recorded immediately after the procedures, then daily before discharge. If the patient had recurrent chest pain after the procedure, troponin T and CK-MB levels were measured and an additional ECG was recorded. The majority of patients were discharged 2 days after the procedure. Follow-up coronary angiography was performed at 6 months.
Angiographic analysis
Quantitative coronary angiographic analysis was performed using the quantitative coronary analysis system (Acom. PC Lite version 2.0 Siemens München, Germany) at the Coronary Angiography Laboratory of the Cardiology Department of Izzet Baysal Medical Faculty of Abant Izzet Baysal University. Angiographic measurements were obtained during end-diastole using the image that showed the greatest narrowing, without overlap and with the least degree of foreshortening. Measurements of the reference vessel diameter, minimal lumen diameter (MLD), and percent diameter stenosis were determined by the average of two orthogonal views. The index reference diameter was the average of proximal and distal reference vessel diameters. Lesion length was measured on the baseline angiography using the “shoulder-to-shoulder” definition. Lesions were characterized according to the modified American College of Cardiology/American Heart Association (ACC/AHA) classification. Changes in MLD were expressed as acute gain (post-procedural MLD minus pre-procedural MLD), late loss (post-procedural MLD minus 6-month follow-up MLD), net gain (acute gain minus late loss), and loss index (late loss/acute gain). Angiographic restenosis was defined as re-narrowing of the target lesion >50% based on a single worst view.
Data collection and statistics
Demographic, clinical, and technical data were prospectively entered into a computerized database. All patients were interviewed and examined monthly. Follow-up coronary angiography was performed 6 months after the procedure. If a revascularization procedure involving the target site had been performed before the 6-month control-angiography, the findings of the most recent angiography (≥2 months after the initial procedure) were used as data for follow-up.
Statistical analysis was performed with SPSS 11.0 for Windows (Statistical Package for Social Sciences). Continuous variables were expressed as mean ± SD. Restenosis was considered as a categorical variable and categorical variables were compered using chi-square test (diabetes mellitus, hyperlipidemia, lesion complexity, and stent size of 4.0 or more vs smaller stents).
Results
From May 2005 to April 2006 60 patients were selected for implantation with a Meo:DrugStar ST stent. The stents were implanted successfully in 60 patients with 60 different lesions. Mean age (years) was 58 ± 11. There was a high proportion of patients with hypertension (55%) according to JNC-VII. Prevalence of patients with diabetes mellitus was 35% and 42% of patients had hyperlipidemia. Baseline clinical characteristics were summarized in and lesion baseline angiographic characteristics were summarized in .
Table 1 Baseline clinical characteristics of patients (n = 60)
Table 2 Baseline angiographic characteristics (n = 60 lesions)
All lesions were implanted with a Meo:DrugStar ST stent successfully and the device success rate was 100%. There was no stent thrombosis in the acute and late follow-up period. Mean stenosis ratio was 78 ± 13%, mean implanted stent diameter was 3.0 ± 0.4 mm and mean length was 22 ± 5 mm. Control coronary angiography was performed for 40 patients in a mean of 199 ± 43 days. Restenosis was detected in 4 (10%) of those patiens and 11 (27.5%) of 40 patients had insignificant amount of restenosis. Control coronary angiography was not performed for 20 patients since they did not have any cardiac complaints. When we thought the asymptomatic patients as being free of significant restenosis, we found the restenosis rate as 7.5%. While the mean stent length was 22.8 ± 5.7 mm in the restenosis group, it was 21.7 ± 5.1 mm in the other patients. While the mean stent diameter was 2.9 ± 0.2 mm in the restenosis groups, it was 3.0 ± 0.4 mm in the other patients.
Discussion
Angiographic and clinical outcome is favorable when percutaneous transluminal angioplasty is combined with stent implantation (CitationSerruys et al 1994). Restenosis rates were especially lower with balloon expandable stent implantation compared with balloon angioplasty in patients with coronary artery disease. The search for a better stent that has the most favorable results continues.
A breakthrough occurred in early 2000 with the development of stents that eluted pharmacology agents directly into the vessel wall by means of a controlled release from a durable polymer coating.
The European extension to SIRIUS, known as E-SIRIUS, enrolled 352 patients who had single native coronary lesions with a vessel diameter 2.5–3.0 mm and lesion length 15–32 mm. Patients were assigned randomly to treatment with SES or a bare metal stent (BMS). The binary angiographic restenosis rate 8 months later was reduced significantly in the sirolimus-eluting stents (SES) group (5.9% versus 42.3% in the BMS group; p = 0.0001) (CitationSchofer et al 2003).
The binary angiographic restenosis rate 6 months later in our study with Meo:DrugStar ST stents was 10%. Taking into consideration the symptom-free patients who did not come for control coronary angiography after 6 months, who had a non-significant restenosis rate, the restenosis rate could be accepted as 7.5%.
The results of this study indicate a potential benefit of the Meo:DrugStar ST stent for the prevention of stent thrombosis and restenosis in these relatively high-risk patients.
Study limitations
This study is an open, non-randomized, single-centre, prospective trial and we conclude that the Meo:DrugStar ST stent is a safe and effective choice with a low incidence of major adverse cardiac events and restenosis rate within 6 months of follow-up. The most important limitation of this study was the absence of intravascular ultrasound analysis, from which one can get more accurate quantitative data. Therefore, our results should be compared with larger-scale, randomized studies with other stent types.
References
- MosesJLeonMPompaJSirolimus-eluting stents versus standart stents in patients with stenosis in a native coronary arteryN Engl J Med200334913152314523139
- PompaJJTulliMDrug-eluting stentsCardiol Clin2006242173116781939
- SerruysPWde JaegerePKiemeneijFfor The Benestent Study GroupA comparison of balloon expandable stent implantation with balloon angioplasty in patients with coronary artery diseaseN Engl J Med1994331489958041413
- SchoferJSchluterMGershlickASirolimus-eluting stents for treatment of patients with long atherosclerotic lesions in small coronary arteries: double-blind, randomized controlled trial (E-SIRIUS)Lancet20033621093914550694