Abstract
Raynaud’s phenomenon is a clinical disorder with episodic digital ischemic vasospasm triggered by cold- or emotional-stress. It was first mentioned by Maurice Raynaud in 1862 describing “a local asphyxia of the extremities” and was further divided into primary Raynaud’s disease and secondary Raynaud’s phenomenon, which is often related to connective tissue diseases, but also physical or chemical strain. Though pathophysiology of Raynaud’s phenomenon is still poorly understood, systemic and local vascular effects are most likely to be involved in primary Raynaud’s disease. In secondary Raynaud’s phenomenon additional abnormalities in vascular structure and function may play the major role. Thus, medical treatment of Raynaud’s phenomenon remains unsatisfactory, due to limited understanding of pathophysiological mechanisms. This review addresses current evidence for medical treatment of primary and secondary Raynaud’s phenomenon with regard to pathophysiological mechanisms as well as future perspectives.
Keywords:
Definition and epidemiology
Raynaud’s phenomenon is described as episodic digital ischemic vasospasm triggered by cold- or emotional-stress leading to a pale and cyanotic skin with a postischemic phase of hyperemia; the typical “tricolore phenomenon”.Citation1 However, because a clear definition and nomenclature of Raynaud’s phenomenon is still lacking, we use the terms primary Raynaud’s disease and secondary Raynaud’s phenomenon throughout this review.
Raynaud’s disease was first mentioned by Maurice Raynaud in 1862 describing “a local asphyxia of the extremities” and was further divided into primary Raynaud’s disease and secondary Raynaud’s phenomenon by Thomas Lewis.Citation1,Citation2 Some criteria were proposed to diagnose primary rather than secondary Raynaud’s phenomenon. These include typical symptoms of digital vasospasm, absence of peripheral vascular disease, no evidence of tissue necrosis, normal nailfold capillaries, a negative antinuclear antibody test and a normal sedimentation rate.Citation3 Moreover, primary Raynaud’s disease typically affects all fingers, whereas secondary Raynaud’s phenomenon has an asymmetric distribution in most cases.
Primary Raynaud’s disease is common, with a prevalence of 3% to 5% in the general population, and remains uncomplicated without permanent injury.Citation3 The underlying mechanisms of temporary vasospasm are still poorly understood, but are suggested to be purely functional. However, secondary Raynaud’s phenomenon occurs in patients with connective tissue disease, but is also driven by physical or chemical strain and might have a more severe progression with digital necrosis and ulceration leading to disability.Citation4
Pathophysiology
The pathophysiology of Raynaud’s phenomenon remains unclear. In contrast to the first description by Maurice Raynaud, vascular rather than neural effects were suggested to play the major role.Citation1 Hence, systemic and local vascular effects were most likely to be involved in primary Raynaud’s disease, whereas additional abnormalities in vascular structure and vascular function are suggested to cause secondary Raynaud’s phenomenon.Citation4
Systemic vascular effects
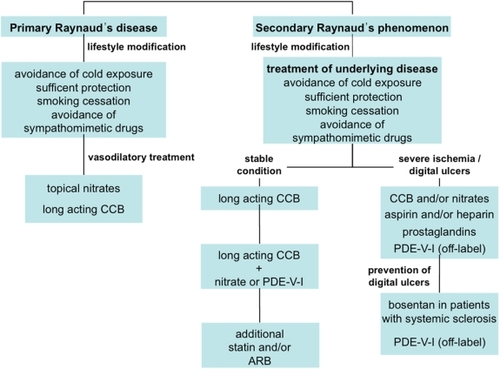
The key issue of Raynaud’s phenomenon is likely to be the imbalance of vasoconstriction and vasodilation due to alterations in neural control of vascular tone and circulating mediators ().Citation5 These mechanisms are suggested to play a major role in secondary Raynaud’s phenomenon due to connective tissue disease as systemic sclerosis. In these patients, circulating levels of endothelin-1, a potent vasoconstrictor, but also involved in fibrosis and structural vascular changes, are significantly increased.Citation6 Thus, inhibition of endothelin-1 receptors might affect vascular remodeling, proliferation of smooth-muscle cells as well as fibroblasts as a possible treatment target in patients with systemic sclerosis.Citation7
Figure 1 Imbalance of vasoconstriction and vasodilation in Raynaud’s disease. Vasodilators as nitric oxide and prostaglandins act via activation of adenylat- or guanylat-cyclase modulating protein kinase A/G. Vasoconstriction by endothelin or thromboxane is mediated by g-coupled specific receptors and is suggested to be increased in Raynaud’s phenomenon.
Another key player in vasoconstriction and likely in pathogenesis of Raynaud’s phenomenon is angiotensin II. The renin-angiotensin system (RAS) plays a major role in regulation of vascular tone, but also in vascular oxidative stress and remodeling.Citation8,Citation9 The role of the RAS in Raynaud’s phenomenon is yet unknown;Citation4 however, in patients with cutaneous systemic sclerosis, circulating levels of angiotensin II are increased which might offer a therapeutic approach with angiotensin-converting enzyme (ACE) inhibitors or angiotensin-receptor blockers.Citation10
Vasoconstrictive mediators are counterbalanced by vasodilators such as nitric oxide or prostaglandins. Despite vasodilating properties, prostaglandins are suggested to inhibit platelet aggregation as well as chemotaxis of leukocytes with consecutive adhesion to the endothelial monolayer.Citation11 Moreover, prostaglandins increase fibrinolytic activity, which may additionally play an important role, especially in patients with secondary Raynaud’s phenomenon.Citation12
Consistently, the vasodilator nitric oxide was found to be decreased more in secondary than primary Raynaud’s phenomenon, indicating the crucial role of endothelial function in vascular regulation and hence in Raynaud’s phenomenon.Citation6 Hence, endothelial synthesis of nitric oxide plays a major role in the pathophysiological mechanisms of Raynaud’s phenomenon. Endogenous as well as exogenous nitric oxide acts as a potent vasodilator via activation of guanylate-cyclase with increased levels of cyclic GMP, therefore resulting in dephosphorylation of the myosin light chain of vascular smooth muscle cells with consecutive vasodilation.
Local vascular effects
In patients with primary Raynaud’s disease, vascular response to alpha2-adrenergic agonists, serotonin and angiotensin II was increased during cooling and could be reversed by tyrosine kinase inhibitors.Citation13 As a possible mechanism, tyrosine phosphorylation was increased during cold exposure in these patients. Moreover, the alpha2c-adrenoreceptor is known to be important in thermoregulation, with an increased activity after cold exposure.Citation14 The underlying pathomechanism is a cold-induced increase of reactive oxygen species activating the rho/rho-kinase-pathway with consecutive translocation of the alpha2c-adrenoreceptor subtype to the cell membrane.Citation15,Citation16 Thus, increased expression of this receptor might play a role in primary Raynaud’s disease, especially in possible effects of estrogens on receptor expression, reflecting the high prevalence of primary Raynaud’s disease in women.
Moreover, regulation of vascular tone not only depends on humoral vasodilating mediators, but also on the release of neuropeptides from corresponding nerve endings. The calcitonin-gene-related peptide, for example, is a potent vasodilator secreted by nerves. In patients with both primary and secondary Raynaud’s phenomenon, neuron release was demonstrated to be diminished in skin biopsies.Citation17
Treatment
So far, medical treatment of Raynaud’s phenomenon remains unsatisfactory. Nevertheless, recent progress in the understanding of pathophysiological mechanisms has promoted further therapeutic approaches. Some clinical trials have revealed promising results, with different substances acting as vasodilators or inhibitors of increased vasoconstriction, but in general data are limited to small populations enrolled in these trials. Moreover, treatment strongly depends on the etiology of Raynaud’s phenomenon as well as on individual symptoms and presence of digital ulcers.
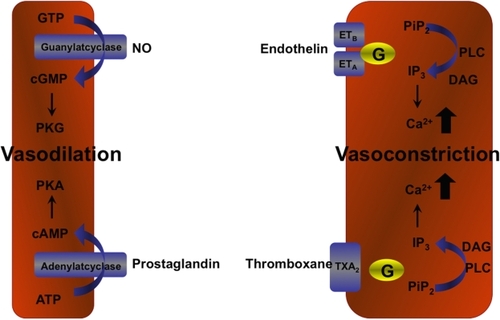
In both primary and secondary Raynaud’s phenomenon, lifestyle modifications are ranked first in the treatment algorithm. Proper body insulation, avoidance of cold exposure, stopping possible vasoconstrictive medication and smoking cessation play an important role and might be a sufficient treatment particularly in patients with primary Raynaud’s disease. In patients with secondary Raynaud’s phenomenon, avoidance of triggering physical or chemical injuries and adequate treatment of the underlying disease are fundamental.
With regard to possible pathophysiological mechanisms of Raynaud’s disease and phenomenon, medical treatment is based on regulation of vasomotion by direct vasodilators (nitrates, calcium-channel blockers, prostaglandins, PDE-V inhibitors) and inhibition of vasoconstriction (endothelin-receptor antagonists, angiotensin-receptor blockers, alpha-receptor blockers). Moreover, substances that increase endothelial function such as rho-kinase-inhibitors and statins as well as interaction with neural vasoregulation (serotonin-reuptake inhibitors) may improve symptoms of Raynaud’s disease or phenomenon.
Vasodilators
Nitrates
Nitrates have been used in both primary and secondary Raynaud’s phenomenon with different ways of administration: topical with transdermal patches or as different cream or gel formulations as well as in oral applications. Sustained release patches with glyceroltrinitrate were demonstrated to significantly reduce severity (P < 0.05) and number (P < 0.05) of Raynaud attacks in patients with primary (n = 21) and also in patients with secondary (n = 21) Raynaud’s phenomenon.Citation18 However, in 80% of the patients included in these trials, headache limited the use of topical nitrates. Moreover, nitrates had already been shown to improve digital ulcers compared to placebo in the early 1980s.Citation19 Nevertheless, efficacy as well as duration of possible beneficial effects of nitrates are still not clear in patients with secondary Raynaud’s phenomenon, in line with the earliest trials on nitrates in Raynaud’s phenomenon of the 1950s.Citation20 Thus, nitrates might be useful in primary Raynaud’s disease only and are highly limited by their frequent side effects, mainly headache and hypotension, irrespective of the way of administration. Interestingly, eight clinical trials are currently investigating the effect of topical nitrates on patients with primary and secondary Raynaud’s phenomenon. Thus, new data on this class of drug will be obtained in the near future.
Calcium channel blockers
In general, less cardioselective calcium channel blockers from the dihydropyridine group were suggested to be beneficial in Raynaud’s phenomenon and were first choice treatment especially in patients with primary Raynaud’s disease.Citation21 More cardioselective calcium channel blockers (phenylalkylamine type, benzothiazepine type) were shown to be ineffective in patients with severe Raynaud’s phenomenon.Citation22
Calcium channel blockers promote relaxation of vascular smooth muscle cells via inhibition of voltage-gated channels, leading to peripheral vasodilation. Especially short-acting substances such as nifedipine can lead to hypotension with consecutive reflex tachycardia, and also headache or flush.Citation23 Use of long-acting calcium channel blockers in patients with Raynaud’s phenomenon such as felodipine, amlodipine or nitrendipine is controversial.Citation24 A meta-analysis of calcium channel blockers in patients with primary Raynaud’s disease revealed a significant reduction of frequency (−2.8% to 5.0%, P = 0.01) as well as a decrease of severity of Raynaud attacks (−33%, P = 0.005).Citation25 These results are in line with a previous meta-analysis of studies evaluating the effect of calcium channel blockers in patients with Raynaud’s phenomenon due to systemic sclerosis. Within 2 weeks treatment, there was a reduction of 8.3 attacks per week and a 35% decline in severity of clinical symptoms.Citation26 However, improvement of clinical symptoms might be a short-term effect of treatment with calcium channel blockers as beneficial effects can be lost in long-term treatment.Citation24 In a head to head comparison of 40 mg nifedipine with intravenous iloprost in patients with secondary Raynaud’s phenomenon, there was no effect of treatment with nifedipine after 1 year.Citation27
In clinical practice, calcium channel blockers are the first choice in primary Raynaud’s disease and have been suggested for testing in secondary Raynaud’s phenomenon. Treatment should start with low dosages and should be titrated with regard to individual symptoms. Recommended doses are nifedipine 10 to 30 mg 3 times daily or amlodipine 5 to 20 mg once daily. In patients with a CREST-syndrome, calcium channel blockers can reduce sphincter tone in the lower esophagus, in these patients calcium channel blockers should be used with caution.
Prostaglandins
Prostaglandins have vasodilatory properties, antiproliferative effects on vasculature and inhibit platelet aggregation. In the treatment of primary and secondary Raynaud’s phenomenon, intravenous administration of prostaglandin E1 as well as iloprost were shown to be beneficial.Citation28 In patients with secondary Raynaud’s phenomenon, treatment with iloprost 6 weekly significantly decreased the Raynaud’s score compared to the calcium channel blocker nifedipin (P = 0.002).Citation27 Moreover, in a multicenter trial with 131 patients with systemic sclerosis, iloprost improved Raynaud’s score (decrease of 39% vs 22%, P = 0.005) as well as healing of digital ulcers in comparison to placebo.Citation29 However, the role of oral or inhaled preparations of prostaglandins is yet not clear and should be evaluated in further clinical trials.
Side effects of prostaglandins were dose-dependent and a result of peripheral vasodilation with headache, flush and nausea. In patients with congestive heart failure, prostaglandins may lead to pulmonary edema; hence outpatient treatment is not recommended in these patients. Moreover, low-dose treatment with prostaglandins (0.5 ng/kg body weight per min ilpoprost) is suggested to be equally effective to high-dose treatment (2.0 ng/kg body weight per min ilpoprost) in patients with systemic sclerosis.Citation30
Phosphodiesterase inhibitors
Phosphodiesterase type V (PDE-V) inhibitors mediate vasodilatory effects via accumulation of cyclic guanosine monophosphate in vascular smooth muscle cells and were indicated in treatment of erectile dysfunction and more recently in pulmonary hypertension.Citation31 In patients with pulmonary hypertension due to connective tissue disease, medical treatment with PDE-V inhibitors was reported to improve symptoms of secondary Raynaud’s phenomenon. Consistently, PDE-V inhibitors were demonstrated to have beneficial effects in primary and secondary Raynaud’s phenomenon in several studies and case reports. In a single-center trial with 16 patients with secondary Raynaud’s phenomenon resistant to vasodilatory treatment, 4-week treatment with 50 mg sildenafil twice daily reduced number of attacks (35 ± 14 vs 52 ± 18, P = 0.0064) and mean Raynaud’s condition score (2.2 ± 0.4 vs 3.0 ± 0.5, P = 0.0386).Citation32 Moreover, capillary blood flow improved significantly (P = 0.0004) compared to placebo. These data were consistent with two case series in which sildenafil reduced frequency and severity of attacks in patients with secondary Raynaud’s phenomenon.Citation33,Citation34
In a case-report, tadalafil, another PDE-V inhibitor, was reported to be beneficial in a patient with secondary Raynaud’s phenomenon not responding to sildenafil.Citation35 Recent data are in line with this observation. In patients with systemic sclerosis, plasma endothelin-1 levels were reduced by daily treatment with tadalafil.Citation36 However, in a randomized, cross-over trial comparing tadalafil with placebo in patients with Raynaud’s phenomenon and systemic sclerosis, there was no significant difference in number, severity and duration of Raynaud’s attacks.Citation37
PDE-V inhibitors are one of the most promising class of substances for treatment of Raynaud’s phenomenon, but more data are needed. A current trial evaluating a novel PDEV-inhibitor (SLx-2101) in patients with secondary Raynaud’s phenomenon has been completed, and the results are expected to be published in early in 2010. At the moment, sildenafil shows best evidence for beneficial effects.
Inhibition of vasoconstriction
Endothelin receptor antagonists
Endothelin-1 is a potent vasoconstrictor, but is also involved in vascular remodeling and local fibrosis, especially in patients with secondary Raynaud’s phenomenon.Citation7 In patients with systemic sclerosis, plasma concentrations of endothelin-1 were reported to be significantly increased, with enhanced proliferation and consecutive hypertrophy of vascular smooth muscle cells and fibroblasts.Citation38 Thus, inhibition of endothelin-1 exerts chronic effects on proliferation and vascular structure rather than acute effects on vasomotion. Bosentan is a competitive antagonist of both endothelin receptor subtypes A and B, with a higher affinity to the first receptor. In the RAPIDS-1 trial (Randomized Placebo-controlled Investigation of Digital Ulcers in Scleroderma) bosentan was evaluated in 122 patients with systemic sclerosis. During the treatment period of 4 months, bostentan reduced onset of new digital ulcers by 48% in comparison to placebo.Citation39 However, the second endpoint of time to healing of digital ulcers did not differ significantly between the two treatment arms. The RAPIDS-2 trial included 188 patients with secondary Raynaud’s phenomenon treated with bosentan or placebo for 20 to 32 weeks. Again, number of new digital ulcers decreased significantly with bosentan (bosentan 1.9 ± 0.2 vs placebo 2.7 ± 0.3, P = 0.035). Based on these results, bosentan was marketed in the European Union in 2007, being indicated for the reduction of onset of digital ulcers in patients with systemic sclerosis. Adverse effects of bosentan were particularly increased hepatic aminotransferase levels, which were dose-dependent and might occur in about 10% of patients treated.
Angiotensin receptor blockers
ACE inhibitors as well as ARBs were demonstrated to be beneficial in cardiovascular risk patients.Citation40 ACE inhibitors and ARBs may also provide improvement in patients with Raynaud’s phenomenon, although no definite evidence exists to suggest that they are superior to commonly used vasodilating substances.Citation41 Large, randomized, controlled trials are needed to compare the effects of ACE inhibitors and ARBs with conventional vasodilatory treatment.Citation42 In one small trial including patients with primary (n = 25) and secondary (n = 27) Raynaud’s phenomenon, losartan was demonstrated to decrease frequency of attacks significantly compared to nifedipine (P = 0.018) after treatment for 15 weeks. Additionally, symptoms improved with losartan (P < 0.05).Citation43 Beneficial effects were more pronounced in the subgroup of patients with primary Raynaud’s disease. Nevertheless, further trials are needed to judge the role of inhibitors of the RAS in patients with Raynaud’s phenomenon.
Alpha-adrenoreceptor blockers
Alpha-adrenoreceptors play an important role in sympathetic nervous regulation of vascular tone, but also in skin temperature regulation.Citation41 Prazosin inhibits the alpha-1 postsynaptic adrenoreceptor with consecutive peripheral vasodilation. In a meta-analysis including 2 trials with a total of 40 patients with secondary Raynaud’s phenomenon due to systemic sclerosis, prazosin significantly decreased severity and frequency of Raynaud’s attacks.Citation44 Despite beneficial effects, several side effects as nausea, dizziness, headache, palpitations and hypotension limit the use of this substance.
Pathophysiological mechanisms and especially the role in thermoregulation of the alpha2c-adrenoreceptor subtype have been described above. In a small trial with 13 patients with systemic sclerosis and consecutive Raynaud’s phenomenon, a specific alpha2c-adrenoreceptor subtype blocker decreased time to recovery of skin temperature after cold exposure significantly (50% of recovery within 5.8 vs 10.0 min, P = 0.02).Citation45 Moreover, digital blood flow increased compared to placebo. These data were promising, even for low frequency of side effects, but further studies with more relevant endpoints such as frequency and severity of attacks are needed.
Improvement of endothelial function
Rho-kinase inhibitors
Rho-kinase is involved in cold-induced modulation of expression or rather translocation of the alpha2c-adrenoreceptor subtype to the plasma membrane. Moreover, rho-kinase is a key mediator of pleiotropic effects of statins, with beneficial effects on endothelial function and development of atherosclerosis.Citation46 Thus, overactivity of rho-kinase was described in several vascular disorders as cerebral ischemia, and also coronary vasospasm.Citation47 Fasudil is a potent inhibitor of rho-kinase and was demonstrated to have beneficial effects in vasospastic angina.Citation48 Recently, fasudil was shown to increase nitric oxide-dependent forearm blood flow and to prevent aortic vasoconstriction in an animal model.Citation49,Citation50 A phase III trial with 24 patients with secondary Raynaud’s phenomenon is currently being performed with fasudil at the Johns Hopkins University (clinicaltrials.gov identifier: NCT00498615). Results may be available in 2010.
Statins
Statins display pleiotropic effects on endothelial function, which may be beneficial also in Raynaud’s phenomenon. In patients with secondary Raynaud’s phenomenon due to systemic sclerosis, 40 mg of atorvastatin (n = 56) or placebo (n = 28) was added to ongoing vasodilatory treatment.Citation51 The overall number of digital ulcers was significantly reduced in the statin group, with a consecutive improvement of quality of life. Another open-label study is currently investigating the effects of atorvastatin on Raynaud’s phenomenon in patients with systemic lupus erythematodes. Thus, HMG-CoA-reductase inhibitors were suggested to be a promising therapeutic option, especially in addition to existing vasodilatory treatment, but more data are necessary to judge the definite role of this class of drugs.
Neural vasoregulation
Serotonin reuptake inhibitors
Digital vasomotion may in part depend on serotonin reuptake in the central nervous system. Moreover, serotonin reuptake may interfere with platelets, but the overall role in Raynaud’s phenomenon remains uncertain. In patients with primary Raynaud’s disease, 6 weeks’ treatment with the selective serotonin reuptake inhibitor fluoxetine (20 mg) improved severity and frequency of attacks compared to nifedipine (40 mg) significantly (P < 0.001), but effects were less pronounced in secondary Raynaud’s phenomenon.Citation52 Consistently, a metaanalysis of the serotonin-reuptake inhibitor ketanserin demonstrated no beneficial effects in secondary Raynaud’s phenomenon due to systemic sclerosis.Citation53 Currently there are insufficient data to support the routine use of this substance in Raynaud’s phenomenon.
Treatment algorithm
Raynaud’s phenomenon is a complex disease with several factors suggested to be involved in pathological vasomotion and also vascular remodeling. Thus, the decision on therapeutic approach has to be taken on a case by case basis. In patients with primary Raynaud’s disease, lifestyle modifications eclipse medical treatment. Avoidance of cold exposure and protection are most important in these patients. Moreover, smoking cessation is recommended, despite unclear evidence of an association with Raynaud’s phenomenon. Citation54 If severity of symptoms requires medical treatment despite lifestyle changes, topical nitrates or low-dose treatment with calcium-channel blockers are recommended.
In patients with secondary Raynaud’s phenomenon, treatment of the underlying disease is crucial. In addition to lifestyle changes, calcium-channel blockers are also suggested to be the first-line treatment in these patients. Patients who do not respond or do not tolerate calcium-channel blockers may use other vasodilatory substances alone or in combination, whereas data from clinical trials on combined treatment in Raynaud’s phenomenon are not available. A possible treatment algorithm suggested by the authors is depicted in . Further trials of several different substances are expected within the next few years. PDE-V inhibitors, rho-kinase inhibitors and endothelin-receptor antagonists especially seem to be most promising for treatment of both primary and secondary Raynaud’s phenomenon.
Patients who develop severe digital ischemia including ulcerations often require hospitalization with application of intravenous prostaglandins. PDE-V inhibitors may also be used for treatment of digital ulcers, but their application is still “off-label”. Patients with systemic sclerosis and history of digital ulcers may be treated with bosentan for prevention of onset of new ulcers.
Future perspective
Diagnosis and treatment of Raynaud’s phenomenon is a major challenge in view of the wide variety of symptoms and pathophysiological mechanisms involved, especially in secondary Raynaud’s phenomenon due to connective tissue diseases. Pathological vascular conditions, but also structural abnormalities are suggested to play the major role in pathophysiology of Raynaud’s phenomenon, but are still poorly understood. The key factors influencing these mechanisms are endothelin-1 and endothelial dysfunction, with consecutive decreased nitric oxide synthesis being responsible for the imbalance of vasoconstriction and vasodilation. Hence, substances inhibiting vascular effects of endothelin-1 as well as improving endothelial function or enhancing nitric oxide-related effects as PDE-V inhibitors are suggested to be the most promising agents for future treatment and research, especially in secondary Raynaud’s phenomenon.
Disclosures
The authors declare no conflicts of interest.
References
- RaynaudMLocal Asphyxia and Symmetrical Gangrene of the ExtremitiesLondonNew Sydenham Society1862
- LewisTExperiments relating to the peripheral mechanisms involved in spasmodic arrest of the circulation in the fingers, a variety of Raynaud’s diseaseHeart1929157101
- LeRoyECMedsgerTAJrRaynaud’s phenomenon: a proposal for classificationClin Exp Rheumatol19921054854881458701
- BakstRMerolaJFFranksAGJrSanchezMRaynaud’s phenomenon: pathogenesis and managementJ Am Acad Dermatol200859463365318656283
- KahelehBMatucci-CerinicMRaynaud’s phenomenon and scleroderma. Dysregulated neuroendothelial control of vascular toneArthritis Rheum199538147818557
- RajagopalanSPfenningerDKehrerCIncreased asymmetric dimethylarginine and endothelin 1 levels in secondary Raynaud’s phenomenon: implications for vascular dysfunction and progression of diseaseArthritis Rheum20034871992200012847693
- KirchengastMMunterKEndothelin-1 and endothelin receptor antagonists in cardiovascular remodelingProc Soc Exp Biol Med1999221431232510460693
- BaumhakelMCustodisFSchlimmerNLaufsUBohmMImprovement of endothelial function of the corpus cavernosum in apolipoprotein E knockout mice treated with irbesartanJ Pharmacol Exp Ther2008327369269818812494
- FriedrichEBTeoKKBohmMACE inhibition in secondary prevention: are the results controversial?Clin Res Cardiol2006952616716598512
- KawaguchiYTakagiKHaraMAngiotensin II in the lesional skin of systemic sclerosis patients contributes to tissue fibrosis via angiotensin II type 1 receptorsArthritis Rheum200450121622614730619
- YardumianDAMackieIJBrennanECBullHMachinSJPlatelet function studies during and after infusions of ZK 36374, a stable prostacyclin analogue, to healthy volunteersHaemostasis198616120262422095
- BerteleVMussoniLdel RossoGDefective fibrinolytic response in atherosclerotic patients – effect of iloprost and its possible mechanism of actionThromb Haemost19886021411442464198
- FurspanPBChatterjeeSFreedmanRRIncreased tyrosine phosphorylation mediates the cooling-induced contraction and increased vascular reactivity of Raynaud’s diseaseArthritis Rheum20045051578158515146428
- ChotaniMAFlavahanSMitraSDauntDFlavahanNASilent alpha(2C)-adrenergic receptors enable cold-induced vasoconstriction in cutaneous arteriesAm J Physiol20002784H1075H1083
- BaileySREidAHMitraSFlavahanSFlavahanNARho kinase mediates cold-induced constriction of cutaneous arteries: role of alpha2C-adrenoceptor translocationCirc Res200494101367137415087420
- BaileySRMitraSFlavahanSFlavahanNAReactive oxygen species from smooth muscle mitochondria initiate cold-induced constriction of cutaneous arteriesAm J Physiol20052891H243H250
- BunkerCBTerenghiGSpringallDRPolakJMDowdPMDeficiency of calcitonin gene-related peptide in Raynaud’s phenomenonLancet19903368730153015331979366
- TehLSManningJMooreTTullyMPO’ReillyDJaysonMISustained-release transdermal glyceryl trinitrate patches as a treatment for primary and secondary Raynaud’s phenomenonBr J Rheumatol19953476366417670782
- FranksAGJrTopical glyceryl trinitrate as adjunctive treatment in Raynaud’s diseaseLancet19821826376776119495
- KlecknerMJrAllenEVWakimKGThe effect of local application of glyceryl trinitrate (nitroglycerine) on Raynaud’s disease and Raynaud’s phenomenon; studies on blood flow and clinical manifestationsCirculation19513568168914831190
- Stosic-GrujicicSDMaksimovicDDStojkovicMBLukicMLPentoxifylline prevents autoimmune mediated inflammation in low dose streptozotocin induced diabetesDev Immunol200183–421322111785671
- KinneyELNicholasGGGalloJPontorieroCZelisRThe treatment of severe Raynaud’s phenomenon with verapamilJ Clin Pharmacol198222174767037872
- AbernethyDRSchwartzJBCalcium-antagonist drugsN Engl J Med1999341191447145710547409
- OpieLHYusufSKublerWCurrent status of safety and efficacy of calcium channel blockers in cardiovascular diseases: a critical analysis based on 100 studiesProg Cardiovasc Dis200043217119611014332
- ThompsonAEPopeJECalcium channel blockers for primary Raynaud’s phenomenon: a meta-analysisRheumatology (Oxford)200544214515015546967
- ThompsonAESheaBWelchVFenlonDPopeJECalcium-channel blockers for Raynaud’s phenomenon in systemic sclerosisArthritis Rheum20014481841184711508437
- ScorzaRCaronniMMascagniBEffects of long-term cyclic iloprost therapy in systemic sclerosis with Raynaud’s phenomenon. A randomized, controlled studyClin Exp Rheumatol200119550350811579708
- Stosic-GrujicicSMaksimovicDBadovinacVAntidiabetogenic effect of pentoxifylline is associated with systemic and target tissue modulation of cytokines and nitric oxide productionJ Autoimmun2001161475811221996
- WigleyFMWiseRASeiboldJRIntravenous iloprost infusion in patients with Raynaud phenomenon secondary to systemic sclerosis. A multicenter, placebo-controlled, double-blind studyAnn Intern Med199412031992067506013
- KawaldABurmesterGRHuscherDSunderkotterCRiemekastenGLow versus high-dose iloprost therapy over 21 days in patients with secondary Raynaud’s phenomenon and systemic sclerosis: a randomized, open, single-center studyJ Rheumatol20083591830183718634152
- WilkinsMRPaulGAStrangeJWSildenafil versus Endothelin Receptor Antagonist for Pulmonary Hypertension (SERAPH) studyAm J Resp Crit Care Med2005171111292129715750042
- FriesRShariatKvon WilmowskyHBohmMSildenafil in the treatment of Raynaud’s phenomenon resistant to vasodilatory therapyCirculation2005112192980298516275885
- LichtensteinJRUse of sildenafil citrate in Raynaud’s phenomenon: comment on the article by Thompson et alArthritis Rheum2003481282283author reply 312528146
- KumanaCRCheungGTLauCSSevere digital ischaemia treated with phosphodiesterase inhibitorsAnn Rheum Dis200463111522152415479910
- BaumhaekelMSchefflerPBoehmMUse of tadalafil in a patient with a secondary Raynaud’s phenomenon not responding to sildenafilMicrovasc Res200569317817915896360
- RosatoELetiziaCProiettiMPlasma adrenomedullin and endothelin-1 levels are reduced and Raynaud’s phenomenon improved by daily tadalafil administration in male patients with systemic sclerosisJ Biol Regul Homeost Agents2009231232919321043
- SchiopuEHsuVMImpensAJRandomized placebo-controlled crossover trial of tadalafil in Raynaud’s phenomenon secondary to systemic sclerosisJ Rheumatol200936102264226819755613
- MorelliSFerriCPolettiniEPlasma endothelin-1 levels, pulmonary hypertension and lung fibrosis in patients with systemic sclerosisAm J Med19959932552607653485
- KornJHMayesMMatucci CerinicMDigital ulcers in systemic sclerosis: prevention by treatment with bosentan, an oral endothelin receptor antagonistArthritis Rheum200450123985399315593188
- WernerCBaumhakelMTeoKKRAS blockade with ARB and ACE inhibitors: current perspective on rationale and patient selectionClin Res Cardiol200897741843118454336
- Garcia-CarrascoMJimenez-HernandezMEscarcegaROTreatment of Raynaud’s phenomenonAutoimmunity reviews200881626818692160
- WoodHMErnstMERenin-angiotensin system mediators and Raynaud’s phenomenonAnn Pharmacother200640111998200217003081
- DziadzioMDentonCPSmithRLosartan therapy for Raynaud’s phenomenon and scleroderma: clinical and biochemical findings in a fifteen-week, randomized, parallel-group, controlled trialArthritis Rheum199942122646265510616013
- PopeJFenlonDThompsonAPrazosin for Raynaud’s phenomenon in progressive systemic sclerosisCochrane Database Syst Rev20002CD00095610796398
- WiseRAWigleyFMWhiteBEfficacy and tolerability of a selective alpha(2C)-adrenergic receptor blocker in recovery from cold-induced vasospasm in scleroderma patients: a single-center, double-blind, placebo-controlled, randomized crossover studyArthritis Rheum200450123994400115593189
- LaufsULa FataVPlutzkyJLiaoJKUpregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitorsCirculation19989712112911359537338
- RikitakeYLiaoJKROCKs as therapeutic targets in cardiovascular diseasesExp Rev Cardiovasc Ther200533441451
- MasumotoAMohriMShimokawaHUrakamiLUsuiMTakeshitaASuppression of coronary artery spasm by the Rho-kinase inhibitor fasudil in patients with vasospastic anginaCirculation2002105131545154711927519
- BussemakerEHerbrigKPistroschFPalmCPassauerJRole of rho-kinase in the regulation of vascular tone in hypertensive renal transplant recipientsAtherosclerosis2009207256757219717154
- ChanCKMakJCManRYVanhouttePMRho kinase inhibitors prevent endothelium-dependent contractions in the rat aortaJ Pharmacol Exp Ther2009329282082619193928
- Abou-RayaAAbou-RayaSHelmiiMStatins: potentially useful in therapy of systemic sclerosis-related Raynaud’s phenomenon and digital ulcersJ Rheumatol20083591801180818709692
- ColeiroBMarshallSEDentonCPTreatment of Raynaud’s phenomenon with the selective serotonin reuptake inhibitor fluoxetineRheumatology (Oxford)20014091038104311561116
- PopeJFenlonDThompsonAKetanserin for Raynaud’s phenomenon in progressive systemic sclerosisCochrane Database Syst Rev20002CD00095410796396
- HerrickALPathogenesis of Raynaud’s phenomenonRheumatology (Oxford)200544558759615741200