Abstract
Background
Antihypertensive agents can reduce arterial stiffness. We hypothesized that an angiotensin receptor blocker (ARB) irbesartan and an angiotensin converting enzyme inhibitor (ACEI) lisinopril improved arterial compliance.
Methods
A randomized, double-blind, double-dummy, controlled crossover trial. Fifteen hypertensive patients, mean age 65.5 ± 8.9 years (mean ± SD) were given irbesartan (150 to 300 mg/day) or lisinopril (10 to 20 mg/day) for 12 weeks and then crossed over for 12 weeks. Pulse wave velocity (PWV) in the carotid-femoral (CF), carotid-radial (CR), and femoral dorsalis-pedis (FD) were measured using a Complior® PWV system.
Results
After 12 weeks, systolic blood pressure (SBP) decreased from 162.4 ± 12.9 to 134.5 ± 14.8 with irbesartan and to 145.2 ± 25 mmHg with lisinopril. Irbesartan and lisinopril reduced PWV (CF) in the elastic arterial system from 15.1 ± 5 to 13.3 ± 2.6 (p < 0.005) and to 14 ± 4.7 (p < 0.05) m/s respectively (p = 0.345). Irbesartan reduced PWV (CR) and PWV (FD), whereas lisinopril did not. The difference between treatments was significant after SBP adjustment (p = 0.037 for PWV (CR) and p < 0.001 for PWV (FD)).
Conclusions
Irbesartan improved arterial compliance in elastic and muscular arteries, whereas lisinopril improved it only in elastic arteries.
Introduction
Hypertension is one of the most important risk factors for cardiovascular diseases and is associated with increased morbidity and mortality.Citation1 It is known that the treatment of hypertensive subjects reduces the diseases associated with hypertension, for example stroke and coronary artery disease.Citation2,Citation3 Despite this favorable effect of antihypertensive treatment, the incidence of cardiovascular diseases remains higher in treated hypertensives than in matched controls with similar blood pressure (BP) levels,Citation4 suggesting the presence of other additional risk factors, such as previous vascular damage, which may be represented by a decreased arterial compliance. Increased arterial stiffness in particular as assessed by pulse wave velocity (PWV), is an independent marker of cardiovascular disease in hypertensive subjects and is linked to ventricular hypertrophy and atherosclerosis.Citation5–Citation9 It is also higher in patients with end stage renal disease and diabetes.Citation10–Citation12 Changes in arterial compliance have been used to assess the effect of some therapies.Citation13,Citation14
Angiotensin II plays an important role in development of an increased BP and also tissue damage. The two categories of drugs acting on the renin-angiotensin system have been shown to have beneficial effects on BP, heart and arteries. The inhibition of angiotensin-converting enzyme (ACE) can provide a protective effect on the adverse changes due to hypertension and prevent cardiovascular outcomes, possibly more than is achieved with diuretic based-therapy.Citation15 Treatment with ACE inhibitors increases arterial distensibilityCitation16 and drugs blocking the angiotensin II receptor have been shown to improve endothelial function and increase arterial compliance of small and large arteries in addition to their antihypertensive effect.Citation17–Citation19 It has been suggested that both valsartan and captopril reduce the pulse wave velocity (PWV) and Augmentation Index by a similar amount in essential hypertension.Citation20
The purpose of this study was to assess the effect of an angiotensin receptor blocker (ARB), irbesartan, and an ACE inhibitor (ACEI), lisinopril, on arterial compliance, comparing the effects of these two antihypertensive drugs on different arterial segments, one predominately elastic and the other predominately muscular.
Methods
Study population
We performed a randomized, double-blind, double-dummy, controlled crossover trial. Fifteen hypertensive patients without cardiovascular complications, mean age 65.5 ± 8.9 years (mean ± SD) were recruited. They were all nonsmokers. They were randomly allocated to receive irbesartan (150 to 300 mg/day) or lisinopril (10 to 20 mg/day) for 12 weeks and then immediately crossed over for a further 12 weeks.
The study was approved by the Ethics Committee of the Hammersmith Hospital Trust, London UK.
Exclusion criteria
We excluded subjects on hormone replacement therapy or with a history of cardiac failure or valvular heart disease. Subjects with contraindications to an ACEI or ARB were also excluded.
Study design
Patients who were currently taking antihypertensive medication had this stopped for 2 weeks prior to the screening visit, while having their BP monitored regularly. Between the screening and baseline visit, BP was measured once a week for 3 weeks. On these occasions the mean of three measurements was recorded and used for fulfilling the study entry criteria, ie, sitting systolic BP (SBP) >160 mmHg and/or sitting diastolic BP (DBP) > 90 mmHg.
At the screening visit written informed consent was obtained and medical history recorded. Lying, sitting and standing BP were measured and a physical examination performed. PWV and BP were recorded at the baseline visit and were repeated at 12 and 24 weeks.
The initial treatment was 150 mg irbesartan or 10 mg lisinopril. These were titrated to 300 mg and 20 mg respectively at weeks 6 and 18 if the SBP > 160 mmHg and/or the DBP was > 90 mmHg. At week 12, the patients were crossed over and received the other drug.
Statistical analysis
The baseline data are presented as means ± standard deviation. Data were analyzed according to the method for crossover trials described by SennCitation21 using SAS Version 8. Parametric data were analyzed by means of a matched paired t-test with adjustment for any period effect and a test for carry-over. PWV readings were converted for a standardized reading of 150 mmHg and repeat t-test was performed between the two groups to eliminate any effect of BP on PWV.
Procedures
Baseline characteristics were measured ().
Table 1 Characteristics of the study population at baseline
Blood pressure (BP)
The average of three BP readings at the brachial artery, taken at 5-minute intervals, in the right upper arm of the supine subject, was performed using an Omron HEM-705CP automatic BP recording unit.
Pulse wave velocity (PWV)
PWV in the central, elastic arteries (carotid-femoral region) and the peripheral, muscular arteries (carotid-radial and femoral-dorsalis pedis regions) were determined using a Complior® (Colson Medicals, Paris) PWV recording unit.Citation22 Two sensors were positioned, one at the base of the right common carotid artery and one over the radial artery, similarly over the right common carotid artery and the right femoral artery and over the right femoral artery and the ipsilateral dorsalis pedis artery, thereby continuously measuring pulse wave signals. Distances between the two applanation sites were measured as a straight line between these points on the skin surface, using a tape measure. The time interval between the feet of two simultaneously recorded waves at the two applanation sites was determined and PWV was calculated.
Results
The characteristics of study population are shown in . We studied 15 patients (7 women and 8 men).
After 12 weeks of treatment SBP decreased from 162.4 ± 12.9 mmHg to 134.5 ± 14.8 mmHg (p < 0.05) with irbesartan and to 145.2 ± 25 mmHg (p < 0.05) with lisinopril and DBP from 98.7 ± 8.1 mmHg to 78.6 ± 9.2 mmHg (p < 0.05) and to 84.1 ± 11.6 mmHg (p < 0.05) with lisinopril (, ). There was a trend to significant differences in the decrease of SBP and DBP between the two drugs (p = 0.08).
Figure 1 Blood pressure systolic (SBP) and diastolic (DBP) at baseline and after 12 weeks treatment with irbesartan and lisinopril. The changes are statistically significant for both drugs (p < 0.05) for SBP and DBP.
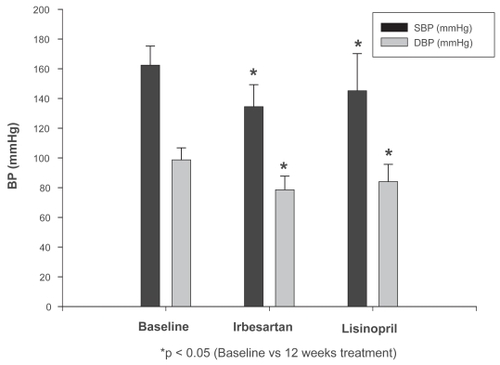
Table 2 Baseline and end of trial results
We found a significant decrease of PWV (C-F) for both drugs after 12 weeks of treatment. The PWV (C-F) decreased from 15.1 ± 5 m/s to 13.3 ± 2.6 m/s (p < 0.005) and to 14 ± 4.7 m/s (p < 0.05) with irbesartan and lisinopril respectively (). The effects of the two treatments were not statistically significantly different (p = 0.345).
We found significant decrease of PWV (F-D) for irbesartan, but not for lisinopril. The PWV (F-D) decreased after treatment with irbesartan from 11 ± 2.6 m/s to 10.1 ± 2.6 m/s (p < 0.05) (). This difference between the treatments was statistically significant before (p = 0.01) and after (p < 0.001) adjustment for SBP = 150 mmHg.
PWV (C-R) after 12 weeks of treatment changed from 12.4 ± 2.3 m/s to 11.6 ± 2.2 m/s (p = 0.19) with irbesartan and to 12.4 ± 2.4 m/s (p = 0.99) with lisinopril. After adjustment for SBP = 150 mmHg this value changed respectively to 11.0 ± 2.1 m/s (p = 0.02) and to 12.2 ± 2.5 m/s (p = 0.76) ().
PWV (F-D) after 12 weeks of treatment changed from 11.0 ± 2.6 m/s to 10.1 ± 2.4 m/s (p ≤ 0.05) with irbesartan and to 11.4 ± 1.5 m/s (p = 0.85) with lisinopril. After adjustment for SBP = 150 mmHg this value changed respectively to 10.9 ± 2.3 m/s (p ≤ 0.05) and to 11.7 ± 2.4 m/s (p = 0.86) ().
Discussion
This study investigated the effects of two different antihypertensive drugs, lisinopril and irbesartan, on the PWV, an index of arterial compliance, in predominantly elastic compared with predominantly muscular arteries. There was a large BP drop in the patients included in the two groups, which may be due to the fact that both medications were titrated upwards at close intervals although the BP readings at the end of the 12 weeks were not significantly different statistically between the two. However lisinopril was not titrated to 40 mg, which could have resulted in the differences in the BP lowering effects between the two drugs. Recent analysis of the CALM II study showed that lisinopril may have different effects on SBP, DBP and pulse pressure compared to candesartan (an ARB),Citation23 and since 24-hour ambulatory BP monitoring was not performed in this study, the observed differences in BP reduction and subsequent differences in PWV need a larger study including 24-hour BP monitoring. However, given the different resultant BP findings at the end of the 12 weeks, and knowing that BP reduction affects vascular compliance, the underlying biologic effects of the two drugs can not be fully explained. A way to address this impact of differences in achieved BP readings would be to titrate both drugs upwards to result in similar BP readings at the end of the study period.
Hypertension is associated with increased arterial stiffnessCitation7,Citation8 but it is also known that a reduction in BP is associated with an improved arterial compliance.Citation23,Citation24 The renin-angiotensin system affects the properties of arteries, both predominantly elastic and muscular. Neutel et al showed that benazepril improved arterial compliance in monotherapy and more efficaciously in combination with amlodipine.Citation16 Shargorodsky et al showed the positive effect of prolonged treatment with the AT1 receptor blocker valsartan on the small and large arterial compliance in a group of uncomplicated essential hypertensives.Citation17 Only one other study compared the effect of ARBs with ACEIs on arterial compliance, showing a significant decrease in augmentation index and PWV with both drugs,Citation20 but did not analyze the effect of these on different types of arteries.
Our results confirm the finding of these previous studies on the PWV, one of the most important measures of arterial compliance. Evaluating the PWV, it has been possible for us compare the effect of these two drugs on different types of arteries. We assessed PWV C-F, PWV C-R and PWV F-D to study different segments of the arterial tree. Our findings confirm the positive effects of irbesartan and lisinopril on improving arterial compliance in elastic vessels. After 12 weeks of treatment for both the drugs the decrease in PWV C-F was statistically significant. This suggests a positive effect of these two drugs in improving the cardiovascular risk, over and above the known effects of lowering BP that were evident and statistically significant in our study.
Similar effects were also seen with irbesartan on the muscular arteries. When on treatment with irbesartan but not when on lisinopril we found a significant decrease in the PWV F-D, suggesting a positive effect of the ARBs on the arterial compliance of the muscular vessels. Our finding is important as it was also significant after adjustment for SBP. Correcting for SBP also showed that irbesartan produced a similar effect on the muscular arteries in the carotid-radial region. This suggests that irbesartan improved arterial compliance in the muscular arteries independently of its effect on BP, whereas lisinopril did not.
There are a number of large epidemiological studies showing that different antihypertensive agents have different outcomes. For example in the LIFE trial it was shown that treatment with losartan was more effective than atenolol in reducing cardiovascular morbidity and mortality as well as mortality from all causes in patients with hypertension, diabetes and LVH.Citation25
In elderly patients with heart failure the ELITE-ICitation26 trial showed better outcomes with an ARB than with an ACEI, showing that treatment with losartan was associated with a lower mortality than that with captopril. This effect was not sustained in the ELITE-II trial.Citation27
In our study the different effects of the two drugs on muscular arteries is difficult to explain. The effects may be due to a more specific effect of the ARB on the vascular smooth muscle contraction or due to a difference in release of some endothelial mediators. However, some studies have shown a similar increase in the bioavailability of nitric oxide after treatment with both drugs.Citation28 There may be some other properties of the ARBs that explain this finding. There is some evidence that ARBs improve erectile dysfunction in hypertensive men and that that this may not be apparent with an ACEI.Citation29 Although there are many possible explanations for the difference, it is clear from our study that the short-term vascular effects are different. It is not clear if they are sustained over a longer period and a long-term study needs to be carried out. However, it is certain that the effect of these two antihypertensive agents on arteries is different, even after the adjustment for SBP. This may have an important clinical relevance and it may further add to the evidence required to choose antihypertensive agents.
There are a number of limitations of this study. The sample size was small. However, the changes in PWV from the baseline were statistically significant (23.8% of reduction in PWV C-F with irbesartan and 10.6% with lisinopril after adjustment for SBP of 150 mmHg), despite the small number of patients involved, suggesting the importance of the effect of these two drugs on arterial compliance. It is important to note that PWV is not the only index of arterial compliance and other techniques should be used to confirm our results. However, PWV is known to be one of the most important and commonly used indices of arterial stiffness. A washout period between the two drug regimes at the crossover point of 12 weeks was not carried out, but this would not have influenced the final statistical analysis as the BP readings analyzed were adjusted for SBP of 150 mmHg. Arterial compliance was not measured after the 12 weeks period of the study. In such a small sample size, the power to detect any crossover effects may be difficult to establish, and a larger study is needed with adjustment for the carry over effects.
In conclusion, both an ARB and an ACEI improved arterial compliance in the central elastic arteries. Irbesartan improved the vascular compliance also in muscular arteries, suggesting an additive action of this class of drugs, independently of its effect on BP.
Acknowledgments
We would like to thank Peter Sacares and Winston Banya for their help with the statistical analyses.
Bristol-Myers Squibb provided an educational grant. They had no input in the trial design, day to day running, data collection, analysis or paper writing.
References
- National High Blood Pressure Education Program Working Group Report on Hypertension in the ElderlyNational High Blood Pressure Education Program Working GroupHypertension1994232752858125550
- Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP)SHEP Cooperative Research GroupJAMA1991265325532642046107
- DahlofBHanssonLLindholmLHScherstenBEkbomTWesterPOSwedish Trial in Old Patients with Hypertension (STOP-Hypertension) analyses performed up to 1992Clin Exp Hypertens1993159259397903578
- HavlikRJLaCroixAZKleinmanJCIngramDDHarrisTCornoni-HuntleyJAntihypertensive drug therapy and survival by treatment status in a national surveyHypertension198913I283122577459
- LehmanEDGoslingRGSonksenPHArterial wall compliance in diabetesDiabet Med199291141191563244
- LaogunAAGoslinRGIn vivo arterial compliance in manClin Phys Physiol Meas198232012127140158
- BenetosALaurentSAsmarRGLacolleyPLarge arterial stiffness in hypertensionJ Hypertens Suppl199715S89979218205
- BlacherJAsmarRDjaneSLondonGMSafarMEAortic pulse wave velocity as a marker of cardiovascular risk in hypertensive subjectHypertension1999331111111710334796
- CameronJDRajkumarCChristophidisNJenningsGLDartAMReduced systemic arterial compliance is associated with left ventricular hypertrophy and diastolic dysfunction in older peopleJ Am Geriatr Soc1997458038089215329
- LehmanEDGoslingRGSonksenPHArterial wall compliance in diabetesDiabet Med199291141191563244
- GuerinAPBlacherJPannierBMarchaisSJSafarMELondonGMImpact of aortic stiffness attenuation on survival of patients in end-stage renal failureCirculation200110398799211181474
- BalcherJGuerinAPPannierBImpact of aortic stiffness on survival in End-Stage renal diseaseCirculation1999992434243910318666
- CohnJNVascular wall function as a risk marker for cardiovascular diseaseJ Hypertens199917S4144
- GlasserSPArnettDKMcVeighGEFinkelsteinSMBankAJMorganDJVascular compliance and cardiovascular disease: a risk factor or a markerAm J Hypertens199710117511899370391
- WingLMReidCMRyanPBeilinLJBrownMAJenningsGLSecond Australian National Blood Pressure Study Group. A comparison of outcomes with angiotensin-converting-enzyme inhibitors and diuretics for hypertension in the elderlyN Engl J Med200334858359212584366
- NeutelJMSmithDHWeberMAEffect of antihypertensive monotherapy and combination therapy on arterial distensibility and left ventricular massAm J Hypertens200417374214700510
- ShargorodskyMLeibovitzELubimovLGavishDZimlichmanRProlonged treatment with the AT1 receptor blocker, valsartan, increases small and large artery compliance in uncomplicated essential hypertensionAm J Hypertens2002151087109112460705
- von zur MuhlenBKahanTHaggAMillgardJLindLTreatment with irbesartan or atenolol improves endothelial function in essential hypertensionJ Hypertens2001191813181811593101
- MahmudAFeelyJFavourable effects on arterial wave reflection and pulse pressure amplification of adding angiotensin II receptor blockade in resistant hypertensionJ Hum Hypertens20001454154610980584
- MahmudAFeelyJReduction in arterial stiffness with angiotensin II antagonist is comparable with and additive to ACE inhibitionAm J Hypertens2002151092109512460706
- SennSCross-over trials in clinical researchChichesterWiley19936069
- AsmarRBenetosATopouchianJLaurentPPannierBBrisacAMAssessment of arterial distensibility by automatic pulse wave velocity measurement: Validation and clinical application studiesHypertension1995264854907649586
- KnudsenSTAndersenNHPoulsenSHPulse pressure lowering effect of dual blockade with candesartan and lisinopril vs high-dose ACE inhibition in hypertensive type 2 diabetic subjects: a CALML II study post-hoc analysisAm J Hypertens20082113318268484
- KhderYBray-DesboscsLAliotEZannadFEffects of blood pressure control on radial artery diameter and compliance in hypertensive patientsAm J Hypertens1997102692749056683
- SlamaMSafavianATualJLLaurentSSafarMEEffects of antihypertensive drugs on large artery complianceNeth J Med1995471622188538819
- DahlofBDevereuxRBKjeldsenSELIFE Study GroupCardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenololLancet2002359995100311937178
- PittBSegalRMartinezFARandomised trial of losartan versus captopril in patients over 65 with heart failure (Evaluation of Losartan in the Elderly Study, ELITE)Lancet19973497477529074572
- PittBPoole-WilsonPASegalREffect of losartan compared with captopril on mortality in patients with symptomatic heart failure: randomised trial--the Losartan Heart Failure Survival Study ELITE IILancet20003551582158710821361
- HornigBLandmesserUKohlerCAhlersmannDSpiekermannSChristophAComparative effect of ace inhibition and angiotensin II type 1 receptor antagonism on bioavailability of nitric oxide in patients with coronary artery disease: role of superoxide dismutaseCirculation200110379980511171786
- FogariRZoppiAEffects of antihypertensive therapy on sexual activity in hypertensive menCurr Hypertens Rep2002420221012003702