 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
The potential importance of both prevention and personal responsibility in controlling heart disease, the leading cause of death in the USA and elsewhere, has attracted renewed attention. Coronary artery disease is preventable, using relatively simple and inexpensive lifestyle changes. The inexorable rise in the prevalence of obesity, diabetes, dyslipidemia, and hypertension, often in the risk cluster known as the metabolic syndrome, drives the ever-increasing incidence of heart disease. Population-wide improvements in personal health habits appear to be a fundamental, evidence based public health measure, yet numerous barriers prevent implementation. A common symptom in patients with coronary artery disease, classical angina refers to the typical chest pressure or discomfort that results when myocardial oxygen demand rises and coronary blood flow is reduced by fixed, atherosclerotic, obstructive lesions. Different forms of angina and diagnosis, with a short description of the significance of pain and silent ischemia, are discussed in this review. The well accepted concept of myocardial oxygen imbalance in the genesis of angina is presented with new data about clinical pathology of stable angina and acute coronary syndromes. The roles of stress electrocardiography and stress myocardial perfusion scintigraphic imaging are reviewed, along with the information these tests provide about risk and prognosis. Finally, the current status of gender disparities in heart disease is summarized. Enhanced risk stratification and identification of patients in whom procedures will meaningfully change management is an ongoing quest. Current guidelines emphasize efficient triage of patients with suspected coronary artery disease. Many experts believe the predictive value of current decision protocols for coronary artery disease still needs improvement in order to optimize outcomes, yet avoid unnecessary coronary angiograms and radiation exposure. Coronary angiography remains the gold standard in the diagnosis of coronary artery obstructive disease. Part II of this two part series will address anti-ischemic therapies, new agents, cardiovascular risk reduction, options to treat refractory angina, and revascularization.
Introduction
Atherosclerosis and its consequences: coronary artery disease, stroke, peripheral artery disease, and aortic and renal arterial disease are modern plagues of civilization. However, it should give us pause to learn that atherosclerotic lesions have been identified in 3500-year-old Egyptian mummies,Citation1 with mention of chest pain syndromes in hieroglyphics of papyruses, although certainly this was a negligible health concern at that time. Fast forwarding to this century, cardiovascular disease is now the most common cause of death, and evidence is now overwhelming that our diets and lifestyle are chief causes of obesity, diabetes, dyslipidemia and inflammation leading to atherosclerosis. The role of inflammation in etiology and as a potential therapeutic target is a topic of intense ongoing interest.Citation2–Citation8
Considerable data show that atherosclerosis and coronary artery disease (CAD) are preventable diseases. The data further indicate that population-wide dietary changes that include a plant-based, calorie controlled intake of fresh, whole foods low in sodium and sugar, avoidance of saturated and trans fats, together with a higher consumption of omega-3 fatty acids and perhaps olive oil, combined with adequate physical activity, could substantially eliminate the disease.Citation9,Citation10 Public health implications are compelling, but proven lifestyle recommendations remain unheeded.Citation11,Citation12
According to the latest American Heart Association (AHA) Statistics 2010,Citation11 overall prevalence of angina is 4.6% in the USA, affecting 10,200,000 persons, compared with a total number of 17,600,000 patients with CAD. Angina therefore afflicts 58% of patients with CAD.Citation11 Approximately 500,000 new cases are reported yearly, and prevalence rises rapidly with increasing age. While anginal attacks are considered reversible short term, they are by no means benign, with significant morbidity and mortality.Citation13,Citation14 New-onset angina, defined as beginning within 2–3 months prior to presentation, has a poor prognosis,Citation13,Citation15 with about 10% of patients experiencing a nonfatal myocardial infarction or coronary death during the next year.Citation16 While much of the data has been collected in men, it is now recognized that in women too, angina is not benign, with a 19% mortality rate within 4.5 years.Citation17
The expense involved in controlling angina is considerable, approaching $1.1 million per capita as a lifetime cost in 2006 dollars for women.Citation18 The estimated total direct and indirect cost of CAD for 2010 in the United States is about $177.1 billion. In weighing statistics, it should be emphasized that many millions of people with CAD remain undiagnosed, making the numbers, as striking as they are, actually conservative.
Definition
Angina, herein referring to angina pectoris, derives from the Latin angore, meaning choking and suffocation, but also anxiety, fear, or terror. Angina was recognized in the Middle Ages, but the description in 1768 by William Heberden is far better known.Citation19
Angina is chest discomfort caused by myocardial ischemia without necrosis, and is further qualified by its precipitating factors, time course to relief, and clinical characteristics, such as radiation and quality. Typical angina may be triggered by increased activity (exercise, sex), emotional stress (anger, fright, stress), or cold, wind, and fever. The discomfort of exertional angina is relieved by rest within 1–5 min, or more rapidly with sublingual nitroglycerin. Episodes last from 2–10 min. Classically there is heaviness or pressure retrosternally, with possible radiation to the ulnar aspect of the left arm, neck, jaw, mid-abdomen, right arm or shoulders. The average frequency of anginal attacks in patients is about 2 per week. Many patients voluntarily curtail their activities to avoid attacks.
Clinically, angina may be further subdivided according to common usage, as follows:
Chronic, stable
As described above, chronic stable angina is generally due to one or more significant obstructive lesions in coronary arteries, obstructive lesions defined as stenosis of ≥50% of the diameter of the left main coronary artery or stenosis of ≥70% of the diameter of a major epicardial vessel. Precipitating circumstances remain similar between episodes, thresholds may be predicted by patients, and relief patterns become known. Since stenoses are fixed, the angina is due to demand ischemia.
Decubitus
Attacks of decubitus angina occur upon recumbency, which raises end-diastolic volume, myocardial wall tension, and hence oxygen demand.
Nocturnal
Anginal discomfort awakens the patient, generally due to respiratory pattern changes, episodic tachycardia, hypoxia due to respiratory changes, or recumbency.
Refractory
Stable chronic angina is termed refractory when it is not controllable by a combination of maximal anti-anginal medication, angioplasty or coronary artery bypass surgery, or in whom the risks are unjustified.
Unstable (also called crescendo or rest)
Unstable angina (UA), is
○ of recent onset, and/or
○ discomfort is severe, and/or
○ occurs at rest or after minimal exertion lasting over 10 min, and/or
○ angina with a crescendo pattern – more frequent, more severe, of greater duration, or less responsive to nitroglycerin.
UA is an acute coronary syndrome (ACS), and when myocardial necrosis becomes evident from elevations in biomarkers, such as troponin I and troponin T,Citation20 the applicable clinical term becomes non-ST-elevation myocardial infarction, or NSTEMI, in the absence of ST-segment changes. The European Society of Cardiology defines ACS as acute chest pain (ie, chest pain at rest > 20 min within the prior 48 hours) together with electrocardiographic (ECG), changes suggesting myocardial ischemia and/or elevation of cardiac markers.Citation21 About 1.35 million patients are admitted to US hospitals annually with the diagnosis of unstable angina-NSTEMI. From 38%–47% of patients with ACS have ST-segment elevations on the ECG, known by the acronym STEMI.
Microvascular (also called Syndrome X)
More common in women, angina-like pain, normal coronary angiograms, and positive exercise tests, sometimes with perfusion defects, are a basic diagnostic triad in microvascular angina.Citation22 Response to nitrates and other anti-ischemic agents is less reliable, and hormonal abnormalities, changes in pain perception with exaggerated sensitivity, insulin resistance, and psychological overlays may be modifying factors. Endothelial dysfunction is one pathophysiological suspect,Citation23 but release of vasoactive substances, autonomic dysfunction, vascular smooth muscle dysfunction and loss of estrogen may all contribute. Chest pain may occur under conditions of cardiac stress without evidence of ischemia. GERD and esophageal motility disorders are common comorbidities. In part, treatment is difficult because therapeutic responses are not sustained. About 1% of patients die and 0.6% suffer a stroke within one year after their first hospital admission.
Vasospastic (also called Prinzmetal’s, or angina inversa)Citation24,Citation25
Described in 1959, this variant form of angina occurs at rest, often at night, or with exertion, is caused by focal vasospasm of an epicardial coronary artery, and is not due to obstructive atherosclerotic lesions. Prinzmetal’s angina is known for transient elevation, rather than depression, in ST-segments on the electrocardiogram, although either may occur. However, most acute patients with coronary vasopasm do not have ST-segment elevations, which are identified more often during an attack or upon provocative testing. Despite an increase in ventricular arrhythmias in some patients, the prognosis is generally better than those with fixed, significant obstructive lesions, although response to treatment may be poor.Citation26 In the CASPAR study, every fourth patient with an ACS had no culprit lesion at coronary angiography, and in those patients epicardial coronary spasm could be documented in 50%.Citation27 Coronary vasospasm is a more common cause of chest pain and ACS than formerly believed, and may contribute to pathology with or without coexisting obstructive plaques, more frequently found in men.Citation28 Over the years, vasospasm has been linked to low intracellular magnesium levels, hyperinsulinemia, defective focal nitric oxide production, and use of tobacco or cocaine.
Atypical angina
Patients with nonclassical symptoms and signs, such as absence of substernal location and character, exertional trigger, or typical relief with rest or nitroglycerin, are grouped under the term atypical angina. Atypical presentations are more frequent in women and diabetics, displaying variable pain intensity or thresholds, timing, and characteristics. Palpitations, sharp lancinating or back pain are confounding complaints. The more atypical the presentation, results of testing, and responses to provocation or therapy, the greater the probability of misdiagnosis and a poor outcome (see below).
Silent ischemia and anginal equivalents
In some patients, particularly diabetics and the elderly,Citation29 myocardial ischemia may cause symptoms other than precordial discomfort. These may include dyspnea, diaphoresis, nausea and emesis, fatigue, weakness, altered sensorium, light headedness, and fainting. In the absence of chest pressure, heaviness, pain or sensorial cognition, ischemia is also called silent. Altered pain perception and presence of autonomic neuropathy may modulate symptom expression. Patients with silent ischemia are less likely to be diagnosed correctly and receive appropriate attention and treatment, resulting in poorer outcomes. In fact, even if there are clear objective findings, such as subsequent ST-segment elevation, the absence of chest pain during the initial presentation still decreases utilization of both fibrinolysis and percutaneous coronary intervention (PCI) later on in such patients’ treatment.Citation30
Diagnosis
Although about 25% of people experience chest pain,Citation31 77% of them do not seek medical care despite widespread public educational efforts.Citation30 The number of patients presenting with chest pain eventually found to have CAD ranges from 11 to 39%,Citation23 but reports trend closer to 12%.Citation23 Of those seen in emergency rooms, about 45%–50% will have a cardiac etiology,Citation30,Citation32 with the remaining 50%–55% diagnosed with noncardiac chest pain.Citation31 In primary care practices, however, the most common conditions encountered are gastroesophageal reflux disease (GERD), musculoskeletal pathology, other gastrointestinal conditions, panic disorder, pulmonary disease, and stable chronic angina.Citation33,Citation34 Ischemic pain is often neglected by patients who mistakenly attribute the pain to an episode of indigestion or gas. Characteristically this history is elicited retrospectively after it is clear the patient has ischemic heart disease.
Questions to ask about chest pain include:Citation35
Background, character, and development of the symptoms. For instance, whether pain occurred during effort, an acute febrile illness, after trauma.
Area involved, with radiation, if any.
For instance, requesting that the patient point to the area of pain with a finger may help with focus and elicit a response of a clenched fist.
Triggers that initiate the pain.
For instance, whether pain occurred during effort, emotional stress, sports events on TV, position, eating, etc. The threshold of pain may be lower after smoking, eating, or cold weather.
Frequency, progression, and duration of the pain.
Factors that relieve the pain.
For instance, variation of pain with rest, maneuvers, position, eating, eructation, antacids, proton pump inhibitors, nitroglycerin.
The precipitating factors, characteristics, and natural course of angina, along with antecedent history, are typically of greater value in evaluation than the physical examination, which is normal in most patients. Discomfort is usually described as heaviness, tightness, crushing, squeezing or pressure in the precordial, substernal or even epigastric area, much more common than peripheral radiation, with or without numbness. It is said that radiation to the arms, diaphoresis and hypotension suggests myocardial infarction. Angina does not vary with change in position, the respiratory cycle or cough. Angina reported postprandially is not usually of differential diagnostic value. Angina or any equivalent, including absence of pain during silent ischemia, may be accompanied by dyspnea, nausea, diaphoresis, weakness/fatigue and apprehension. Therefore, any patient of appropriate age with naked, unexplained weakness, dyspnea, or nausea, particularly precipitated by activity, sex, or emotion, should be investigated for ischemic heart disease along with other usual possible etiologies.
Angina must be differentiated from other causes of chest pain, the most common summarized in .
Table 1 Some noncoronary causes of chest pain
Production and significance of pain
Myocardial ischemia stimulates cardiac sensory receptors to initiate a sympathoexcitatory reflex. Bradykinin, protons, and other substances released during ischemia activate the vallinoid receptor 1 (VR-1) on capsaicin-sensitive cardiac sensory nerves (unmyelinated [type C] or thinly myelinated [A-δ] fibers).Citation37 The VR-1 receptor acts as a transducer responsible for sensing tissue ischemia, and through sympathetic activation, leads to the sympathoexcitatory reflex and the pain of angina.Citation38
Simultaneously, cardiac sensory nerves also release neuropeptides, among them calcitonin gene-related peptide, substance P (SP), and neurokinin A, believed to modulate myocardial ischemia/reperfusion injury.Citation39 By dilating the coronary arteries and through their negative inotropic and chronotropic actions, they could reduce negative ischemic effects, in part mediated by raised amounts of nitric oxide produced by secondary actions of SP.Citation40 Considerable data now support an increasingly popular view that VR-1 receptors protect the heart during ischemia.Citation41,Citation42 Cardiac afferents from the first four thoracic spinal neurons, after interacting with other nerves and signals from descending supraspinal locations, ascend along spinothalamic afferents to the thalamus on their way to the cerebral cortex. Anxiety and/or stress, frequently associated with CAD, upregulate glucocorticoid release and increase sensitization to cardiac nociceptive stimuli by modulating upper thoracic neuronal activity.Citation43 Awareness of the pain may be variable, in part due to an interpretive component in the cortex.
It is possible that diabetics have more severe ischemia related to neuropathy because their VR1 sensitivity and SP production are impaired. Preclinical studies also suggest that a reduction in nerve growth factor in diabetics may account for failure to experience pain.Citation44 Some evidence exists that central processing of afferent pain signals from the heart mediates lack of pain in patients with silent ischemia. Pain messages are, however, physically received by the brain in these patients.
In the light of this new information, angina appears to serve as a warning to the patient to stop activity that may further ischemic damage and obtain medical care, but simultaneously initiates some degree of myocardial protection.
Silent ischemia
Silent ischemia is angina without pain, a unique clinical challenge.
While angina is considered a common diagnosis in clinical practice, it is highly likely that prevalence rates remain underestimated. Asymptomatic and hence undiagnosed myocardial infarction accounted for 33% of transmural (Q-wave) myocardial infarctions identified by serial electrocardiographic changes and 22% of all nonfatal infarctions in the Honolulu Heart Program.Citation45 Recently, using a delayed enhancement cardiac MRI (DE-CMR), which identified both Q-wave and non-Q-wave myocardial infarctions, a study was conducted in 502 subjects with extracardiac atherosclerotic disease or advanced risk factors for CAD but without symptoms.Citation18 An unrecognized myocardial infarction was identified in 13.1% of men and 3.7% of women. There was also a suggestion that silent events were associated with a poorer prognosis. In the elderly, from 21% to 68% of all myocardial infarctions are asymptomatic or unrecognized as determined by electrocardiography.Citation18,Citation46,Citation47 In high risk patients evaluated with dual-isotope myocardial perfusion SPECT, silent myocardial infarction is also common.Citation48
Additionally, silent ischemia is surprisingly frequent during continuous electrocardiography, exercise testing, or stress echocardiography in high risk patients in a variety of clinical situations. Up to 75% of ischemic (ST-segment depression ≥1 mm for ≥1 min) episodes may occur without pain.Citation49 When clinical symptoms of stable angina are thought to be controlled, at least 40% of those patients continue to show ischemia on monitoring.Citation50 The longer patients continue to be monitored, the greater the number of ischemic episodes that are detected.Citation51
All things considered, it is becoming evident that most ischemic cardiac events are asymptomatic and unrecognized, even in patients with typical stable angina who consider themselves extremely aware. From 10%–20% of diabetics have silent ischemia and the burden is rising. From the significant number of silent myocardial infarctions found on electrocardiography and MRI, and asymptomatic ischemic episodes during exercise provocation or ambulatory ST-segment monitoring, a great number of would-be anginal attacks also go unrecognized, undiagnosed, and undertreated. Hence the clinical reporting of anginal episodes is quite insensitive. Since continuous ECG monitoring is also underutilized, the clinical implications are immense.
Patients with silent ischemia have a poorer prognosis than those with classical symptoms and may require more aggressive therapy.Citation49,Citation52,Citation53 Just one or a few episodes of ST-segment depression on 24 hour continuous monitoring is associated with a 7.43 rise in risk of AMI or death at 30 days in patients with unstable angina.Citation52,Citation54 Silent ischemia remains a formidable unsolved clinical problem in all its guises,Citation55–Citation58 not only with respect to the absence of anginal pain. In medicine, random, instant, “snap-shot”, or “ice-pick” samples of elements of disease, even as deceptively simple as blood pressure or serum glucose measurements, may be disastrously misleading when compared to continuous recordings.
Classification and grading
Symptom intensity does not necessarily reflect severity or extent of coronary obstruction, but assessment is helpful and included in current guidelines.Citation59 Angina is classified with respect to functional capacity by the New York Heart Association functional classification, and according to severity by the Canadian Cardiovascular Society ().
Table 2 Classifications of functional capacity and severity in angina patients
The Canadian Cardiovascular Society classes correspond to the exercise tolerances, shown in , in metabolic equivalent units, MET:Citation62,Citation63
Table 3 Exercise capability corresponding to Canadian Cardiovascular Society Functional Classifications
Pathophysiology
Myocardial energy (oxygen) balance
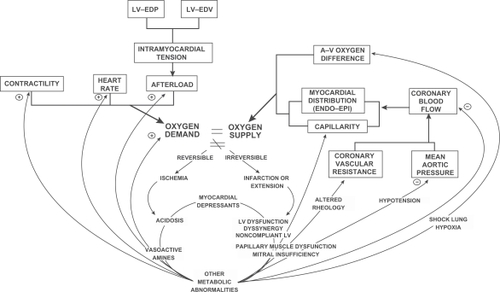
For over 40 years, it has been recognized that myocardial ischemia results from an imbalance between myocardial energy supply, from insufficient sources of oxygen and substrate (glucose, free fatty acids), and myocardial oxygen demand.Citation64–Citation67 Usually this is simply referred to as an imbalance between myocardial oxygen supply and demand, but it should be clear that substrate supply, utilization, and enzymatic activities, along with other variables involved in intermediary metabolism and mitochondrial function, play a major role in the pathogenesis of myocardial ischemia in angina, acute coronary syndromes, and during reperfusion ischemic injury ().
Figure 1 Global relationships and positive feedback loops relating to the inequality of myocardial oxygen supply and demand.
Many of the global relationships and positive feedback loops relating to the inequality of myocardial oxygen supply and demand have not changed in many years, although molecular, electrophysiological, conceptual, and technological advances have been considerable. Myocardial energy imbalance is central to all ischemic syndromes: angina, myocardial infarction, and cardiogenic shock. The variables determining myocardial oxygen supply (right) are altered by negative feedback loops from complications of poor left ventricular function (center, lower cycle). Those factors affecting myocardial oxygen demand (left, as heart rate, afterload, preload, contractility) are altered by positive feedback loops from those events perpetuating systemic features. An increase in left ventricular end-diastolic pressure (LV-EDP) or volume (LV-EDV) increases preload according to LaPlace’s Law. Both the negative feedback on oxygen supply and the positive feedback on oxygen demand tend to further the inequality between the two and may jeopardize poorly perfused myocardial tissue. When ischemia progresses beyond the reversible stage of angina and myocardial necrosis follows, well-known hemodynamic, metabolic and mechanical sequellae may occur. Reproduced with permission from Kones, 1973.Citation65
The production of useable energy in the form of ATP is determined by the degree of oxidative phosphorylation (including nutrient supply) and oxygen availability; hence, the two are inexorably intertwined. Major determinants of myocardial oxygen demand are heart rate, blood pressure, and myocardial wall tension, in turn influenced by preload, afterload, and contractility. Since myocardial oxygen extraction from coronary arterial blood at rest is normally high, about 75% of arterial oxygen content,Citation68 adjustments in oxygen extraction cannot correct an imbalance. Physiological increases in myocardial oxygen needs are normally provided by rises in coronary blood flow.
Coronary autoregulation
Ability of coronary arteries to increase flow to meet myocardial metabolic demand, called coronary flow reserve, is about 4–6 times the resting value at maximum dilatation of the coronary arteries,Citation68,Citation69 which can be somewhat expanded pharmacologically. Coronary autoregulation is a complex phenomenon with many regulating variables.Citation70 Superimposed upon the hierarchy are the influences of disease upon each variable – atherosclerosis, ischemia, hypertrophy, alterations in autonomic nerve function, endothelial function, electrophysiology, etc.Citation71 Up to 95% of the resistance in coronary vessels arises within small intramural vessels, about 10 nm to 140 nm in diameter, which are not visualized during coronary angiography or multislice CT angiography, a procedure identifying epicardial arteries with diameters from a few mm to about 500 μm (arterioles with a diameter <100 μm and prearterioles with diameters from ∼500 μm to ∼100 μm are below the resolutions of angiography and are not visualized).
About 5% of the resistance that determines coronary blood flow arises within the conductive epicardial coronary arteries. Resolution limitations of coronary angiography pre-clude assessment of pathology in the important microvascular bed, where alterations are common in ischemic heart disease, hypertension, diabetes, and autoimmune vascular pathology. The microvascular bed may respond to therapies differently than epicardial vessels.Citation72 In considering that about 30% of patients referred for coronary angiography have normal or nonactionable reports, it is understood that the vast microvascular bed has not been evaluated. When angiography is used to assess accuracy of stress perfusion or echocardiographic testing, these limitations are pertinent.Citation73 Measurement of blood flow using positron emission tomography is a useful tool in assessing coronary dynamics, especially in combination with other imaging techniques.Citation74 A more aggressive stance in treating ischemic heart disease (IHD) requires an improved, detailed understanding of the microvasculature.
In patients with stable angina, a fixed reduction in the diameter of coronary arteries by at least 70% dictates an obligatory reduction in coronary blood flow in one or more coronary arteries. The inability to increase oxygen extraction or coronary blood flow, together with elevated myocardial energy demand, leads to anginal pain, variably accompanied by panoply of metabolic, electrophysiologic, and hemodynamic consequences. Most events that trigger angina do so by changing myocardial oxygen demand, viz, increases in heart rate (jogging, sexual activity), afterload (doing a difficult bench press, not taking blood pressure medication), preload (consumption of a sodium-loaded pizza by a patient with heart failure and CAD), or contractility (in part, watching an exciting sports event or explosive anger with subsequent catecholamine discharge). Similarly, the beneficial effects of most maneuvers that relieve angina may be explained through corrective alterations in the determinants of myocardial oxygen supply and demand.
Endothelial dysfunction within atherosclerotic coronary arteries is abnormal, and nitric oxide production may be reduced and contribute to myocardial oxygen imbalance.
Clinical pathology
Over the past few years, an important distinction between the pathology of acute and chronic coronary syndromes has been made. In the patient with chronic coronary artery disease and fixed obstructive coronary lesions, sudden increases in myocardial oxygen demand, usually due to effort, in face of the inability to raise myocardial blood flow and oxygen supply, result in a transient myocardial energy imbalance and demand ischemia. The fixed areas of stenosis responsible are those which are likely to be seen on coronary angiography. In contrast, the majority of patients with an acute coronary syndrome suffers sudden reduction of coronary blood flow due to a discrete plaque event: rupture, erosion, or hemorrhage in a vulnerable plaque.Citation75 A physical disruption in the plaque exposes platelets to collagen, initiating adhesion and aggregation, while tissue factor in plaque induces coagulation, and thrombus formation ensues with variable degrees of arterial obstruction. Vulnerable plaques may not be visualized during coronary angiography. Subclinical microembolism, smooth muscle hyperreactivity, and endothelial dysfunction may also contribute to progression of the syndrome. Many fatal intraarterial occlusions arising from plaque rupture do not occur at highly stenotic areas in coronary arteries. After myocardial infarction, since prognosis is significantly determined by the amount of muscle destroyed during ischemia/reperfusion,Citation66,Citation76 ensuring vessel patency and limiting injury to preserve myocardium are the overriding concerns.
Not every plaque disruption causes a total arterial occlusion or even clinical manifestations. Rather, the process is ongoing, involving inflammation, thrombosis, reabsorption of thrombus, fibrosis and remodeling of the plaque over time that determines whether coronary blood flow will continue unimpeded. The processes of thrombus dissolution, organization, plaque cell and lipid accumulation and synthesis of extracellular matrix cannot be predicted. An inflamed plaque with intense oxidative stress may continue to enlarge its lipid pool and accumulate inflammatory cells that produce excessive amounts of protease,Citation77 resulting in a thin, friable, fibrous cap. The metalloproteinases in particular, expressed by macrophages and smooth muscle cells within plaques, degrade matrix collagen and elastin. In contrast, the plaque may stabilize and remodel inward during healing, decreasing its lipid pool, accumulate extracellular matrix, thicken its fibrous cap, and maintain a variably patent lumen. Alternatively, vulnerable plaques may rupture, heal, become relatively stable, but then shrink (negative remodeling) causing stenosis and low blood flow requiring revascularization.Citation78 Lesion evolution and progression include organizing thrombi from otherwise lethal ruptures that may remodel and heal well. Outward expansion of evolving plaque (positive remodeling) may limit luminal encroachment, but is paradoxically associated with vulnerable unstable lesions containing large lipid cores rich in macrophages. The lesion considered most vulnerable is the thin-cap fibroatheroma with a large necrotic lipid core (>34% of plaque area) and a thin fibrous cap (thickness <65 μm). However, plaque remodeling is heterogeneous, involving intra-plaque hemorrhage and erosions of fibrous plaques. Recent information suggests that erosions rather than ruptures and may occur in the young, particularly women, who succumb to sudden coronary death.Citation79 Erosions may be even less identifiable on stress testing and coronary angiography, and may result from repeated coronary vasospasm. Distal microembolization as a later complication of thrombosis is also of interest.Citation80
Differences in plaque from patients with chronic stable angina and acute myocardial infarction have been reported using optical coherence tomography (OCT) imaging to assess plaque vulnerability.Citation81 Acute myocardial infarction (AMI) survivors who were undergoing percutaneous interventions and those with stable lesions in multiple vessels had OCT images performed of infarct-related lesions or lesions slated for revascularization, as well as noninfarct-related and nontarget lesions. OCT images found intracoronary thrombus in all patients with AMI, and none in stable angina patients. Plaque rupture was identified in 77% of AMI patients, but only in 7% of stable angina patients. Thin-cap fibroatheroma were much more common in the AMI patients, not only in infarct-related culprit lesions, but in others as well. The authors concluded that thin caps were part of a diffuse inflammatory process in patients with acute events. Rates of plaque rupture in noninfarct-related lesions in AMI patients and nontarget lesions in stable angina patients were similar.
The myocardial oxygen imbalance of chronic stable angina is characteristically reversible short term and unassociated with myocardial necrosis. In contrast, the extent of the imbalance in acute coronary syndromes generally produces muscle cell death. To help begin decide which it is, even imperfectly, the American College of Cardiology/American Heart Association (ACC/AHA) guidelines advise a resting electrocardiogram (ECG) be done in all patients with symptoms of angina.Citation59 The ECG will be either normal or nondiagnostic about half the time, and false positive and negative findings in patients with angina abound. In half of such patients with a normal resting ECG, one recorded during chest pain may reveal a significant change. Even advanced CAD may be present with a normal ECG.
Interventions that reduce cardiometabolic risk, to be discussed in Part II of this review, may promote plaque stabilization by lowering inflammation, oxidation, and suppress the thrombotic cascade. Many nonpharmacological and some pharmacological treatments, especially statins, are pleiotropic in the sense that they not only improve lipid profiles, but also act in other ways to impede inflammation and destructive events.Citation82
Pretest stratification and probability of ischemia
The three elements of typical angina include
substernal discomfort with location, characteristics and duration as discussed above,
provocation by effort or emotional stress, and
relief by rest or nitroglycerin.
The likelihood that a patient will have a firm diagnosis of CAD or obstructive lesions on coronary angiography from the clinical description of chest pain varies according to age, sex, and number of these three typical elements in the presentation. For instance, at age 45, if the history contained all three criteria, 87% of men would have CAD, but only 55% of women.Citation59,Citation83 If the history contained two elements, ie, were atypical, these would be 51% and 22%, respectively. If the chest discomfort described had none of the three elements, ie, were noncardiac, 13% of men and 3% of women would have CAD.
A few patients with obstructive CAD in fact would be missed clinically. Women have significantly less obstructive CAD than men at the same age, and even when the history is negative for ischemia, there will be some patients who will have CAD in all groups.
At age 65, if all three elements of typical angina are present, 94% of men and 86% of women will have CAD. If no elements are present, ie, the chest pain is noncardiac, 27% of men and 14% of women will have CAD. As age increases, the correlation between the number of typical elements and diagnosis rises. As women age, especially beyond menopause, a greater proportion of those presenting for care will have demonstrable obstructive lesions than younger women.
The probability of ischemic heart disease
An assessment of the pretest probability of ischemic heart disease (IHD) is required for a decision about further testing.
If pain lasts > 20 min at rest, reproduces pain previously documented as angina, and/or there is associated transient mitral regurgitation, diaphoresis, hypotension, or pulmonary rales, the probability of ischemia is high.
If there is new ST-segment deviation ≥ 0.5 mm, T-wave inversion ≥ 2 mm, new left bundle branch block or a serious ventricular arrhythmia, an ischemic origin is likely.
Elevations in cardiac biomarkers indicate myocardial necrosis and reclassify the patient by definition.
Features suggesting an intermediate probability of ischemic origin include absence of the above, pain > 20 min but abated with rest or nitroglycerin, male gender, age over 70 years, presence of diabetes, extracardiac vascular disease, fixed Q waves, and resting ST depression ≤ 1 mm in multiple lead groups. While the presence of left ventricular hypertrophy somewhat raises probability of associated ischemia, it is not diagnostic. Similarly, while the finding of several traditional risk factors is of interest and to be weighed, severe CAD may be present without them.
Features arguing for a low likelihood of an ischemic origin exist if
none of the findings above are present,
the patient has used cocaine prior to the episode or there is a documented history of recurrent panic attacks and/or hyperventilation with similar pain,
there is chest wall tenderness, and/or
the ECG is normal, shows T-wave flattening, or T-wave inversions in leads with dominant R waves.Citation84
None of these features are diagnostic.
Placing great predictive value upon one feature of the presentation may lead to a diagnostic error, for without a coronary angiogram, the possibility of obstructive CAD always remains open. New angina may also occur in patients who have histories of common diseases well known to mimic angina, such as GERD, esophageal spasm, peptic ulcer, and cholecystitis, all of which may be indistinguishable clinically. Although the differential diagnosis is familiar to physicians, errors remain a frequent subject of lawsuits. Up to 12% of patients who are discharged from emergency departments (EDs) with a noncardiac diagnosis have had or will sustain an AMI.
New imaging techniques, especially in EDs, and biomarkers currently available for both AMI and rule out diagnoses now offer greater assistance in improving accuracy of diagnosis and treatment.Citation85,Citation86 For instance, the use of new high sensitivity troponin assays, hs-cTnT, properly used, provide sooner exclusion and potentially improved identification of myocardial necrosis.Citation87–Citation91 In addition, the increasing use of chest pain units in hospitals may improve patient outcomes and possibly reduce inappropriate hospital admissions.Citation92–Citation94
By following applicable guidelines and pursuing objective data to confirm clinical impressions, the careful physician will avoid many of the common pitfalls in clinical decision making leading to misdiagnosis and/or mistreatment.
Diagnostic studies
The choice of how to proceed depends upon the individual patient, and also reflects the two objectives of noninvasive testing. For those with new onset chest pain, the need for diagnosis predominates, and the question to be answered is whether or not ischemia due to obstructive atherosclerotic lesions is present. In established patients, the dominant issue is risk stratification and whether coronary angiography is needed for further management.
Exercise ECG testing
In general, most patients – all but those with extremely low probabilities of an ischemic origin of their chest pain – should receive graded exercise testing, particularly if the resting ECG is normal. The Bruce protocol and Duke Treadmill Score are commonly used. Patients must be able to exercise adequately, and be free of confounding features precluding interpretation on the resting ECG.Citation95 The test may reveal typical changes of ischemia on the ECG in association with chest pain, which clarifies the diagnosis, and the patient’s exercise capacity may provide further direction in treatment. Together with the Duke Treadmill score, exercise testing gives predictive information concerning survival. Exercise tests are most valuable when there is an intermediate probability of CAD, according to Bayesian theory, and are recognized by the ACC/AHA Task Force on practice guidelines as an important asset in such patients for clinical decision making.Citation59 However, when the probability of CAD is high, the exercise test may be indicated for risk stratification, prognosis and clinical direction.Citation83
Exercise tests are not indicated in patients with preexcitation syndromes, those that are being paced, have complete left bundle branch block (LBBB), over 1 mm of ST segment depression at rest, a myocardial infarction within the previous two days, unstable angina, pericarditis, active ECG changes, severe aortic stenosis or lung disease, ongoing poorly controlled arrhythmias, uncontrolled hypertension, active cerebral ischemia or embolic phenomena, advanced lung disease, heart failure, aortic dissection, myocarditis/endocarditis, or other major unresolved problems. Generally β-blockers, nodal blockers, and nitrates are discontinued about two days before testing and digoxin about one week beforehand. The test should be aborted if there is chest pain, severe dyspnea, dizziness or near syncope, fatigue, ST elevation ≥ 1 mm without diagnostic Q waves, ST depression ≥ 2 mm, fall in systolic BP > 10 mmHg, or a ventricular arrhythmia.
An exercise test is positive for ischemia if any of the following occur:
New flat or downsloping ST-segment depression ≥ 1 mV below the baseline, at least 0.06–0.08 sec after the QRS complex J-point in multiple leads, the most reliable indicator of ischemia.Citation95 If it appears during a low workload, prognosis may be worse.
New ST-segment depression at the start of exercise (within 3 min);
ST-segment depression persists beyond 6 min of the recovery phase;
Fall in systolic blood pressure during exercise (normally this rises because of increased stroke volume);
Development of acute heart failure or sustained ventricular arrhythmias. Significant ventricular ectopy during recovery has greater significance than ectopy during exercise.
Development of characteristic chest pain during exercise;
Inability to exercise more than 2 min on a cardiac basis.
The exercise test is imperfect, with false-negative and false-positive results one-third of the time, but is useful, inexpensive, widely available, simple and practical. For instance, if the test is positive in a male with a history of classical angina, he develops chest pain during the test, and is over 50 years of age, there is a 98% probability he has advanced CAD. On the other hand, with limited sensitivity, a negative test strongly argues against more ominous forms of CAD such as three-vessel or left anterior descending coronary obstruction, but certainly does not exclude CAD. The sensitivity and specificity is 68% and 77% respectively.Citation96,Citation97 Specificity is reduced in middleaged females, with a false positive rate of 17% compared to 11% in males.Citation98
Some investigators believe the overall accuracy of ST segment depression on exercise ECG testing is only about 65%.Citation99,Citation100 For this reason an additional scoring system using three independent variables: exercise time; ST segment deviation; and angina index has been used extensively, and was incorporated into the ACC/AHA Guidelines for exercise testing.Citation96 The Duke Treadmill Score (DTS) quantitates risk, assists with prognosis, and is calculated as followsCitation101
where the angina index is
0 if no angina occurs anytime,
2 if angina is the reason for stopping the exercise test, and
1 if angina occurs during the test or during the recovery period.
If DTS is ≥5, risk is low, the associated 4 year survival is 99%, and such patients should be managed medically. If DTS is <(−10), risk is high, the 4 year survival is 79% with an average mortality of 5%, and such patients should be referred for coronary angiography. Approximately 4% of patients have high risk DTS, and about two-thirds of patients have low risk DTS ().Citation101
Table 4 Duke Treadmill scores (DTS), survival, and annual mortality
Patients with overtly positive exercise tests should undergo cardiac catheterization with revascularization in mind. Further indications, precautions, contraindications, caveats, interpretation criteria, and details of exercise testing are given in the full ACC/AHA guidelines.Citation96,Citation102
Stress imaging
Stress imaging includes myocardial perfusion, stress echocardiography, and other techniques.
Compared to exercise electrocardiography, perfusion imaging with 201thallium or 99mtechnetium-sestamibi raises sensitivity, but prognostic value is less established.Citation102 Perfusion imaging is particularly useful when the resting ECG is abnormal, in women because of false positives on stress ECG,Citation103 and in symptomatic patients who have had prior revascularization, reversible areas of ischemia may be quantified and localized to specific areas of the myocardium.Citation104
99mTechnetium-sestamibi produces better and faster images with decreased attenuation, has lower sensitivity for viable myocardium than 201thallium, and is more expensive.
Increased lung uptake post testing, left ventricular dilation, and multiple perfusion defects are associated with left main coronary or severe multivessel disease and should be followed by coronary angiography. Patients with two or more perfusion defects and ventricular dysfunction are also candidates for angiography. Use of perfusion imaging has been found to lower rates of hospital admission by up to 52% while evaluating acute chest pain in the emergency department.Citation105
A number of patients who require stress testing are unable to exercise, most frequently due to peripheral vascular disease, a prior stroke, arthritis, lung disease, neurological disorders, or simply deconditioning in the elderly. In this circumstance pharmacological challenge is performed using dipyridamole, adenosine, or dobutamine. Dipyridamole and adenosine raise blood flow in healthy coronary arteries, stealing blood from myocardium served by obstructed vessels. After administration of either of these two agents the perfusion imaging study is performed. Dipyridamole may cause bronchospasm and is not used in asthmatics. Xanthines may cause false-negative studies. Adenosine may produce flushing, dyspnea, chest pain, and bradyarrhythmias, and cannot be used in a patient with sick sinus syndrome or high grade AV block. Alternatively, a graded infusion of dobutamine may be used to raise myocardial oxygen demand prior to perfusion imaging, and is useful in patients who cannot raise their heart rates adequately during exercise.
If the initial evaluation of the patient with angina suggests heart failure, pulmonary hypertension, valve disease or hypertrophic cardiomyopathy, echocardiography may be considered. In addition, baseline or follow-up measurement of systolic or diastolic function may be of value in rehabilitation. Echocardiography may be also used with or without exercise or pharmacological stress to reveal segmental wall motion abnormalities associated with ischemia. Stress echocardiography is more sensitive than stress electrocardiography. Exercise makes normal myocardium hyperdynamic, but ischemic walls become hypokinetic or akinetic. Accuracy is comparable to perfusion imaging, not as widely available, and less expensive. Since it is the only stress technique that evaluates ventricular function, valve disease, and cardiac dimensions, it has special value in patients with aortic stenosis, idiopathic hypertrophic subaortic stenosis, or changing murmurs.
Magnetic resonance coronary angiography (MRCA) is an exciting and promising addition to cardiac imaging.Citation106–Citation109 While useful in the emergency department for triage, information derived is primarily anatomic rather than functional or predictive; present limitations will no doubt be improved with further research and development.Citation110 Both MRCA and computed tomographic coronary angiography (CTCA) are effective as rule-out techniques but remain imperfect. Radiation exposure and need for contrast with CTCA detracts from long term interest. An excellent authoritative review of both techniques is available,Citation111 and recent criteria for appropriate cardiac radionuclide imaging with further details are summarized in a consensus statement.Citation112
Current guidelines clearly indicate that in most patients a noninvasive test should be performed prior to coronary angiography, but in about 15% of cases, it is not done.
has a comparison of sensitivity, specificity, and predictive accuracy of noninvasive tests currently used for diagnosis and stratification of patients suspected of having coronary artery disease.
Table 5 Tests used for diagnosis and prognosis in ischemic heart diseaseTable Footnote*
Risk stratification after noninvasive testing
Evidence based guidelines stratify patients into three categories: high, intermediate, and low, for clinical decision making and advising patients about their choices.Citation59 Inclusion criteria for these categories based on noninvasive testing are summarized in .
Table 6 Risk stratification based upon noninvasive testing in patients suspected of having ischemic heart disease
Coronary angiography
Coronary angiography remains the gold standard for the diagnosis of CAD, and defines the location(s) as well as the extent of the disease. As mentioned, it should be performed in patients with angina who have a markedly positive stress test, but also in those in whom testing strongly suggests left main coronary artery or three-vessel disease. Other indications include patients who may have a nonatherosclerotic cause of ischemia such as a coronary arterial anomaly, those who have frequent readmissions for chest pain, who are resistant to medical therapy (disabling angina despite optimal evidence based medical management), who have undergone prior revascularization procedures, those with indeterminate stress tests and clinical features of severe CAD, those with heart failure, some patients who are unable to proceed with noninvasive evaluation, or whose occupation demands a definitive diagnosis.
Coronary angiography also refines prognosis. In patients referred for angiography and subsequently treated medically, in those who had three-vessel disease, the 12 year survival was 40%; in those with two-vessel disease, it was 59%; in patients with one vessel obstructed, 74%; and in patients with normal coronary arteries, there was 91% survival over the same period.Citation113 Extent and location of obstruction may be precisely quantitated; when lesions are proximal, prognosis is worse. Simultaneously, left ventricular function, a critical determinant of prognosis, may also be accurately characterized. Coronary angiography provides precise information about two of the four most important predictors of long term survival: left ventricular systolic function and extent and distribution of obstructions. Unfortunately, however, it does not quantify plaque stability and probability of rupture, a third determinant of outcome and a topic of great current interest. The fourth determinant of risk and prognosis of patients with ischemic heart disease is general health and extra-coronary comorbidity.Citation59
Use of coronary angiography as a screen, especially in symptom free patients, has been criticized because of low diagnostic yield, with up to 38% of “negative” studies, in view of the radiation exposure and potential adverse events.Citation199 However, a normal result does not imply that a procedure is not indicated or is overutilized. When used appropriately according to current decision guidelines, both the negative as well as the positive information obtained is necessary for optimal management. Such discussions about overuse of coronary angiography do not apply to the urgent evaluation of chest pain, or to patients with known CAD, in whom potential benefits clearly outweigh potential procedural risks. The high frequency of false negative coronary angiograms in some subsets of patients only underscores the need for improving the diagnosis of obstructive CAD, following guidelines, and continuing the search for additional data and new techniques.
Gender differences in CAD
Gender differences in CAD are now acknowledged and recognized, but not yet fully characterized or incorporated.
Angina is the most common symptom of IHD in women. Age, gender, ethnic, regional and socioeconomic differences in patients with chest pain and heart disease, spawning inequalities or disparities in care, have long been neglected, and remain only partially addressed open issues, requiring further research and action.Citation114,Citation115 Etiology, risk factors, pathogenesis, presentation, evaluation, diagnostic testing, physicians’ choice of treatment, response to therapy, and outcomes are all gender specific.Citation116 Even initiation or restarting drugs for secondary prevention lags in women. Gender differences in presentation of chest pain and angina are important and merit greater awareness among all members of cardiac service teams. Moreover, women have a 20 percent higher prevalence of stable angina than men.Citation117
The typical triad of angina includes effort induced substernal pressure or tightness and relief upon rest or use of nitroglycerin. Patients with atypical histories and symptoms, especially women,Citation116,Citation118,Citation119 are more likely to be misdiagnosed and under treated. Women with acute coronary syndromes (ACS) have more dyspnea, indigestion, nausea and vomiting, weakness, and back pain than men.Citation120,Citation121 In a recent study, a significantly greater number of men presenting with chest pain (17%) had a diagnosis of CAD than women (13%), and chest pain lasting from 1–12 hours in women was more likely to be due to CAD than in men, who reported a shorter episode (30–60 min).Citation122 Another series of 112 women and 144 men admitted for ACS confirmed greater reporting of indigestion, palpitations, nausea, numbness of the hands, and fatigue in women.Citation123 The vagueness and nonspecific nature of these symptoms poses difficulties in clinical decision making. Ischemic heart disease is a different disease in women and is strongly dependent upon stage of life; in young women, differences are even greater ().
Table 7 Some observations of interest about angina/ischemic heart disease in womenTable Footnote*
Evaluation, appropriateness of treatment, and research inequality in women, with respect to atherosclerosis progression, relief of symptoms and ultimate prognosis, are concerns that begin with risk factor differences between gendersCitation183 and persist even beyond percutaneous coronary intervention (PCI).Citation184 For instance, a gender delay in emergency medical services in Dallas County, Texas was dismissed as minor, but women were actually 52% more likely than men to be delayed 15 min or more from the time emergency medical services teams arrived in response to a call and reaching a hospital, potentially involving additional myocardial cell death, critical in subsequent complication rates and prognosis.Citation161,Citation162 Interestingly, during an evaluation of gender differences in the management and prognosis of myocardial infarction, women had a higher body mass index and more diabetes, renal dysfunction and depression, but less chronic lung disease, smoking history, cancer, and fewer prior myocardial infarctions than men.Citation185
Cardiac electrophysiological differences between men and women are well known.Citation186 Women have longer QT intervals, and estradiol and testosterone are capable of altering portions of the cardiac action potential. Estradiol has been linked to after-depolarizations and torsades de pointes in laboratory animals. Inappropriate sinus tachycardia, more common in women, may be related to both autonomic dysregulation of the sinus node and/or an immunological disorder of cardiac β-adrenergic receptors. Significant gender differences in sudden cardiac death have been reported, including different responses to therapy. Despite equal benefits derived from such devices, utilization of implantable cardioverter defibrillators and cardiac resynchronization therapy is lower in women.Citation187
Women enjoy premenopausal protection against IHD, which may be blunted by diabetes, multiple risk factors, and a myocardial infarction. Why women, with a higher prevalence of risk factors, clinically more difficult angina, fewer obstructive coronary lesions, and milder myocardial infarctions have poorer clinical outcomes, most accentuated in younger women, remains uncertain.Citation14,Citation188 Another feature of the paradox is the higher incidence of heart failure in the face of better left ventricular systolic function, as compared with men, before PCI. Fundamental biological differences between sexes, especially microvascular dysfunction, with smooth muscle, endothelial, and autonomic nervous system components, appear to contribute to ischemic physiology in women (). However, as attractive as the endothelial and microvascular dysfunction hypothesis is, supporting data are not yet robust. Failure to follow guidelines equally, ie, gender bias in invasive procedures, accounts for only a part of the difference.Citation189,Citation190
Perhaps the lack of a single cohesive explanation of differences between the pathophysiology of IHD in women and men contributes in a small way to gender disparities, since the message cannot be underpinned with a large, single arrow. Nonetheless, women generally do not receive sufficiently intense therapy when treated medically for CAD,Citation189,Citation191 nor after AMI,Citation192 with or without obstructive CAD. However, women with chronic stable angina and CAD most certainly benefit from, and deserve, full medical therapy just as do men,Citation193 and the guidelines are clear.
A meta-analysis of randomized trials compared the effects of a conservative vs an invasive strategy in women and men with acute coronary syndrome without ST-elevation.Citation194 While high risk patients of either sex enjoyed a 20% reduction in the composite endpoint of death, myocardial infarction, or recurrent ACS, an early invasive treatment in women with angina/ACS and negative biomarkers was associated with a 35% increase in risk of death. Men did not face this risk. These data significantly tempered enthusiasm for aggressive ACS strategies in low risk women, and ACC/AHA guidelines now recommend an invasive strategy in high risk women (the same as men), but in low risk women, a conservative strategy is advised.Citation195–Citation198
Goals in management of the patient with angina
There are generally three inter-related goals in managing patients with stable chronic angina:
Limit the number, severity, and sequellae of anginal attacks, including psychological consequences, thereby increasing quality of life.
Protect against future, potentially more lethal ischemic syndromes, such as sudden death, myocardial infarction, and cardiogenic shock.
Lower the risk for atherosclerosis progression.
Conclusion
The diagnosis of chronic stable angina is made clinically, and is further refined by laboratory data, including electrocardiography, exercise testing, imaging, and possibly coronary angiography. Coronary artery disease, or ischemic heart disease, is the leading cause of death in the United States. Angina is one of the syndromes produced by CAD, and chest discomfort is a commonly encountered symptom reflecting myocardial ischemia. Successful management draws upon both the science and art of medicine, but yet may challenge even the most seasoned cardiologist. New pathophysiological data, as well as conceptual and technological advances, have consistently improved patient evaluation over the past decade.
While perhaps less fashionable than topics concerning myocardial infarction/STEMI/NSTEMI, PCI, and CABG, the sheer number of patients afflicted with angina has attracted renewed interest. Independently, diagnosis, risk assessment, ability to predict prognosis, and treatment all remain imperfect.
Unfortunately, just as guideline defined targets remain unmet in the treatment of hypertension, dyslipidemia, and diabetes, significant numbers of women, and to a lesser degree, men, are also undertreated for their angina, and suffer ongoing, disabling exertional symptoms while under active medical care. Despite fundamental advances in basic science and availability of clinical outcome data, clinical inertia in following current guidelines continues to be a barrier in achieving therapeutic goals.
In the second part of this two-part series, current evidence based medical management with anti-ischemic therapy, promising novel anti-anginal agents and their potential to improve outcomes, options for treating refractory angina, the important role of implementing population-wide, lifestyle modification and risk reduction to lower the prevalence and burden of angina and ischemic heart disease, and current data, guidelines, and comparative performance regarding revascularization procedures in patients will be reviewed.
Acknowledgements
The author wishes to thank Michelle Delaney for her astuteness, computer skills, untiring assistance, and valuable suggestions in the preparation of this manuscript.
Disclosure
The author reports no conflicts of interest in this work.
References
- SkalskiJHMyocardial infarction and angina pectoris in the history of Polish medicinePol Arch Med Wewn2008118424324718575426
- IqbalJFoxKAAEpidemiological trends in acute coronary syndromes: understanding the past to predict and improve the futureArch Med Sci201061AS3S14
- GiuglianoDCerielloAEspositoKThe effects of diet on inflammationJ Am Coll Cardiol20064867768516904534
- IkedaUInflammation and coronary artery diseaseCurr Vasc Pharmacol200311657015320854
- HeinischRHZanettiCRCominFFernandesJLRamiresJASerranoCVJrSerial changes in plasma levels of cytokines in patients with coronary artery diseaseVasc Health Risk Manag20051324525017319110
- RidkerPMTesting the inflammatory hypothesis of atherothrombosis: scientific rationale for the cardiovascular inflammation reduction trial (CIRT)J Thromb Haemost20097Suppl 133233919630828
- DevarajSSinghUJialalIThe evolving role of C-reactive protein in atherothrombosisClin Chem20095522923819095731
- RidkerPMInflammation, high-sensitivity C-reactive protein, and vascular protectionTex Heart Inst J2010371404120200625
- DewellAOrnishDPlant-based dietary patterns in the control of obesity and cardiovascular riskCurr Cardiovasc Risk Rep20071915
- BrownWVKarmallyWKris-EthertonPRudelLRDiscussion on dietary fatJ Clin Lipidol20093303314
- Lloyd-JonesDMHongYLabartheDMozaffarianDon behalf of the American Heart Association Strategic Planning Task Force and Statistics CommitteeDefining and Setting National Goals for Cardiovascular Health Promotion and Disease Reduction. The American Heart Association’s Strategic Impact Goal Through 2020 and BeyondCirculation201012158661320089546
- PatelNBBaladyGJThe Rewards of Good BehaviorCirculation2010121673373520124131
- BuckleyBMurphyAWDo patients with angina alone have a more benign prognosis than patients with a history of acute myocardial infarction, revascularisation or both? Findings from a community cohort studyHeart20099546146718669551
- HemingwayHShipleyMBrittonAPrognosis of angina with and without a diagnosis: 11 year follow up in the Whitehall II prospective cohort studyBMJ200332789589814563744
- HemingwayHMcCallumAShipleyMIncidence and prognostic implications of stable angina pectoris among women and menJAMA20062951404141116551712
- GandhiMMLampeFCWooDAIncidence, clinical characteristics, and short-term prognosis of angina pectorisBr Heart J1995731931987696034
- Berecki-GisofJHumphreyes-ReidLWilsonADobsonAAngina symptoms are associated with mortality in older women with ischemic heart diseaseCirculation20091202330233619933930
- MeijsFMLBotsMLCramerMJMon behalf of the SMART Study groupUnrecognized myocardial infarction in subjects at high vascular risk: prevalence and determinantsHeart20099572873219218261
- AllamAhThompsonRCWannLSMiyamotoMIComputed Tomographic Assessment of Atherosclerosis in Ancient Egyptian MummiesJAMA20093022091209419920233
- MorrowDAAntmanEMEvaluation of high-sensitivity assays for cardiac troponinClin Chem2009555819028812
- BertrandMESimoonsMLFoxKATask Force on the Management of Acute Coronary Syndromes of the European Society of Cardiology. Management of acute coronary syndromes in patients presenting without persistent ST-segment elevationEur Heart J2002231809184012503543
- CannonRMicrovascular angina and the continuing dilemma of chest pain with normal coronary arteriesJ Am Coll Cardiol20095487788519712795
- AsburyEACollinsPCardiac Syndrome XInt J Clin Pract2005591063106916115183
- MayerSHillisLDPrinzmetal’s vriant anginaClin Cardiol1998212432469562933
- VandergotenPBenitEDendalePPrinzmetal’s variant angina: three case reports and a review of the literatureActa Cardiol199954717610378017
- SuedaSKohnoHFukudaHLimitations of medical therapy in patients with pure coronary spastic anginaChest200312338038612576355
- OngPAthanasiadisAHillSCoronary artery spasm as a frequent cause of acute coronary syndrome: the CASPAR (Coronary Artery Spasm in Patients with Acute Coronary Syndrome) studyJ Am Coll Cardiol20085252352718687244
- EagleKAGoodmanSGAvezumABudajASullivanCMLopez-SendonJGRACE InvestigatorsPractice variation and missed opportunities for reperfusion in ST-segment elevation myocardial infarction: findings from the Global Registry of Acute Coronary Events (GRACE)Lancet200235937337711844506
- HwangSYParkEHShinESJeongMHComparison of factors associated with atypical symptoms in younger and older patients with acute coronary syndromesJ Korean Med Sci20092478979419794972
- KachintornUHow do we define non-cardiac chest pain?J Gastroenterol Hepatol200520SupplS2S516359344
- EslickGDCoulshedDSTalleyNJDiagnosis and treatment of noncardiac chest painNat Clin Pract Gastroenterol Hepatol2005246347216224478
- ShepsDSCreedFClouseREChest pain in patients with cardiac and noncardiac diseasePsychosom Med20046686186715564350
- CayleyWEJrDiagnosing the cause of chest painAm Fam Physician2005722012202116342831
- FassRDickmanRNon-cardiac chest pain: An updateNeurogastroenterol Motil20061840841716700719
- RingstromEFreedmanJApproach to undifferentiated chest pain in the emergency department: A review of recent medical literature and published practice guidelinesMt Sinai Med200673499505
- HewsonEGSinclairJWDaltonCBTwenty-four hour esophageal pH monitoring: The most useful test for evaluating noncardiac chest painAm J Med1994905765832029015
- ZahnerMRLiDPChenSRPanHLCardiac vanilloid receptor 1-expressing afferent nerves and their role in the cardiogenic sympathetic reflex in ratsJ Physiol (Lond)200355151552312829722
- PanHLChenSRSensing tissue ischemia: another new function for capsaicin receptors?Circulation20041101826183115364816
- UstinovaEEBergrenDSchultzHDNeuropeptide depletion impairs postischemic recovery of the isolated rat heart: role of substance PCardiovasc Res19953055637553724
- BolliRCardioprotective function of inducible nitric oxide synthase and role of nitric oxide in myocardial ischemia and preconditioning: an overview of a decade of researchJ Mol Cell Cardiol2001331897191811708836
- BolliRAbdel-LatifANo pain, no gain: The useful function of AnginaCirculation20051123541354316330693
- WangLWangDHTRPV1 gene knockout impairs postischemic recovery in isolated perfused heart in miceCirculation20051123617362316314376
- ForemanRDQinCQNeuromodulation of cardiac pain and cerebral vasculature: Neural mechanismsCleveland Clin J Med200976S75S79
- CamiciPGPaganiMCardiac NociceptionCirculation20061142309231217130354
- YanoKMacLeanCJThe incidence and prognosis of unrecognized myocardial infarction in the honolulu, hawaii, heart programArch Intern Med19891497152815322742427
- de TorbalABoersmaEKorsJAIncidence of recognized and unrecognized myocardial infarction in men and women aged 55 and older: The Rotterdam StudyEur Heart J20062772973616478749
- AronowWSSilentMIPrevalence and prognosis in older patients diagnosed by routine electrocardiogramsGeriatrics200358242636384012545670
- ZellwegerMJHachamovitchRKangXThreshold, incidence, and predictors of prognostically high-risk silent ischemia in asymptomatic patients without prior diagnosis of coronary artery diseaseJ Nuclear Cardiol2009162193200
- DeedwaniaPStonePHMerzCNBEffects of intensive versus moderate lipid-lowering therapy on myocardial ischemia in older patients with coronary heart disease: Results of the Study Assessing Goals in the Elderly (SAGE)Circulation200711570070717283260
- ParkerJOChiongMAWestROSequential alterations in myocardial lactate metabolism, ST segments, and left ventricular function during angina induced by atrial pacingCirculation1969401131315792993
- SciricaBMMorrowDABudajAIschemia detected on continuous electrocardiography after acute coronary syndrome: observations from the MERLIN-TIMI 36 (Metabolic Efficiency With Ranolazine for Less Ischemia in Non-ST-Elevation Acute Coronary Syndrome-Thrombolysis In Myocardial Infarction 36) TrialJ Am Coll Cardiol2009531411142119371824
- NorgaardBLAndersenKDellborgMThe TRIM Study GroupAdmission risk assessment by cardiac Troponin T in unstable coronary artery disease: Additional prognostic information from continuous ST segment monitoringJ Am Coll Cardiol1999331519152710334417
- DeedwaniaPCCarbajalEVSilent ischemia during daily life is an independent predictor of mortality in stable anginaCirculation1990817487562306826
- GottoJRAMStatin therapy and the elderly: SAGE Advice?Circulation200711568168317296867
- ErnePSchoenenbergerAWZuberMEffects of anti-ischaemic drug therapy in silent myocardial ischaemia type I: the Swiss Interventional Study on Silent Ischaemia type I (SWISSI I): a randomized, controlled pilot studyEur Heart J2007282110211717644512
- CohnPFA new look at benefits of drug therapy in silent myocardial ischaemiaEur Heart J2007282053205417660518
- KwongRYChanAKBrownKAImpact of unrecognized myocardial scar detected by cardiac magnetic resonance imaging on event-free survival in patients presenting with signs or symptoms of coronary artery diseaseCirculation20061132733274316754804
- DweckMCampbellIWMillerDFrancisCMClinical aspects of silent myocardial ischaemia: with particular reference to diabetes mellitusBrit J Diab Vasc Disease20099110116
- GibbonsRJAbramsJChatterjeeKACC/AHA 2002 guideline update for the management of patients with chronic stable angina – summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina)J Am Coll Cardiol20034115916812570960
- The Criteria Committee of the New York Heart AssociationNomenclature and Criteria for Diagnosis of Diseases of the Heart and Great Vessels9th edBostonLittle, Brown & Co1994253256
- CampeauLThe Canadian Cardiovascular Society grading of angina pectoris revisited 30 years laterCan J Cardiol20021837137911992130
- HackettTPCassemNHPsychological aspects of rehabilitation following myocardial infarctionWengerNKHellersteinHKRehabilitation of the Coronary PatientJohn Wiley and Sons1978243253
- ShubCClickRLGoonMDMyocardial ischemia clinical syndromes; B: Angina pectoris and coronary heart diseaseGiulianiERGershBJMayo Clinic Practice of Cardiology3rd edMosby199611601190
- KonesRMetabolism of the acutely ischemic and hypoxic heartCrit Care Med197313213304272729
- KonesRMolecular and ionic basic of altered myocardial contractilityRes Commun Chem Pathol Pharmacol197351844356588
- KonesRCardiogenic ShockArmonk NYFutura-Blackwell Publishing1974
- FeiglEOCoronary physiologyPhysiol Rev19836312056296890
- KonesRPathogenesis of cardiogenic Shock IIN Y State J Med197373166216704575582
- DunckerDJBacheRJRegulation of coronary blood flow during exercisePhysiol Rev2008881009108618626066
- WesterhofNBoerCLambertsRRSipkemaPCross-talk between cardiac muscle and coronary vasculaturePhysiol Rev2006861263130817015490
- CollinsPCoronary Flow ReserveBr Heart J1993692792818489855
- HoolePHeckPMWhitePAIschemic preconditioning stimulus does not reduce microvascular resistance or improve myocardial blood flow in patients undergoing elective percutaneous coronary interventionAngiology200960440341119106155
- KlockeFJBairdMGLorellBHACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging: executive summary – a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging)Circulation20031081404141812975245
- CamiciPGRimoldiOEThe clinical value of myocardial blood flow measurementJ Nucl Med2009501076108719525470
- LibbyPTherouxPPathophysiology of coronary artery diseaseCirculation20051113481348815983262
- PfefferMBraunwaldEVentricular remodeling after myocardial infarction: experimental observations and clinical implicationsCirculation199081116111722138525
- DolleryCMLibbyPAtherosclerosis and proteinase activationCardiovasc Res20066962563516376322
- CroceKLibbyPIntertwining of thrombosis and inflammation in atherosclerosisCurr Opin Hematol200714556117133101
- KramerMRittersmaSde WinterRJRelationship of thrombus healing to underlying plaque morphology in sudden coronary deathJ Am Coll Cardiol20105512213219818571
- LevinRIPlaque vulnerability pathologic form and patient fateJ Am Coll Cardiol20105513313420117380
- KuboTImanishiTKashiwagiMMultiple coronary lesion instability in patients with acute myocardial infarction as determined by optical coherence tomographyAm J Cardiol201010531832220102942
- KonesRThe Jupiter Study, CRP Screening, and aggressive statin therapy – implications for the primary prevention of cardiovascular diseaseTher Adv Cardiovasc Dis2009330931519460829
- FoxKGarciaMAArdissinoDTask Force on the Management of Stable Angina pectoris of the European Society of Cardiology; ESC Committee for Practice Guidelines (CPG). Guidelines on the management of stable angina pectoris: executive summary: the Task Force on the Management of Stable Angina Pectoris of the European Society of CardiologyEur Heart J2006271341138116735367
- AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, Part 8: Stabilization of the Patient With Acute Coronary SyndromesCirculation2005112Suppl 4I239I290
- GoldsteinJAGallagherMJO’NeillWWRossMAO’NeilBJRaffGLA Randomized Controlled Trial of Multi-Slice Coronary Computed Tomography for Evaluation of Acute Chest PainJ Am Coll Cardiol20074986387117320744
- HoffmannUBambergFChaeCUCoronary Computed Tomography Angiography for Early Triage of Patients With Acute Chest Pain: The ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) TrialJ Am Coll. Cardiol. 20095316421650
- JaffeASAppleFSHigh-Sensitivity Cardiac Troponin: Hype, Help, and RealityClin Chem20105634234420040616
- GiannitsisEBeckerMKurzKHessGZdunekDKatusHAHigh-Sensitivity Cardiac Troponin T for Early Prediction of Evolving Non-ST-Segment Elevation Myocardial Infarction in Patients with Suspected Acute Coronary Syndrome and Negative Troponin Results on AdmissionClin Chem20105664265020167697
- KellerTZellerTPeetzDTzikasSSensitive troponin I assay in early diagnosis of acute myocardial infarctionN Engl J Med200936186887719710485
- ReichlinTHochholzerWBassettiSEarly diagnosis of myocardial infarction with sensitive cardiac troponin assaysN Engl J Med200936185886719710484
- MorrowDAClinical application of sensitive troponin assaysN Engl J Med200936191391519710490
- deFilippiCRTocchiMParmarRJCardiac troponin T in chest pain unit patients without ischemic electrocardiographic changes: angiographic correlates and long-term clinical outcomesJ Am Coll Cardiol2000351827183410841231
- SánchezMPredictors and outcomes of frequent chest pain unit usersAm J Emerg Med20092766066719751622
- OluboyedeYGoodacreSWailooAfor the ESCAPE Research TeamCost effectiveness of chest pain unit care in the NHSBMC Health Services Research2008817418700961
- HillJTimmisAABC of electrocardiography: Exercise tolerance testingBMJ20023241084108711991917
- GibbonsRJBaladyGJBeasleyJWACC/AHA Guidelines for Exercise Testing A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing)J Am Coll Cardiol1997302603119207652
- MoriseAPDiamondGAComparison of the sensitivity and specificity of exercise electrocardiography in biased and unbiased populations of men and womenAm Heart J19951307417477572581
- MieresJHShawLJHendelRCAmerican Society of Nuclear Cardiology consensus statement: task force on women and coronary artery disease – the role of myocardial perfusion imaging in the clinical evaluation of coronary artery disease in women [correction]J Nucl Cardiol2003109510112569338
- ShawLJHachamovitchRIskandrianAETreadmill test scores: Attributes and LimitationsJ Nucl Cardiol1997474759138842
- ChaitmanBRThe changing role of the exercise electrocardiogram as a diagnostic and prognostic test for chronic ischemic heart diseaseJ Am Coll Cardiol19868119512103531288
- MarkDBShawLHarrellFEJrPrognostic value of a treadmill exercise score in outpatients with suspected coronary artery diseaseN Eng J Med1991325849853
- GibbonsRJBaladyGJBrickerJTCommittee Members Task Force MembersACC/AHA 2002 Guideline Update for Exercise Testing: Summary Article: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines)Circulation20021061883189212356646
- MieresJHShawLJAraiARole of Noninvasive Testing in the Clinical Evaluation of Women With Suspected Coronary Artery Disease: Consensus Statement From the Cardiac Imaging Committee, Council on Clinical Cardiology, and the Cardiovascular Imaging and Intervention Committee, Council on Cardiovascular Radiology and Intervention, American Heart AssociationCirculation200511168269615687114
- JacobsAKCoronary Intervention in 2009: Are Women No Different Than Men?Circ Cardiovasc Interv20092697820031695
- UdelsonJEBeshanskyJRBallinDSMyocardial perfusion imaging for evaluation and triage of patients with suspected acute cardiac ischemia: A randomized controlled trialJAMA20022882693270012460092
- DouglasPSTaylorABildDOutcomes Research in Cardiovascular Imaging: Report of a Workshop Sponsored by the National Heart, Lung, and Blood InstituteJ Am Coll Cardiol Img20092897907
- PouleurACLe Polain de WarouxJBKeferJPasquetAVanoverscheldeJLGerberBLDirect comparison of whole-heart, navigatorgated magnetic resonance coronary angiography and 40/64-slice multi-detector row computed tomography to detect coronary artery stenosis in patients scheduled for conventional coronary angiographyCirc Cardiovasc Imaging2008111412119808528
- LeeJNiedererSNordslettenDCoupling contraction, excitation, ventricular and coronary blood flow across scale and physics in the heartPhil Trans R Soc A20093672311233119414457
- PennellDJCardiovascular Magnetic ResonanceCirculation201012169270520142462
- KimHWFarzaneh-FarAKimRJCardiovascular Magnetic Resonance in Patients With Myocardial Infarction: Current and Emerging ApplicationsJ Am Coll Cardiol20105511620117357
- de FeyterPJvan GeunsRJNoninvasive Coronary Imaging: The Contest between Magnetic Resonance and Computed Tomographic Coronary AngiographyCirc Cardiovasc Imaging20081899119808524
- HendelRCBermanDSDi CarliMFACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear MedicineJ Am Coll Cardiol2009532201222919497454
- EmondMMockMBDavisKBLong-term survival of medical treated patients in the Coronary Artery Surgery Study (CASS) RegistryCirculation19949026457994804
- MensahGAMokdadAHFordESGreenlundKJCroftJBState of disparities in cardiovascular health in the United StatesCirculation20051111233124115769763
- MoscaLGrundySMJudelsonDAmerican Heart Association/American College of Cardiology AHA/ACC scientific statement consensus panel statement. Guide to preventive cardiology for womenCirculation1999992480248410318674
- ShawLJMerzCNPepineCJfor the WISE investigatorsInsights from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation (WISE) studyJ Am Coll Cardiol200647SupplS4S2016458170
- HemingwayHLangenbergCDamantJPrevalence of angina in women versus men: a systematic review and meta-analysis of international variations across 31 countriesCirculation20081171526153618347213
- ChouAFWongLWeismanCSGender disparities in cardiovascular disease care among commercial and medicare managed care plansWomens Health Issues20071713914917481918
- LanskyAJHochmanJSWardPAAmerican College of Cardiology FoundationAmerican Heart AssociationPercutaneous coronary intervention and adjunctive pharmacotherapy in women: a statement for healthcare professionals from the American Heart AssociationCirculation200511194095315687113
- MilnerKAVaccarinoVArnoldALFunkMGoldbergRJGender and age differences in chief complaints of acute myocardial infarction (Worcester Heart Attack Study)Am J Cardiol20049360660814996588
- Arslanian-EngorenCPatelAFangJSymptoms of men and women presenting with acute coronary syndromesAm J Cardiol2006981177118117056322
- BosnerSHassenritterJHaniMAGender differences in presentation and diagnosis of chest pain in primary careBMC Family Practice2009107920003406
- DeVonHARyanCJOchsALShapiroMSymptoms across the continuum of acute coronary syndromes: differences between women and menAm J Crit Care200817142518158385
- BessantRHingoraniAPatelLMacGregorAIsenbergDARahmanARisk of coronary heart disease and stroke in a large British cohort of patients with systemic lupus erythematosusRheumatology (Oxford)20044392492915150430
- Von MeringGOArantCBWesselTRNational Heart, Lung and Blood InstituteAbnormal coronary vasomotion as a prognostic indicator of cardiovascular events in women: results from the National Heart, Lung, and Blood Institute-Sponsored Women’s Ischemia Syndrome Evaluation (WISE)Circulation200410972272514970106
- ReisSEHolubkovRConrad SmithAJCoronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: results from the NHLBI WISE studyAm Heart J200114173574111320360
- SunHMohrMShimokawaHCoronary microvascular spasm causes myocardial ischemia in patients with vasospastic anginaJ Am Coll Cardiol20023984785111869851
- HibinoHKurachiYA new insight into the pathogenesis of coronary vasospasmCirc Res20069857958116543506
- KakkarRYeBStollerDASpontaneous coronary vasospasm in KATP mutant mice arises from a smooth muscle-extrinsic processCirc Res20069868268916456098
- HanSHBaeJHHolmesDRSex differences in atheroma burden and endothelial function in patients with early coronary atherosclerosisEur Heart J2008291359136918424787
- ColacurciNManzellaDFornaroFCarbonellaMPaolissoGEndothelial function and menopause: effects of raloxifene administrationJ Clin Endocrinol Metab2003882135214012727966
- RossiRNuzzoAOriglianiGModenaMGPrognostic role of flow-mediated dilation and cardiac risk factors in post-menopausal womenJ Am Coll Cardiol200851997100218325438
- BeckerDMSegalJVaidyaDSex differences in platelet reactivity and response to low-dose aspirin therapyJAMA20062951420142716551714
- RidkerPMCookNRLeeIMA randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in womenN Engl J Med20053521293130415753114
- RosamondWFlegalKFurieKfor the Writing Group MembersHeart disease and stroke statistics – 2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics SubcommitteeCirculation2008117e25e14618086926
- FordESCapewellSCoronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality ratesJ Am Coll Cardiol2007502128213218036449
- Centers for Disease Control and Prevention Racial/Ethnic Disparities in Prevalence, Treatment, and Control of Hypertension – United States, 1999–2002. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5401a3.htm Accessed Aug 25, 2008.
- NiHCoadySRosamondWTrends from 1987 to 2004 in sudden death due to coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) studyAm Heart J2009157465219081395
- WongTYKleinRSharrettARRetinal arteriolar narrowing and risk of coronary heart disease in men and womenJAMA20022871153115911879113
- ShawLJShawREBairey MerzCNImpact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in-hospital mortality in the American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR)Circulation20081171787180118378615
- Bairey MerzCNShawLJReisSEIschemic heart disease in women: insights from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study. Part II: Gender differences in presentation, diagnosis, and outcome with regard to sex-based pathophysiology of atherosclerosis, macro- and micro-vascular CADJ Am Coll Cardiol200647Suppl21s29s
- BurkeAPFarbAMalcolmGTLiangYSmialekJVirmaniREffects of risk factors on the mechanism of acute thrombosis and sudden coronary death in womenCirculation199897211021169626170
- BurkeAPVirmaniRGalisZHaudenschildCCMullerJE34th Bethesda Conference: Task force #2 – what is the pathologic basis for new atherosclerosis imaging techniques?J Am Coll Cardiol2003411874188612798554
- AkahoshiMSodaMNakashimaEEffects of menopause on trends of serum cholesterol, blood pressure, and body mass indexCirculation19969461668964119
- DerbyCACrawfordSLPasternakRCSowersMSternfeldBMatthewsKALipid changes during the menopause transition in relation to age and weight: The Study of Women’s Health Across the NationAm J Epidemiol2009169111352136119357323
- McTigueKLarsonJCValoskiAMortality and cardiac and vascular outcomes in extremely obese womenJAMA2006296798616820550
- JanssenIPowellLHCrawfordSLasleyBSutton-TyrrellKMenopause and the metabolic syndrome: The Study of Women’s Health Across the NationArch Intern Med2008168141568157518663170
- RamosRGOldenKThe prevalence of metabolic syndrome among US women of childbearing ageAm J Public Health2008981122112718445796
- HokansonJEAustinMAPlasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein level: a meta-analysis of population-based prospective studiesJ Cardiovasc Risk199632132198836866
- Barrett-ConnorELCohnBAWingardDLEdelsteinSLWhy is diabetes mellitus a stronger risk factor for fatal ischemic heart disease in women than in men? The Rancho Bernardo StudyJAMA19912656276311987413
- GreggEWGuQChengYJNarayanKMCowieCCMortality trends in men and women with diabetesAnn Intern Med200714714915517576993
- WongNDPioJValenciaRThakalGDistribution of C-reactive protein and its relation to risk factors and coronary heart disease risk estimation in the National Health and Nutrition Examination Survey (NHANES) IIIPrev Cardiol2001410911411828186
- RidkerPMBuringJECookNRRifaiNC-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8- year follow-up of 14,719 initially healthy American womenCirculation200310739139712551861
- CookNRBuringJERidkerPMThe effect of including C-reactive protein in cardiovascular risk prediction models for womenAnn Intern Med2006145212916818925
- PasternakRCAbramsJGreenlandP34th Bethesda Conference: task force #1 – identification of coronary heart disease risk: is there a detection gap?J Am Coll Cardiol2003411863187412798553
- LakoskiSGGreenlandPWongNDSchreinerPJCoronary artery calcium scores and risk for cardiovascular events in women classified as “low risk” based on Framingham risk score: the Multi-Ethnic Study of Atherosclerosis (MESA)Arch Intern Med20071672437244218071165
- RidkerPMBuringJERifaiNCookNRDevelopment and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk ScoreJAMA200729761161917299196
- O’Keefe-McCarthySWomen’s experiences of cardiac pain: a review of the literatureCan J Cardiovasc Nurs2008181825
- DouglasPSGinsburgGSThe evaluation of chest pain in womenN Engl J Med1996334131113158609950
- TingHHBradleyEHWangYFactors associated with longer time from symptom onset to hospital presentation for patients with ST-elevation myocardial infarctionArch Intern Med200816895996818474760
- ConcannonTWGriffithJLKentDMElapsed Time in emergency medical services for patients with cardiac complaints: are some patients at greater risk for delay?Circ Cardiovasc Qual Outcomes2009291520031807
- OrnatoJPGender Delay in Emergency Medical Services: Does it Really Exist?Circ Cardiovasc Qual Outcomes200924520031805
- JohnsonBDKelseySFBairey MerzCNClinical risk assessment in women: chest discomfort Report from the WISE studyShawLJRedbergRFCAD in Women: Evidence-Based Diagnosis and TreatmentTotowa, NJHumana Press2003129142
- JohnsonBDBairey MerzCNKelseySFPersistent chest pain predicts cardiovascular events in women with and without obstructive coronary artery disease: results from the NHLBI-sponsored WISE studyEur Heart J2006271408141516720691
- ShawLJBairey MerzCNPepineCJfor the Women’s Ischemia Syndrome Evaluation (WISE) InvestigatorsThe Economic Burden of Angina in Women With Suspected Ischemic Heart Disease: Results From the National Institute of Health – National Heart, Lung, and Blood Institute – Sponsored Women’s Ischemia Syndrome Evaluation (WISE)Circulation200611489490416923752
- ShawLJHellerGVTravinMICost analysis of diagnostic testing for coronary artery disease in women with stable chest painJ Nucl Cardiol1999655956910608582
- OlsonMBKelseySFMatthewsKSymptoms, myocardial ischaemia and quality of life in women: results from the NHLBI-sponsored WISE StudyEur Heart J2003241506151412919775
- KwokYSKimCGradyDMeta-analysis of exercise testing to detect coronary artery disease in womenAm J Cardiol19998366066610080415
- GulatiMArnsdorfMFShawLJPrognostic value of the duke treadmill score in asymptomatic womenAm J Cardiol20059636937516054460
- GulatiMPandeyDKArnsdorfMFExercise capacity and the risk of death in womenCirculation20031081554155912975254
- KavanaghTMertensDJHammLFPeak oxygen intake and cardiac mortality in women referred for cardiac rehabilitationJ Am Coll Cardiol2003422139214314680741
- ShawLJIskandrianAEPrognostic value of stress gated SPECT in patients with known or suspected coronary artery diseaseJ Nucl Cardiol20041117118515052249
- ShawLJVaseyCSawadaSRimmermanCMarwickTHImpact of gender on risk stratification by exercise and dobutamine stress echocardiography: long-term mortality in 4,234 women and 6,898 menEur Heart J20052644745615687253
- SicariRPasanisiEVenneriLLandiPCortigianiLPicanoEEcho Persantine International Cooperative (EPIC) Study Group. Echo Dobutamine International Cooperative (EDIC) Study Group. Stress echo results predict mortality: a large-scale multicenter prospective international studyJ Am Coll Cardiol20034158959512598070
- SharafBLPepineCJKerenskyRADetailed angiographic analysis of women with suspected ischemic chest pain (pilot phase data from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation [WISE] Study Angiographic Core Laboratory)Am J Cardiol20018793794111305981
- BugiardiniRBairey MerzCNAngina with “normal” coronary arteries: a changing philosophyJAMA200529347748415671433
- AndersonRDPepineCJGender differences in the treatment for acute myocardial infarction: bias or biology?Circulation200711582382617309930
- CookNLAyanianJZOravEJHicksLSDifferences in specialist consultations for cardiovascular disease by race, ethnicity, gender, insurance status, and site of primary careCirculation20091192463247019398667
- LanskyAJOutcomes of percutaneous and surgical revascularization in womenProg Cardiovasc Dis20044630531914961454
- ModenaMGBonettiLCoppiFPrognostic role of reversible endothelial dysfunction in hypertensive postmenopausal womenJ Am Coll Cardiol20024050551012142118
- KyBKirwanBAde BrouwerSGender differences in cardiac remodeling and clinical outcomes in chronic stable angina pectoris (from the ACTION Trial)Am J Cardiol201010594394720346310
- ChangWCKaulPWesterhoutCMImpact of sex on long-term mortality from acute myocardial infarction vs unstable anginaArch Intern Med20031632476248414609784
- Schenck-GustafsonKHow do gender differences affect cardiovascular risk factors?Dialogues in Cardiovasc Med200813103110
- HomvangLMickleyHGender differences following percutaneous coronary interventionTher Adv Cardiovasc Dis2008210911319124414
- SetoguchiSSolomonDHLevinRWinkelmayerWCGender differences in the management and prognosis of myocardial infarction among patients ≥65 years of ageAm J Cardiol20081011531153618489928
- YarnozMJCurtisABMore reasons why men and women are not the same (gender differences in electrophysiology and arrhythmias)Am J Cardiol20081011291129618435960
- YarnozMJCurtisABSex-based differences in cardiac resynchronization therapy and implantable cardioverter-defibrillator therapies: effectiveness and useCardiol Rev20061429229817053376
- HumphriesKHPuAGaoMCarereRGPiloteMAngina with “normal” coronary arteries: sex differences in outcomesAm Heart J200815537538118215611
- BlomkalnsALChenAYHochmanJSGender disparities in diagnosis & treatment of non-ST-segment elevation acute coronary syndromesJ Am Coll Cardiol20054583283715766815
- HvelplundAGalatiusSMadsenMWomen with acute coronary syndrome are less invasively examined and subsequently less treated than menEur Heart J20103168469019933516
- MoscaLMochari-GreenbergerHDolorRJKristin NewbyLKarenJRobb. Twelve-year follow-up of American women’s awareness of cardiovascular disease risk and barriers to heart healthCirc Cardiovasc Qual Outcomes2010312012720147489
- GanSCBeaverSKHouckPMMacLehoseRFLawsonHWChanLTreatment of acute myocardial infarction and 30-day mortality among women and menN Engl J Med200034381510882763
- BodenWEO’RourkeRATeoKKOptimal medical therapy with or without PCI for stable coronary diseaseN Engl J Med20073561503151617387127
- O’DonoghueMBodenWEBraunwaldEEarly invasive vs conservative treatment strategies in women and men with unstable angina and non-ST-segment elevation myocardial infarctionJAMA2008300718018594042
- AndersonJLAdamsCDAntmanEMACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction)J Am Coll Cardiol200750e1e15717692738
- StegPHimbergDUnmet medical needs and therapeutic opportunities in stable anginaEur Heart J20057H7H15
- MannheimerCCamiciPChesterMRThe problem of chronic refractory angina; report from the ESC Joint Study Group on the Treatment of Refractory AnginaEur Heart J20022335537011846493
- FrakerTDJrFihnSDWriting on behalf of the 2002 Chronic Stable Angina Writing Committee 2007 Chronic Angina Focused Update of the ACC/AHA 2002 Guidelines for the Management of Patients With Chronic Stable AnginaA Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to Develop the Focused Update of the 2002 Guidelines for the Management of Patients With Chronic Stable AnginaJ Am Coll Cardiol2007502264227418061078
- PatelMRPetersonEDDaiDLow diagnostic yield of elective coronary angiographyN Engl J Med201036288689520220183