Abstract
Background: A successful antimicrobial stewardship program (ASP) is sustained through improving antimicrobial prescribing by changing prescribing behavior. This requires a better understanding of hospital stakeholders’ views regarding antimicrobial resistance (AMR), antimicrobial use and participation in ASP activities. Objectives: Identify perceptions and attitudes among physicians and pharmacists in a public hospital toward AMR, prescription and ASP. Methods: A questionnaire consisting of 45 items was distributed to physicians and pharmacists in a 320-bed public hospital. All responses were formatted into the Likert scale. Results: A total of 78 respondents (73% response rate) completed the questionnaire. The majority of the respondents perceived AMR within hospital as less of a severe problem, and factors outside hospital were considered to be greater contributors to AMR. In addition, interprofessional conflict was identified as a serious concern in relation to implementing ASP. Conclusion: This finding indicates the need to address existing perceptions and attitudes toward ASP activities that may hamper its successful implementation in Indonesia.
Antimicrobial resistance (AMR) is a global threat in the medical field [Citation1,Citation2]. In addition to the devastating impact of infections that are resistant to commonly used antimicrobials, the slow development of new antimicrobials to treat resistant pathogens is concerning [Citation2,Citation3]. While encouraging progress to create novel antimicrobial entities has been observed [Citation3–6], efforts to maintain the efficacy of existing antimicrobial resources are of paramount importance [Citation4]. Furthermore, given the limited options of antimicrobials in the low- and middle-income countries, strong commitment to using currently available antimicrobials judiciously is essential in the healthcare setting [Citation7,Citation8]. Though the predominant use of antimicrobials is in primary healthcare settings [Citation9], inappropriate use of antimicrobials remains a challenging issue in hospitals [Citation10,Citation11].
Along with infection control measures, the use of antimicrobial stewardship programs (ASPs) is considered a fundamental strategy to minimize the emergence and escalation of AMR in hospitals [Citation12]. Antimicrobial stewardship program activities have successfully decreased antimicrobial consumption and helped contain the development of antimicrobial-resistant pathogens in hospitals without compromising clinical benefit [Citation13,Citation14]. Regardless of the strategies being implemented, one critical component of any successful ASP initiative is changing the behavior in antimicrobial prescribing practices [Citation15,Citation16]. Identifying factors that influence antimicrobial prescribing patterns has been shown to help change prescribing behavior and curtail the inappropriate use of antimicrobials in hospitals [Citation17].
Through the Indonesian Ministry of Health in 2015, hospital ASPs have found political momentum to be widely implemented across the country [Citation18]. There are more than 2400 hospitals in Indonesia, and almost 40% are public hospitals. Even though the total number is less than the private hospitals, the beds in public hospitals contribute almost 55% of the total bed capacity in Indonesia [Citation19]. The pressure to enact hospital-wide ASP activities has only increased since then, as the Indonesian Commission for Hospital Accreditation regards these ASPs as a central indicator in the hospital accreditation process [Citation20]. Nevertheless, reports regarding the extent to which hospital-wide ASP implementation has occurred across the country are yet to be published.
It is now acknowledged that regular survey of knowledge, beliefs, attitudes and perceptions on antimicrobial use is central to evaluating the successful implementation of hospital-wide ASPs [Citation17]. Currently, published surveys in an Indonesian setting explored two main areas: the knowledge and belief of healthcare professionals toward judicious antimicrobial use [Citation21]; and whether the requirements for successful ASP implementation, as recommended by the CDC, are in place [Citation22]. The perceptions and attitudes of key healthcare stakeholders toward ASP implementation in Indonesian hospitals, however, are currently unknown. In particular, concerns regarding ASP implementation, particularly the impact on hospital hierarchy and prescribing autonomy, are yet to be investigated [Citation21–23]. Lack of understanding of these aspects may hamper the sustainability of ASP implementation in Indonesian hospitals [Citation24,Citation25].
The aim of this study was to describe perceptions and attitudes toward AMR, antimicrobial use and ASPs among key healthcare professionals in an urban teaching hospital in Indonesia.
Materials & methods
Study design & setting
A descriptive cross-sectional study was conducted in a 320-bed public hospital in Surabaya, East Java Province, Indonesia. At the time of survey, there were 65 specialist physicians, 30 general physicians, 12 pharmacists and 357 nurses covering 24 outpatient departments, emergency department, a dialysis centre, inpatient wards and an intensive care unit. There were no infectious disease physicians, specialist infectious disease pharmacists or clinical microbiologists at the hospital. However, some of the physicians at the hospital have a special interest in infectious disease, while some pharmacists have a master’s degree in clinical pharmacy. An ASP team consisting of 15 people from different disciplinary backgrounds, including physicians with various specialties, pharmacists, nurses and midwives, was established at the hospital in 2016. Limited ASP activities were being conducted by this team at the time of study. These mainly focused on monitoring and reporting the most frequent antimicrobials used in the hospital.
Questionnaire development
A purposive structured questionnaire, designed to be self-administered, was used in this study. The first section of the questionnaire collected demographic information and included a brief description of ASPs in anticipation of some respondents not being familiar with the term. The second section covered four domains: attitudes toward introduction of a hospital-wide ASP, perceptions toward AMR, antimicrobial use and the impact of ASP implementation. Items for each domain were generated through a literature review [Citation17,Citation26–42], together with input from an expert from Australia. The first draft of the questionnaire was written in English and consisted of 75 items. This first draft was sent to a multidisciplinary research group consisting of physicians, hospital pharmacists and academic faculty members from both Australia and Indonesia for content validation. Except for two questions regarding the contribution of antimicrobial use in agriculture and veterinary medicine to the problem of AMR in hospitals (which were subsequently deleted), all other questions were considered appropriate for identification of perceptions and beliefs toward AMR, antimicrobial utilization and ASP implementation in the hospitals. In addition, another five questions were deleted because they were deemed to have very similar content with other questions. Upon further review, it was highlighted by our Indonesian research group that a total of 68 questions might be considered too long, resulting in hospital-based workers not being willing to complete it due to time constraints. Therefore questions surrounding perceptions of factors influencing antimicrobial prescribing behavior (n = 15) and continuing education (n = 8) were further deleted. The final approved survey contained 45 items.
Items were formatted with a seven-point Likert scale which included several possible answers ranging from ‘strongly disagree’ to ‘strongly agree’, from ‘not useful at all’ to ‘very useful’, from ‘not a problem’ to ‘a very serious problem’ and from ‘never’ to ‘always’. Translation into Bahasa Indonesia was conducted by one researcher (ES), and the backward translation to English version was conducted by a native English-speaking researcher fluent in Bahasa Indonesia.
Face validity and reliability of the Indonesian version of the 45-item questionnaire were established through field tests conducted among 21 physicians and 21 hospital pharmacists from several hospitals other than the study hospital. Previous survey studies and methodology have defined a Chronbach’s α-coefficient of 0.45–0.99 as acceptable for internal consistency [Citation43,Citation44]. In our study, we defined a Chronbach’s α ≥0.6 as acceptable [Citation44]. Based on a sample of 42 respondents, our survey was expected to achieve this defined threshold for an acceptable Chronbach’s α-coefficient [Citation43]. In our pre-testing, it was found that the time needed to complete the questionnaire ranged from 8 to 16 min, while the Chronbach’s α-coefficients for the four domains ranged from 0.72 to 0.906.
Eligibility criteria of respondents & data collection
All physicians and pharmacists working in the hospital were eligible to be included in this study. However, those who were not active at the time of questionnaire distribution, including those on study and annual leave, were excluded. Physicians in training were also excluded from participation.
A set of documents consisting of an introductory letter, a respondent information sheet, two copies of an informed consent form and a copy of ethical clearance was handed to each respondent along with the questionnaire. Besides written documentation, the nature of voluntary participation and anonymity was verbally explained to each respondent at the time of distributing the questionnaire.
The questionnaire was distributed to all physicians and pharmacists on site during working hours from the end of April 2019 to the end of August 2019. Participation was voluntary. One of the researchers (ES) visited respondents to follow up completion of the questionnaire. Those who did not hand in the questionnaire after being visited on three separate occasions or who clearly stated that they did not want to participate were excluded in the final analysis. There was no incentive given to participate in the questionnaire.
Data analysis
Descriptive analyses using means and percentages were performed for the sociodemographic data. Categorical data were presented as proportions that were ‘in agreement’ or as a ‘serious problem’ (i.e., those with a ‘6’ and ‘7’ Likert scale response). Levels of concern toward the consequences of ASP were graded as ‘no concern’ (i.e., a ‘1’ or ‘2’ Likert scale response), ‘limited concern’ (i.e., a ‘3’, ‘4’ or ‘5’ Likert scale response) and ‘very concerned’ (i.e., with a ‘6’ or ‘7’ Likert scale response). A two-sided Fisher’s exact test or Pearson’s χ-square test were used to compare the perceptions toward AMR and antimicrobial use in the hospital, and attitudes toward ASP between physicians and pharmacists [Citation45]. A p-value of <0.05 was used as a cutoff point to define statistically significant differences observed between the two professions. All data analysis was conducted in Statistics/Data Analysis (STATA) Special Edition v.16.p (StataCorp, TX, USA).
Ethical consideration
This study was approved by the Human Research Ethics Committee (HREC) of the University of Queensland (approval no. 2018001341) and the Ethical Committee at the research site (approval no. 004/KE/KEPK/2019).
Results
A total of 107 questionnaires were distributed and 78 were returned, corresponding to a response rate of 73%. Returned questionnaires were from 12 pharmacists (out of 12) and 66 physicians (out of 95), giving response rates of 100 and 69.4%, respectively. Three physicians were on leave at the time of data collection, and 26 did not return the questionnaire regardless of follow-up efforts. One pediatrician did not complete due to time constraints; reasons for not completing the questionnaire for the remaining non-responder physicians could not be determined. presents the detailed demographic information of respondents.
Table 1. Characteristics of participants.
Antimicrobial resistance
More than 50% of respondents agreed that AMR was a serious problem in their hospital (). When asked about the impact of AMR on their patients, a large proportion of respondents agreed that AMR could prolong hospital stay, increase health expenditure and lead to worse clinical outcomes. When compared with the physicians, pharmacists were significantly less likely to have experience caring for a patient with a multidrug-resistant infection (p = 0.007). Almost 90% of respondents agreed that factors outside of the hospital, including self-medication with antimicrobials and poor patient adherence, contributed to AMR. In comparison, fewer participants felt that intrahospital factors such as overuse of antimicrobials in the hospital (70.5%) and ineffective infection control (71.8%) in the hospital would contribute to AMR. In addition to this, approximately 75% of respondents believed that irresponsible and inappropriate use of antimicrobials could potentially cause AMR.
Table 2. Perceptions toward antimicrobial resistance.
Antimicrobial use & appropriateness
The perceptions toward antimicrobial prescribing practices within the hospital are presented in . Pharmacists were more likely to agree that antimicrobials were overused within the hospital (p = 0.028) and that overprescribing antimicrobials was better than underprescribing (p = 0.044). A relatively limited number of respondents (26.9%) were in agreement that antimicrobial use in the hospital could be classified as highly appropriate. Of the total respondents, fewer than half (48.7%) agreed that appropriateness of antimicrobial prescriptions should be reviewed every day.
Table 3. Perceptions toward antimicrobial use in the hospital.
Antimicrobial stewardship
The perception and attitudes toward ASPs are summarized in . The majority of respondents were unfamiliar with the term ‘ASP’ (64.1%) and were currently not involved in any ASP activities (84.6%). The two ASP activities that had the most agreement among respondents to be implemented were a formal policy regulating the overall use of antimicrobials in the hospital (88.5%) and introduction of local antimicrobial guidelines and protocols (84.6%). However, no significant differences were observed with regard to the preferred ASP activities among the two groups. Compared with the physicians, pharmacists were more likely to participate in education sessions about ASP (p = 0.007) and also to commit to ASP activities (p = 0.022).
Table 4. Attitude toward antimicrobial stewardship program.
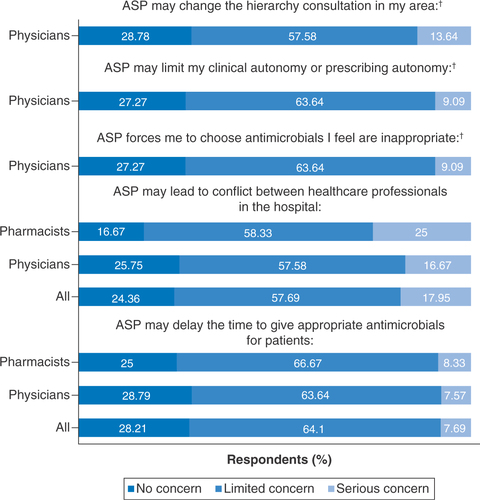
A large proportion of respondents reported concerns about the implementation of an ASP, including the timely administration of antimicrobials to patients (75.6%) and potential conflict with other healthcare professionals (71.8%) (). In addition to this, a substantial number of physicians raised concerns regarding the autonomy (72.73%) and prescribing etiquette (71.22%) in their field that may result from ASP implementation.
Discussion
This study represents a description of perceptions and attitudes among hospital-based healthcare professionals toward AMR, antimicrobial use and ASPs in an Indonesian setting. Based on the findings, considerable work needs to be undertaken to ensure successful implementation of hospital-wide ASP activities in this country.
Notably, the findings showed that healthcare professionals in the present study were aware of the problem of AMR in their hospital, as well as at national and international levels. However, the perception was that AMR was less of a problem at the study hospital when compared with the national level, a finding common to other surveys [Citation17,Citation35,Citation36]. Factors outside hospitals, in particular antimicrobial self-medication in the community, were perceived as major contributors to the development of resistant pathogens. It is worth noting that antimicrobial self-medication has been identified as a public health issue in low- and middle-income countries, including the city in which the current study was conducted [Citation46–48]. This could potentially explain why there was an impression that AMR was more of a problem outside of the study hospital.
Similar to findings from other studies [Citation49,Citation50], a limited number of respondents were of the view that antimicrobials were overused in the hospital, with pharmacists more likely to agree that overprescribing was better than underprescribing. This does not necessarily indicate that pharmacists support irresponsible use of antimicrobials, as evidenced by their awareness of the negative consequences of overprescribing antibiotics and the risk of dwindling antibiotic resources. Although the precise reasons for this finding have not been explored in the study, a tendency toward overprescribing antimicrobials may reflect a lack of clarity among pharmacists on which patients may or may not benefit from antimicrobial therapy. This may stem from the notable finding that respondent pharmacists had less experience in caring for patients with multidrug-resistant infections.
Almost three-quarters of our respondents were not confident of antimicrobial prescriptions being appropriate, a finding similar to those of previous studies [Citation51,Citation52]. There might be several reasons why the respondents believe there is a high level of inappropriate prescribing in the hospital [Citation53–56]. Firstly, guidelines to determine dose and duration of antimicrobial treatment might not always be accessible at the time of prescription, as has been documented in other studies from developing countries [Citation54–56]. Secondly, patients’ presenting signs and symptoms and concerns regarding clinical deterioration might mean that antimicrobials are prescribed pre-emptively and not according to best practice [Citation55]. For example, due to limited access to hospitals and use of alternative therapies beforehand, patients might arrive in Indonesian hospitals in relatively sicker condition compared with those in developed countries [Citation19,Citation57]. Thirdly, our respondents might not have adequate time or resources to self-evaluate the appropriateness of their own antimicrobial prescriptions, meaning there is a lack of a feedback loop to consolidate confidence in their antimicrobial prescribing.
The majority of respondents in this study welcomed any strategies to improve the appropriateness of antimicrobial prescription behavior. It is worth highlighting that the least-preferred option, that of computer-assisted stewardship, may in fact relate to inadequate access to information technology facilities within the hospital.
As has been reported in a previous study [Citation17], pharmacists were more interested in being actively involved in stewardship activities when compared with physicians. One reason for this could be related to the way in which pharmacists now perceive their role as members of the health profession [Citation58,Citation59]. Traditionally, the central role of pharmacists has been more focused on drug supply and knowledge, including dispensing, distributing and providing medical information [Citation60]. However, this role is extending to provide more patient-centered services; examples of this include pharmacists’ involvement in drug selection and reviewing the appropriateness of medications. In Indonesia, pharmacists have also been transitioning to patient-centered services [Citation60,Citation61]. For the hospital settings, the Indonesian Ministry of Health requires pharmacists to assess the appropriateness of treatment received by patients, including antimicrobials [Citation61]. It is, therefore, expected that the practices of Indonesian pharmacists nowadays extend beyond just medicine supply.
In contrast to pharmacists, almost one-half of physicians said they would not be willing to participate in ASP activities. As most physicians were supportive of ASP implementation, this finding may indicate time constraints as a barrier to being actively involved in these activities, rather than opposition to a hospital-based ASP.
A potential barrier to active involvement in antimicrobial therapy, however, may be pharmacists’ concerns about potential conflict with other healthcare professionals, including prescribers. Previous studies have commonly reported open communication with prescribers as a barrier for pharmacists to be routinely involved in ASP activities [Citation62,Citation63]. It should be acknowledged that communication among different health professionals is uniquely challenging for several reasons, including the differences in ideologies and aims, inequalities in perceived power relations and interpersonal trust barriers [Citation64,Citation65].
Identification of the roles and responsibilities of each profession are essential as a starting point to encourage a multidisciplinary framework for ASP activities [Citation66]. In addition, opening up opportunities for regular meetings and maintaining a safe, non-judgmental work environment should be encouraged, to breach fragmented interprofessional communication within the hospital [Citation66–68]. Finally, providing regular ASP workshops that focus on upskilling and training can be useful to foster relationships and trust among healthcare professionals [Citation68].
Another issue that may potentially weaken the efforts to optimize antimicrobial prescribing behavior is the physicians’ perception of the impact of stewardship activities. A large proportion of physicians (72.7%) in the present study expressed concerns over prescribing autonomy and the impact that ASP may have on ‘prescribing etiquette’ within the hospital (72.2%). It has been widely recognized that it is every physician’s privilege to prescribe antimicrobials, and such prescription may function to disclose their specialized knowledge [Citation69,Citation70]. Therefore, as also reported in another study, losing clinical and prescribing autonomy has been found to be one of the major concerns of prescribers toward the implementation of hospital-wide ASPs [Citation38]. The challenges increase because the issue is not merely about losing individual autonomy, but rather group autonomy. Medicine prescription, including antimicrobials, is mostly dictated with ‘what to prescribe’ by peer practices [Citation71,Citation72]. Moreover, it is worth noting that selection of an ‘appropriate’ antimicrobial may vary considerably between departments within a hospital [Citation73].
In view of the cultural dimensions associated with ASP implementation, the Indonesian culture is described as one with a high power distance and relatively low individualism [Citation59,Citation60]. In this context, it is widely perceived that there is disproportionate power held by a few stakeholders who essentially control ‘the rules of the game’ [Citation74,Citation75]. In addition, in a ‘collectivist society’ such as Indonesia, people’s self-image is more representative of ‘we’ rather than ‘I’. In this context, further work is required in Indonesian hospitals to determine how best to strategize ASP implementation. This may entail identifying how ASP activities can be tailored to individual hospital departments’ requirements rather than pursuing a blanket ‘one size fits all’ ASP program throughout the whole hospital [Citation71,Citation76,Citation77].
It should be noted that this study has some potential limitations. First, as has been found in other survey studies, we cannot exclude the possibility of selection bias or that respondents of this study provided socially desirable responses. However, given that an independent researcher, who is not a member of hospital staff, distributed the questionnaires and all were completed anonymously without any supervision, we affirm that respondent answers represent their sincere choices. Second, we acknowledge that approximately one-quarter of physicians did not complete the questionnaire, and this non-response rate could lead to inherent selection bias [Citation78]. However, it is generally accepted that the response rate we obtained (almost 70%) is acceptable [Citation78,Citation79]. Additionally, at least one physician from each department completed the questionnaire, and almost all heads of departments participated in our study. Third, given that this was a single-site study, the findings may not represent the perceptions and attitudes of all physicians and pharmacists across the country. This may be especially evident in private hospitals, where the working dynamics between doctors and pharmacists often differ from those in public facilities. Given that the number of private hospitals is approximately double that of their public counterparts in Indonesia, a survey administered in the private hospital setting may be worthwhile.
Conclusion
This study has identified important perceptions of AMR, antimicrobial prescription and the impact of stewardship activities among key healthcare providers involved with antimicrobial prescriptions. The majority of physicians and pharmacists were aware of the negative impacts of AMR, but this impact was thought to be less of a concern within the hospital as compared with nationally. In terms of antimicrobial use within the hospital, the differing perceptions between pharmacists and physicians could be related to the contrasting clinical experiences between the two professions. While general ASP activities were relatively well accepted by both professions, pharmacists were more eager to know more about ASP and to engage with ASP initiatives. It could therefore be suggested that designing ASP activities that enhance physician participation and utilize pharmacists as ASP champions may be a strategy worth considering. In order for this to be effective and sustainable, however, concerns toward interprofessional communication and perceived differences in hierarchy need to be addressed when designing and implementing hospital-based ASP activities.
The perception of healthcare providers in our study was that antimicrobial resistance was less of a severe problem at the study hospital when compared with the national level.
Factors outside hospitals, in particular antimicrobial self-medication in the community, were perceived as major contributors to the development of resistant pathogens.
A majority of respondents were aware that antimicrobial resistance could prolong hospital stay, increase health expenditure and lead to worse clinical outcomes.
A relatively limited number of respondents were in agreement that antimicrobial use in the hospital could be classified as highly appropriate.
Pharmacists were more likely to agree that overprescribing was better than underprescribing; this may reflect a lack of clarity among pharmacists on which patients may or may not benefit from antimicrobial therapy.
Any strategies to improve the appropriateness of antimicrobial prescription behavior in the hospital were accepted by the respondents.
Pharmacists were more interested in being actively involved in stewardship activities than physicians; however, their concerns about potential conflict with other healthcare professionals, including prescribers, may hamper their active involvement in antimicrobial stewardship programs.
From the physicians’ perspective, losing clinical and prescribing autonomy has been found as one of the major concerns toward the implementation of hospital-wide antimicrobial stewardship programs.
Author contributions
Conceptualized and designed the study protocol: E Setiawan, M Cotta, J Roberts. Obtained ethical approval from the University of Queensland: E Setiawan, M Cotta, M-H Abdul-Aziz, J Roberts. Obtained ethical approval from the research site in Indonesia: E Setiawan, H Sosilya, D Widjanarko, D Kusuma Wardhani. Data collection: E Setiawan, H Sosilya, D Widjanarko, D Kusuma Wardhani. Data analysis: E Setiawan, M Cotta, M-H Abdul-Aziz. Writing – original draft preparation: E Setiawan; review and editing: M Cotta, M-H Abdul-Aziz, J Roberts, H Sosilya, D Widjanarko, D Kusuma Wardhani. Supervision: M Cotta, J Roberts.
Ethical conduct of research
The questionnaire and methodology for this study was approved by the Human Research Ethics Committee (HREC) of The University of Queensland (approval no. 2018001341) and the Ethical Committee at the research site (approval no. 004/KE/KEPK/2019). Informed consent was obtained from all individual participants included in the study.
Acknowledgments
E Setiawan is a PhD student sponsored by an Australia Awards Scholarship from Department of Foreign Affairs and Trade (DFAT), Australian Government. J Roberts would like to acknowledge funding from the Australian National Health and Medical Research Council for a Centre of Research Excellence (APP1099452) and a Practitioner Fellowship (APP1117065).
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Additional information
Funding
References
- Cassini A , HögbergLD , PlachourasDet al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect. Dis.19(1), 56–66 (2019).
- Aslam B , WangW , ArshadMIet al. Antibiotic resistance: a rundown of a global crisis. Infect. Drug. Resist.11, 1645–1658 (2018).
- World Health Organization . 2019 Antibacterial agents in clinical development: an analysis of the antibacterial clinical development pipeline (2019). www.who.int/publications/i/item/9789240000193
- Spellberg B , BlaserM , GuidosRJet al. Combating antimicrobial resistance: policy recommendations to save lives. Clin. Infect. Dis.52(Suppl. 5), S397–S428 (2011).
- Singer AC , KirchhelleC , RobertsAP. (Inter)nationalising the antibiotic research and development pipeline. Lancet Infect. Dis.20(2), e54–e62 (2020).
- Theuretzbacher U , OuttersonK , EngelA , KarlenA. The global preclinical antibacterial pipeline. Nat. Rev. Microbiol.18(5), 275–285 (2020).
- Cox JA , VliegheE , MendelsonMet al. Antibiotic stewardship in low- and middle-income countries: the same but different?. Clin. Infect. Dis.23(11), 812–818 (2017).
- Laxminarayan R , MatsosoP , PantSet al. Access to effective antimicrobials: a worldwide challenge. Lancet387(10014), 168–175 (2016).
- Duffy E , RitchieS , MetcalfeS , Van BakelB , ThomasMG. Antibacterials dispensed in the community comprise 85%–95% of total human antibacterial consumption. J. Clin. Pharm. Ther.43, 59–64 (2018).
- Australian Commission on Safety and Quality in Health Care . AURA 2019: third Australian report on antimicrobial use and resistance in human health (2019). www.safetyandquality.gov.au/our-work/antimicrobial-resistance/antimicrobial-use-and-resistance-australia-surveillance-system/aura-2019
- Willemsen I , GroenhuijzenA , BogaersD , StuurmanA , van KeulenP , KluytmansJ. Appropriateness of antimicrobial therapy measured by repeated prevalence surveys. Antimicrob. Agents Chemother.51(3), 864–867 (2007).
- Manning ML , SeptimusEJ , AshleyESDet al. Antimicrobial stewardship and infection prevention – leveraging the synergy: a position paper update. Infect. Control Hosp. Epidemiol.39(4), 467–472 (2018).
- Karanika S , PaudelS , GrigorasC , KalbasiA , MylonakisE. Systematic review and meta-analysis of clinical and economic outcomes from the implementation of hospital based antimicrobial stewardship programs. Antimicrob. Agents Chemother.60(8), 4840–4852 (2016).
- Mas-Morey P , ValleM. A systematic review of inpatient antimicrobial stewardship programmes involving clinical pharmacists in small-to-medium-sized hospitals. Eur. J. Hosp. Pharm.25(e1), e69–e73 (2018).
- World Health Organization . Antimicrobial stewardship programmes in health-care facilities in low- and middle-income countries. A practical toolkit (2019). https://apps.who.int/iris/handle/10665/329404
- Davey P . The 2015 Garrod Lecture: why is improvement difficult?. J. Antimicrob. Chemother.70(11), 2931–2944 (2015).
- Cotta MO , RobertsonMS , TaceyMet al. Attitudes towards antimicrobial stewardship: results from a large private hospital in Australia. Healthcare Infect.19(3), 89–94 (2014).
- Ministry of Health of the Republic of Indonesia . Regulation of Ministry of Health Number 8 year of 2015 concerning antimicrobial stewardship program in the hospital settings (2015). https://peraturan.bpk.go.id/Home/Details/114886/permenkes-no-8-tahun-2015
- Mahendradhata Y , TrisnantoroL , ListyadewiSet al. The Republic of Indonesia health system review. Health Syst. Transition7(1), 1–292 (2017).
- Committee on Hospital Accreditation . 2017 National Standard on Hospital Accreditation; first edition. www.pdpersi.co.id/kanalpersi/manajemen_mutu/data/snars_edisi1.pdf
- Herawati F , JaelaniAK , WijonoHet al. Antibiotic stewardship knowledge and belief differences among healthcare professionals in hospitals: a survey study. Heliyon7(6), e07377 (2021).
- Herawati F , AnantaSC , ParwithaIAAet al. Interview-based cross-sectional needs assessment to advance the implementation of an effective antibiotic stewardship program in Indonesian hospitals. Health Policy Open1, 100002 (2020).
- Chaw PS , HöpnerJ , MikolajczykR. The knowledge, attitude and practice of health practitioners towards antibiotic prescribing and resistance in developing countries – a systematic review. J. Clin. Pharm. Ther.43(5), 606–613 (2018).
- Broom JK , BroomAF , KirbyER , GibsonAF , PostJJ. Clinical and social barriers to antimicrobial stewardship in pulmonary medicine: a qualitative study. Am. J. Infect. Control45, 911–916 (2017).
- Charani E , Castro-SanchezE , SevdalisNet al. Understanding the determinants of antimicrobial prescribing within hospitals: the role of ‘prescribing etiquette’. Clin. Infect. Dis.57(2), 188–196 (2013).
- Nicholson A , TennantI , WhiteLet al. The knowledge, attitudes and practices of doctors regarding antibiotic resistance at a tertiary care institution in the Caribbean. Antimicrob. Resist. Infect. Control7, 23 (2018).
- Sutthiruk N , ConsidineJ , HutchinsonA , DriscollA , MalathumK , BottiM. Thai clinicians’ attitudes toward antimicrobial stewardship programs. Am. J. Infect. Control46(4), 425–430 (2018).
- Baadani AM , BaigK , AlfahadWA , AldalbahiS , OmraniAS. Physicians’ knowledge, perceptions, and attitudes toward antimicrobial prescribing in Riyadh, Saudi Arabia. Saudi Med. J.36(5), 613–619 (2015).
- Labi AK , Obeng-NkrumahN , BjerrumSet al. Physicians’ knowledge, attitudes, and perceptions concerning antibiotic resistance: a survey in a Ghanaian tertiary care hospital. BMC Health Serv. Res.18(1), 126 (2018).
- Tafa B , EndaleA , BekeleD. Paramedical staffs knowledge and attitudes towards antimicrobial resistance in Dire Dawa, Ethiopia: a cross sectional study. Ann. Clin. Microbiol. Antimicrob.16(1), 64 (2017).
- Abbo L , SmithL , PereyraM , WyckoffM , HootonTM. Nurse practitioners’ attitudes, perceptions, and knowledge about antimicrobial stewardship. J. Nurse Pract.8(5), 370–376 (2012).
- Abbo LM , CosgroveSE , PottingerPSet al. Medical students’ perceptions and knowledge about antimicrobial stewardship: how are we educating our future prescribers?. Clin. Infect. Dis.57(5), 631–638 (2013).
- Salsgiver E , BernsteinD , SimonMSet al. Knowledge, attitudes, and practices regarding antimicrobial use and stewardship among prescribers at acute-care hospitals. Infect. Control Hosp. Epidemiol.39(3), 316–322 (2018).
- Fathi I , SamehO , Abu-OlloMet al. Knowledge, attitudes, and beliefs regarding antimicrobial therapy and resistance among physicians in Alexandria University Teaching Hospitals and the associated prescription habits. Microb. Drug Resist.23(1), 71–78 (2017).
- Garcia C , LlamoccaLP , GarciaKet al. Knowledge, attitudes and practice survey about antimicrobial resistance and prescribing among physicians in a hospital setting in Lima, Peru. BMC Clin. Pharmacol.11, 18 (2011).
- Abera B , KibretM , MuluW. Knowledge and beliefs on antimicrobial resistance among physicians and nurses in hospitals in Amhara Region, Ethiopia. BMC Pharmacol. Toxicol.15, 26 (2014).
- Alothman A , AlgwizaniA , AlsulaimanM , AlalwanA , BinsalihS , BosaeedM. Knowledge and attitude of physicians toward prescribing antibiotics and the risk of resistance in two reference hospitals. Infect. Dis.9, 33–38 (2016).
- Dyar OJ , PulciniC , HowardP , NathwaniD. European medical students: a first multicentre study of knowledge, attitudes and perceptions of antibiotic prescribing and antibiotic resistance. J. Antimicrob. Chemother.69(3), 842–846 (2014).
- Stach LM , HedicanEB , HerigonJC , JacksonMA , NewlandJG. Clinicians attitudes towards an antimicrobial stewardship program at a children’s hospital. J. Pediatric Infect. Dis. Soc.1(3), 190–197 (2012).
- Buckel WR , HershAL , PaviaAT , JonesPS , Owen-SmithAA , StenehjemE. Antimicrobial stewardship knowledge, attitudes, and practices among health care professionals at small community hospitals. Hosp. Pharm.51(2), 149–157 (2016).
- Bannan A , BuonoE , McLawsML , GottliebT. A survey of medical staff attitudes to an antibiotic approval and stewardship programme. Intern. Med. J.39(10), 662–668 (2009).
- Srinivasan A , SongX , RichardsA , Sinkowitz-CochranR , CardoD , RandC. A survey of knowledge, attitudes, and beliefs of house staff physicians from various specialties concerning antimicrobial use and resistance. Arch. Intern. Med.164(13), 1451–1456 (2004).
- Bujang MA , OmarED , BaharumNA. A review on sample size determination for Cronbach’s alpha test: a simple guide for researchers. Malays. J. Med. Sci.25(6), 85–99 (2018).
- Taber KS . The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res. Sci. Educ.48, 1273–1296 (2018).
- Fisher MJ , MarshallAP , MitchellM. Testing differences in proportions. Aust. Crit. Care24, 133–138 (2011).
- World Health Organization . The world medicines situation 2011 (2011). www.who.int/medicines/areas/policy/world_medicines_situation/WMS_ch14_wRational.pdf
- Puspitasari HP , FaturrohmahA , HermansyahA. Do Indonesian community pharmacy workers respond to antibiotics requests appropriately?. Trop. Med. Int. Health16(7), 840–846 (2011).
- Djawaria DPA , SetiadiAP , SetiawanE. Behavior analysis and attributed factors to non prescription antibiotic used in Surabaya. Media Kesehatan Masyarakat Indonesia14(4), 406–417 (2018).
- Abbo L , Sinkowitz-CochranR , SmithLet al. Faculty and resident physicians’ attitudes, perceptions, and knowledge about antimicrobial use and resistance. Infect. Control Hosp. Epidemiol.32(7), 714–718 (2011).
- Szymczak JE , FeemsterKA , ZaoutisTE , GerberJS. Pediatrician perceptions of an outpatient antimicrobial stewardship intervention. Infect. Control Hosp. Epidemiol.35(Suppl. 3), S69–S78 (2014).
- Tiong JJ , LooJS , MaiCW. Global antimicrobial stewardship: a closer look at the formidable implementation challenges. Front. Microbiol.7, 1860 (2016).
- Spernovasilis N , IerodiakonouD , MilioniA , MarkakiL , KofteridisDP , TsioutisC. Assessing the knowledge, attitudes and perceptions of junior doctors on antimicrobial use and antimicrobial resistance in Greece. J. Glob. Antimicrob. Resist.21, 296–302 (2020).
- Tarrant C , KrockowEM , NakkawitaWMIDet al. Moral and contextual dimensions of ‘inappropriate’ antibiotic prescribing in secondary care: a three-country interview study. Front. Sociol.5, 7 (2020).
- Saleem Z , HassaliMA , GodmanB , HashmiFK , SaleemF. Antimicrobial prescribing and determinants of antimicrobial resistance: a qualitative study among physicians in Pakistan. Int. J. Clin. Pharm.41(5), 1348–1358 (2019).
- Satti MZ , HamzaM , SajidZet al. Compliance rate of surgical antimicrobial prophylaxis and its association with knowledge of guidelines among surgical residents in a tertiary care public hospital of a developing country. Cureus11(5), e4776 (2019).
- Kagoya EK , RoyenKV , WaakoPet al. Experiences and views of healthcare professionals on the prescription of antibiotics in Eastern Uganda: a qualitative study. J. Glob. Antimicrob. Resist.25, 66–71 (2021).
- Widayanti AW , GreenJA , HeydonS , NorrisP. Health-seeking behaviour of people in Indonesia: a narrative review. J. Epidemiol. Glob. Health10(1), 6–15 (2020).
- Schindel TJ , YukselN , BreaultR , DanielsJ , VarnhagenS , HughesCA. Perceptions of pharmacists’ roles in the era of expanding scopes of practice. Res. Social Adm. Pharm.13(1), 148–161 (2017).
- Barber N , SmithF , AndersonS. Improving quality of health care: the role of pharmacists. Qual. Health Care3(3), 153–158 (1994).
- Tan CK , AslamM. The development of clinical pharmacy in Indonesia. Pharm. J.264(7098), 817–819 (2000).
- Ministry of Health of the Republic of Indonesia, Jakarta, Indonesia . Regulation of Ministry of Health Number 72 year of 2016 concerning standard of pharmacy services in the hospital settings (2016). https://peraturan.bpk.go.id/Home/Details/114491/permenkes-no-72-tahun-2016
- Broom A , BroomJ , KirbyE , PlageS , AdamsJ. What role do pharmacists play in mediating antibiotic use in hospitals? A qualitative study. BMJ Open5(11), e008326 (2015).
- Park S , KangJE , ChoiHJet al. Antimicrobial stewardship programs in community health systems perceived by physicians and pharmacists: a qualitative study with gap analysis. Antibiotics (Basel)8(4), 252 (2019).
- Steihaug S , JohannessenAK , AdnanesM , PaulsenB , MannionR. Challenges in achieving collaboration in clinical practice: the case of Norwegian health care. Int. J. Integr. Care16(3), 3 (2016).
- Rabol LI , McPhailMA , OstergaardD , AndersenHB , MogensenT. Promoters and barriers in hospital team communication. A focus group study. J. Commun. Healthc.5(2), 129–139 (2012).
- van Schaik SM , O’BrienBC , AlmeidaSA , AdlerSR. Perceptions of interprofessional teamwork in low-acuity settings: a qualitative analysis. Med. Educ.48(6), 583–592 (2014).
- Eddy K , JordanZ , StephensonM. Health professionals’ experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. JBI Database System. Rev. Implement. Rep.14(4), 96–137 (2016).
- Foronda C , MacWilliamsB , McArthurE. Interprofessional communication in healthcare: an integrative review. Nurse Educ. Pract.19, 36–40 (2016).
- Freidson E . Profession of Medicine: A Study of the Sociology of Applied Knowledge.Dodd Mead, NY, USA (1970).
- Hulscher MEJL , GrolRPTM , vander Meer JWM. Antibiotic prescribing in hospitals: a social and behavioural scientific approach. Lancet Infect. Dis.10(3), 167–175 (2010).
- Bosk CL . Occupational rituals in patient management. N. Engl. J. Med.303(2), 71–76 (1980).
- Perozziello A , RoutelousC , CharaniEet al. Experiences and perspectives of implementing antimicrobial stewardship in five French hospitals: a qualitative study. Int. J. Antimicrob. Agents51(6), 829–835 (2018).
- Mol PGM , RuttenWJMJ , GansROB , DegenerJE , Haaijer-RuskampFM. Adherence barriers to antimicrobial treatment guidelines in teaching hospital, the Netherlands. Emerg. Infect. Dis.10(3), 522–525 (2004).
- Hofstede G . Culture’s Consequences: Comparing Values, Behaviors, Institutions, and Organizations Across Nations.Sage Publications, CA, USA (2001).
- Hofstede G , HofstedeGJ , MinkovM. Cultures and Organizations: Software of the Mind (3rd Edition).McGraw-Hill, NY, USA (2010).
- Baker SN , AcquistoNM , AshleyED , FairbanksRJ , BeamishSE , HaasCE. Pharmacist-managed antimicrobial stewardship program for patients discharged from the emergency department. J. Pharm. Pract.25(2), 190–194 (2012).
- Grill E , WeberA , LohmannS , Vetter-KerkhoffC , StroblR , JauchKW. Effects of pharmaceutical counselling on antimicrobial use in surgical wards: intervention study with historical control group. Pharmacoepidemiol. Drug Saf.20(7), 739–746 (2011).
- Sjöström O , HolstD , LindSO. Validity of a questionnaire survey: the role of non-response and incorrect answers. Acta. Odontol. Scand.57(5), 242–246 (1999).
- Fincham JE . Response rates and responsiveness for surveys, standards, and the journal. Am. J. Pharm. Educ.72(2), 43 (2008).