Abstract
Aim: The aim was to study acquisition and persistence of carbapenemase-producing Enterobacteriaceae (CPE) among travelers. Materials & methods: Stools from 2001 travelers and 215 nontraveling household members, collected before and immediately post-travel as well as 1, 3, 6 and 12 months upon return, were screened for CPE. Results: Five travelers, all visiting Asia outside the Indian subcontinent, acquired CPE. One traveler persistently carried the same OXA-244 CPE up to 6 months post-travel. Three months after travel, her co-traveling spouse also became positive for this OXA-244 CPE strain, suggesting clonal transmission within this household. Conclusion: Acquisition of CPE is not restricted to travelers to the Indian subcontinent and/or to travelers seeking healthcare during travel and can persist up to at least 6 months post-travel.
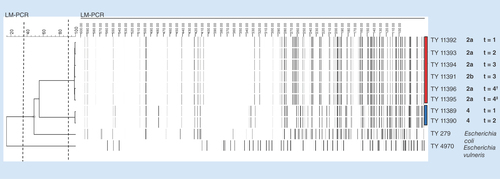
Red and blue bars indicate isolates with identical amplification fragment length polymorphism pattern. Cut-off for identical strains is set at 90% as indicated by the right dashed line.
†Isolated from chromID® ESBL agar.
‡Isolated from chromID OXA-48 agar.
2a: Subject 2a; 2b: Subject 2b; 4: Subject 4; t = 1: Within 1 week after travel; t = 2: 1 month after travel; t = 3: 3 months after travel; t = 4: 6 months after travel.
The Indian subcontinent has been identified as an important reservoir of carbapenemase-producing Enterobacteriaceae (CPE). Indeed, acquisition of CPE during travel to India has recently been reported, illustrating the risk of further global spread by travelers to this CPE-endemic region [Citation1]. However, acquisition of CPE in healthy travelers to Asian regions other than the Indian subcontinent is suggested but has not been reported from prospective studies thus far. There are a number of prospective studies on acquisition of extended-spectrum β-lactamase-producing Enterobacteriaceae (ESBL-E) and CPE in healthy travelers [Citation1–10]. Except for the above-mentioned study on CPE acquisition in travelers to India [Citation1], none of these studies identified subjects with CPE acquisition during travel.
Within the context of a large-scale prospective cohort of healthy travelers, the COMBAT study, we aimed to determine CPE acquisition, persistence of colonization and potential onward transmission.
Materials & methods
Design & data collection
As part of the COMBAT study (ClinicalTrials.gov identifier: NCT01676974), a multicenter longitudinal cohort of healthy travelers (n = 2001) and their nontraveling household members (n = 215) was followed. Participants were recruited within a period of 1 year, from November 2012 until November 2013 at the outpatient clinics run by the Academic Medical Center (Amsterdam, The Netherlands), Havenziekenhuis (Rotterdam, The Netherlands) and Maastricht University Medical Center/Public Health Service South Limburg (Maastricht, The Netherlands). Adult (≥18 years) travelers visiting one of the above-stated travel clinics, traveling abroad for a minimum of 1 week to a maximum of 3 months were eligible for participation. Minors (<18 years) and incapacitated subjects are excluded from this study. No restriction was applied with respect to travel destination.
Fecal samples (Fecal Swab®; Copan, Brescia, Italy) were collected before, immediately after (within 1–2 weeks) and 1 month after return from all participants. Follow-up fecal samples were collected 3, 6 and 12 months after return from travelers (and their household members) who acquired extended-spectrum β-lactamase-producing Enterobacteriaceae (ESBL-E) and/or CPE. Ethical approval was obtained by the Medical Ethical Committee of Maastricht University Medical Center (study number: METC 12-4-093). A full description of the study design has been published elsewhere [Citation11].
Microbiological methods
Fecal samples were enriched overnight at 35°C in TSB with vancomycin (50 mg/l) to prevent overgrowth of Gram-positive bacteria [Citation12]. Ten microliters were inoculated on chromID® ESBL agar (bioMérieux, Marcy l'Etoile, France) and incubated overnight at 35°C. Screening with this cefpodoxime-containing agar aims at maximum detection of ESBL-E. However some CPE, such as those producing OXA-48-like β-lactamases not co-producing an ESBL, remain susceptible and can be missed using this agar [Citation13]. To see what the proportion of EBSL-negative, OXA-48-positive CPE was in our cohort, a substudy was held from August until November 2013. In total, 500 consecutive post-travel samples were additionally screened for OXA-48 CPE using chromID OXA-48 agar. All colonies of different morphologies growing on any of these two agars were characterized to the species level using MALDI-TOF (Bruker, London, UK). Minimum inhibitory concentrations (MICs) were measured for all Enterobacteriaceae by the use of the Vitek 2 system (bioMérieux, Marcy l'Etoile, France).
Phenotypic confirmation of ESBL production was performed by the combination disk diffusion test according to current national Dutch guidelines [Citation14]. Isolates with MICs for imipenem >1 mg/l or for meropenem >0.25 mg/l, confirmed with E-test (bioMérieux), were considered possible carbapenemase producers [Citation14] and genotypically characterized. In case a CPE was cultured from the post-travel sample (either from the ESBL or OXA-48 agar) specific PCR for the detected carbapenemase gene was performed on fecal metagenomic DNA of the pretravel sample. All CPE suspected isolates were screened for the presence of multiple classes of ESBL and carbapenemase genes using microarray (Identibac® AMR08; Alere Technologies GmbH, Jena, Germany) [Citation15,Citation16]. Targeted PCR and DNA sequencing of the PCR-amplicons was performed with primers as described previously [Citation15,Citation17–23] and in-house primers. The underlined nucleotide from the IMI primer 5′-CAAAGCAAATGAACGATTTC-3′ was modified from [Citation23]. DNA was extracted as described by Anjum et al. [Citation15]. The lysate containing the crude DNA was used for biotin labeling and PCR.
All acquired carbapenemase-producing Escherichia coli and Klebsiella pneumoniae isolates from post-travel samples were further analyzed with multilocus sequence typing (MLST) [Citation24,Citation25] and sequence types (ST) were assigned by querying the respective MLST databases for E. coli [Citation26] and K. pneumoniae [Citation27].
To determine persistence of carriage and clonal transmission, amplification fragment length polymorphism (AFLP) [Citation28] was assayed for all consecutive CPE isolates of the travelers and their household members.
Results
More than half of all included travelers visited destinations in Asia (n = 1016/2001, 50.8%), while Africa was visited by 633 travelers (31.6%). America (mainly South and Central America), Europe and Oceania were visited by 326 (16.3%), 21 (1.0%) and 5 (0.2%) travelers, respectively.
Prior to travel, one participant was carrying an OXA-48-producing E. coli and as such excluded from subsequent analysis. This 47-year-old healthy male subject had no travel history in the previous 12 months, but had been admitted to a Dutch hospital and treated with azithromycin within the preceding 3 months.
In five travelers, CPE was detected in specimens collected immediately upon return. Specific PCR for the detected carbapenemase-encoding gene on fecal metagenomic DNA of the pretravel sample was negative in all five cases. Subject- and travel-related characteristics of the travelers who acquired CPE during travel, as well as the molecular characteristics and dynamics over time of acquired CPE isolates, are summarized in .
Out of the five travelers who acquired CPE, none had sought medical care during their travel, all but one (subject 3) reported diarrhea during travel and one traveler (subject 5) had used broad-spectrum antibiotics (). This traveler used an oral drug called Disento for complaints of watery diarrhea during travel (a mix of quinoline, aminoglycoside, nitrofuran and sulfonamide).
Out of the acquired CPEs, three isolates were E. coli of various sequence types and encoding different carbapenemase genes, one was an bla OXA-48-encoding ST363 K. pneumoniae and one an E. cloacae complex harboring an bla IMI-2 gene ().
Similar to the previous report by Ruppé et al. [Citation1], carriage of acquired CPE was of limited duration in three of our travelers, in whom CPE could not be detected 1 month after return from travel (). However, in one traveler, CPE carriage persisted at least 1 month and in another traveler (subject 2a), an OXA-244-producing E. coli isolate persisted for at least 6 months after return, as evidenced by similar AFLP patterns of isolates in follow-up specimens (). Three months after travel, an OXA-244 E. coli isolate with a similar AFLP pattern was isolated from a fecal sample collected from her spouse and travel companion (subject 2b; & ). As all other fecal specimens from this subject were CPE negative, this strongly suggests post-travel acquisition of the same bacterium through transmission from his wife.
Discussion
Our report underscores that CPE are indeed acquired during travel by healthy travelers in the absence of exposure to local healthcare during travel. Importantly, our observations also indicate that a risk of such acquisition during travel is not limited to travelers to the Indian subcontinent. In fact, none of 119 travelers in our cohort who traveled to India had acquired CPE. Instead, CPE acquisition was observed in five study participants who traveled to Europe and countries in south-eastern, eastern and western Asian, including two out of 23 visitors to Myanmar.
The low prevalence of CPE in the pretravel samples from our study (one of 2001 subjects was positive for CPE) is consistent with the very low background carriage of CPE in the Dutch community as described previously. In two studies on the prevalence and molecular characteristics of ESBL-E in the Dutch community, conducted in 2010 and 2011 and including 720 and 1033 subjects, respectively, no CPE or carbapenemase-encoding genes were found [Citation29,Citation30]. Moreover, the prevalence of carbapenemase resistance in clinical isolates in The Netherlands was only 0.01% for E. coli and 0.15% for K. pneumoniae in 2013–2014 [Citation31].
One traveler to Myanmar acquired an E. cloacae complex isolate harboring an bla IMI-2 gene. The IMI β-lactamases are a relatively uncommon group of carbapenemases. They are sporadically found in clinical isolates and environmental isolates from rivers in the USA [Citation20] and in clinical isolates from China [Citation32] and France [Citation33]. Acquisition of IMI carbapenemases in travelers has not been described yet. This acquisition shows that travel might not only play a role in the spread of more common OXA-48-like and NDM-carbapenemases, but also of rarer plasmid-encoded carbapenemases such as IMI-2.
Another traveler to Myanmar acquired an ST162 E. coli isolate carrying an bla NDM-7 gene. Although data on the prevalence of antimicrobial resistance in Myanmar are very limited, it is interesting to note that the first NDM-7 E. coli was recovered in France from urine of a female patient who also traveled to Myanmar [Citation34]. Concordantly with the isolate retrieved in our study, this isolate also harbored a bla CTX-M-15 ESBL gene, but belonged to a different sequence type (ST167).
A second bla NDM gene was acquired by a traveler when traveling throughout south-eastern and eastern Asia. NDM-producers are considered to be endemic in India and Pakistan [Citation35], but likely have spread from the Indian subcontinent to neighboring countries and throughout Asia as reflected by the acquisition of bla NDM genes in the two travelers that traveled outside these countries and confirmed by publications on the emergence of NDM-producing Enterobacteriaceae in Thailand [Citation36].
One of the 270 travelers that visited Indonesia acquired a CPE: an OXA-244 positive E. coli isolate belonging to ST38. OXA-244 is an OXA-48-like β-lactamase that exhibits weak carbapenemase activity and which differs by a single amino acid substitution from classical OXA-48 [Citation37]. ST38-type E. coli isolates harboring a classical bla OXA-48 gene have previously been recovered from Lebanon, Egypt, Turkey, Switzerland and France [Citation38–41]. More recently, the OXA-48-like variant OXA-244 was also identified in an ST38 E. coli isolated from a hospitalized patient in France without any travel history [Citation42]. To our knowledge, there are no reports of OXA-48-like harboring Enterobacteriaceae from Indonesia.
An OXA-48 harboring K. pneumoniae isolate was acquired by a traveler that visited Turkey and Greece. For many years, almost all the reports of OXA-48-producers remained from patients hospitalized in Turkey or from patients with a link to Turkey [Citation21]. The endemicity of OXA-48 in this country has most likely resulted to the acquisition in this traveler, as Greece is known as an important reservoir for KPC, but not for OXA-48 [Citation35].
Household transmission of travel-acquired CPE between healthy subjects 2a and 2b was strongly suspected, although the possibility cannot be fully excluded that subject 2b also acquired CPE during travel but that this remained undetected in initial specimens. Possible household transmission from a documented carbapenemase-producing K. pneumoniae carrier – a female with amyotrophic lateral sclerosis that required mechanical ventilation and had been hospitalized in a tertiary hospital in the Tel Aviv area – to her spouse has previously been reported [Citation43]. Another paper describes possible vertical or horizontal transmission of an NDM-1-producing Enterobacter cloacae in an Australian newborn that did not travel overseas [Citation44].
The COMBAT-study aimed at maximum detection of ESBL-E, which might have led to an underestimation of acquisition of OXA-48-like β-lactamase producers. In our subset of 500 travelers, one additional OXA-48 acquisition was found (subject 3). This indicates that likely only a few additional OXA-48 acquisitions would have been detected when all 2001 subjects would have been screened with OXA-48 agar.
Literature on antimicrobial resistance in resource-limited settings is infrequent thereby hampering the comparison between CPEs acquired by travelers and the local prevalence and molecular characteristics of CPEs at the travel destination. However, travelers may act as a sentinel for emerging local resistance in developing countries like Indonesia and Myanmar as illustrated in this paper.
Conclusion & future perspective
In conclusion, the risk of acquisition of CPE during travel is not restricted to travelers to the Indian subcontinent and/or to travelers seeking healthcare during travel and carriage of travel-acquired CPE can persist up to at least 6 months after return from travel. Prolonged carriage obviously increases the risk of onward transmission and further spread of CPE. These observations deserve consideration by healthcare providers and public health professionals worldwide. Particularly in countries with low-level prevalence of CPE, screening for CPE in patients who are admitted to healthcare facilities should be considered, not only after recent travel, but even several months after returning from high-risk countries.
Table 1. Characteristics of travelers that acquired carbapenemase-producing Enterobacteriaceae during travel, characteristics of journeys made, characteristics of acquired carbapenemase-producing Enterobacteriaceae isolates and dynamics of acquired carbapenemase-producing Enterobacteriaceae over time.
Background
Acquisition of carbapenemase-producing Enterobacteriaceae (CPE) in healthy travelers without local healthcare contact during travel has recently been described for travelers to India.
Results
This study reports acquisition of CPE in five travelers to Asia that did not travel across the Indian subcontinent.
None of these travelers had sought medical care during their travel, all but one reported diarrhea during travel and one traveler had used broad-spectrum antibiotics.
Persistence of colonization up to at least 6 months after return from travel was found for one traveler.
In one of the CPE-positive travelers evidence was found for clonal transmission of OXA-244 Escherichia coli to her spouse.
Conclusion
Acquisition of CPE during travel is neither restricted to travelers to the Indian subcontinent nor to travelers seeking healthcare during travel.
Screening for CPE in patients who are admitted to healthcare facilities should be considered, not only after recent travel, but even several months after returning from high-risk countries.
Acknowledgements
The authors would like to thank Muna Anjum and Roderick Card from the Animal Health and Veterinary Laboratories Agency (AHVLA), Weybridge, UK, for their help with the microarray.
Financial & competing interests disclosure
This study was funded by The Netherlands Organization for Health, Research and Development (ZonMw) programme Priority Medicine Antimicrobial Resistance (project number: 50-51700-98-120). The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Additional information
Funding
References
- Ruppe E, Armand-Lefevre L, Estellat C et al. Acquisition of carbapenemase-producing Enterobacteriaceae by healthy travellers to India, France, February 2012 to March 2013. Euro Surveill. 19 (14 ), pii: 20768 (2014).
- Kennedy K, Collignon P. Colonisation with Escherichia coli resistant to “critically important” antibiotics: a high risk for international travellers. Eur. J. Clin. Microbiol. Infect. Dis. 29 (12 ), 1501 – 1506 (2010).
- Tangden T, Cars O, Melhus A et al. Foreign travel is a major risk factor for colonization with Escherichia coli producing CTX-M-type extended-spectrum beta-lactamases: a prospective study with Swedish volunteers. Antimicrob. Agents Chemother. 54 (9 ), 3564 – 3568 (2010).
- Weisenberg SA, Mediavilla JR, Chen L et al. Extended spectrum beta-lactamase-producing Enterobacteriaceae in international travelers and non-travelers in New York City. PLoS ONE 7 (9 ), e45141 (2012).
- Paltansing S, Vlot JA, Kraakman MEM et al. Extended-spectrum β-lactamase-producing Enterobacteriaceae among travelers from The Netherlands. Emerg. Infect. Dis. 19 (8 ), 1206 – 1213 (2013).
- Ostholm-Balkhed A, Tarnberg M, Nilsson M et al. Travel-associated faecal colonization with ESBL-producing Enterobacteriaceae: incidence and risk factors. J. Antimicrob. Chemother. 68 (9 ), 2144 – 2153 (2013).
- Kuenzli E, Jaeger VK, Frei R et al. High colonization rates of extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli in Swiss travellers to south Asia – a prospective observational multicenter cohort study looking at epidemiology, microbiology and risk factors. BMC Infect. Dis. 14, 528 (2014).
- Lubbert C, Straube L, Stein C et al. Colonization with extended-spectrum beta-lactamase-producing and carbapenemase-producing Enterobacteriaceae in international travelers returning to Germany. Int. J. Med. Microbiol. 305 (1 ), 148 – 156 (2015).
- Kantele A, Laaveri T, Mero S et al. Antimicrobials increase travelers’ risk of colonization by extended-spectrum betalactamase-producing Enterobacteriaceae. Clin. Infect. Dis. 60 (6 ), 837 – 846 (2015).
- Angelin M, Forsell J, Granlund M et al. Risk factors for colonization with extended-spectrum beta-lactamase producing Enterobacteriaceae in healthcare students on clinical assignment abroad: a prospective study. Travel Med. Infect. Dis. 13 (3 ), 223 – 229 (2015).
- Arcilla MS, Van Hattem JM, Bootsma MC et al. The Carriage of Multiresistant Bacteria after Travel (COMBAT) prospective cohort study: methodology and design. BMC Public Health 14, 410 (2014).
- Murk JL, Heddema ER, Hess DL et al. Enrichment broth improved detection of extended-spectrum-beta-lactamase-producing bacteria in throat and rectal surveillance cultures of samples from patients in intensive care units. J. Clin. Microbiol. 47 (6 ), 1885 – 1887 (2009).
- Carrer A, Fortineau N, Nordmann P. Use of ChromID extended-spectrum beta-lactamase medium for detecting carbapenemase-producing Enterobacteriaceae. J. Clin. Microbiol. 48 (5 ), 1913 – 1914 (2010).
- Bernards AT, Bonten MJ, Cohen Stuart J et al. NVMM Guideline Laboratory detection of highly resistant microorganisms (HRMO) (2 ), 25 – 46 (2012). www.nvmm.nl/richtlijnen/hrmo-laboratory-detection-highly-resistant-microorganisms.
- Anjum MF, Choudhary S, Morrison V et al. Identifying antimicrobial resistance genes of human clinical relevance within Salmonella isolated from food animals in Great Britain. J. Antimicrob. Chemother. 66 (3 ), 550 – 559 (2011).
- Card R, Zhang J, Das P et al. Evaluation of an expanded microarray for detecting antibiotic resistance genes in a broad range of gram-negative bacterial pathogens. Antimicrob. Agents Chemother. 57 (1 ), 458 – 465 (2013).
- Pitout JD, Hossain A, Hanson ND. Phenotypic and molecular detection of CTX-M-beta-lactamases produced by Escherichia coli and Klebsiella spp. J. Clin. Microbiol. 42 (12 ), 5715 – 5721 (2004).
- Paauw A, Fluit AC, Verhoef J et al. Enterobacter cloacae outbreak and emergence of quinolone resistance gene in Dutch hospital. Emerg. Infect. Dis. 12 (5 ), 807 – 812 (2006).
- Eckert C, Gautier V, Saladin-Allard M et al. Dissemination of CTX-M-type -lactamases among clinical isolates of Enterobacteriaceae in Paris, France. Antimicrob. Agents Chemother. 48 (4 ), 1249 – 1255 (2004).
- Aubron C, Poirel L, Ash RJ et al. Carbapenemase-producing Enterobacteriaceae U.S. rivers. Emerg. Infect. Dis. 11 (2 ), 260 – 264 (2005).
- Poirel L, Potron A, Nordmann P. OXA-48-like carbapenemases: the phantom menace. J. Antimicrob. Chemother. 67 (7 ), 1597 – 1606 (2012).
- Poirel L, Dortet L, Bernabeu S et al. Genetic features of blaNDM-1-positive Enterobacteriaceae. Antimicrob. Agents Chemother. 55 (11 ), 5403 – 5407 (2011).
- Pasteran F, Mendez T, Guerriero L et al. Sensitive screening tests for suspected class A carbapenemase production in species of Enterobacteriaceae. J. Clin. Microbiol. 47 (6 ), 1631 – 1639 (2009).
- Wirth T, Falush D, Lan R et al. Sex and virulence in Escherichia coli: an evolutionary perspective. Mol. Microbiol. 60 (5 ), 1136 – 1151 (2006).
- Diancourt L, Passet V, Verhoef J et al. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J. Clin. Microbiol. 43 (8 ), 4178 – 4182 (2005).
- MLST website hosted at the Warwick University, UK. http://mlst.warwick.ac.uk/mlst/dbs/Ecoli.
- MLST website hosted at Institut Pasteur, France. http://bigsdb.web.pasteur.fr/klebsiella/klebsiella.html.
- Savelkoul PH, Aarts HJ, De Haas J et al. Amplified-fragment length polymorphism analysis: the state of an art. J. Clin. Microbiol. 37 (10 ), 3083 – 3091 (1999).
- Van Hoek AH, Schouls L, Van Santen MG, Florijn A, De Greeff SC, Van Duijkeren E. Molecular characteristics of extended-spectrum cephalosporin-resistant Enterobacteriaceae from humans in the community. PLoS ONE 10 (6 ), e0129085 (2015).
- Reuland EA, Overdevest IT, Al Naiemi N et al. High prevalence of ESBL-producing Enterobacteriaceae carriage in Dutch community patients with gastrointestinal complaints. Clin. Microbiol. Infect. 19 (6 ), 542 – 549 (2013).
- NethMap. Consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in The Netherlands in 2014. www.swab.nl/swab/cms3.nsf/uploads/.
- Huang L, Wang X, Feng Y et al. First identification of an IMI-1 carbapenemase-producing colistin-resistant Enterobacter cloacae in China. Ann. Clin. Microbiol. Antimicrob. 14 (1 ), 51 (2015).
- Dupont H, Gaillot O, Goetgheluck AS et al. Molecular characterization of carbapenem-non-susceptible Enterobacterial isolates collected during a prospective interregional survey in France and susceptibility to the novel ceftazidime-avibactam and aztreonam-avibactam combinations. Antimicrob. Agents Chemother. 60 (1 ), 215 – 221 (2015).
- Cuzon G, Bonnin RA, Nordmann P. First identification of novel NDM carbapenemase, NDM-7, in Escherichia coli in France. PLoS ONE 8 (4 ), e61322 (2013).
- Nordmann P, Poirel L. The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clin. Microbiol. Infect. 20 (9 ), 821 – 830 (2014).
- Rimrang B, Chanawong A, Lulitanond A et al. Emergence of NDM-1- and IMP-14a-producing Enterobacteriaceae in Thailand. J. Antimicrob. Chemother. 67 (11 ), 2626 – 2630 (2012).
- Oteo J, Hernandez JM, Espasa M et al. Emergence of OXA-48-producing Klebsiella pneumoniae and the novel carbapenemases OXA-244 and OXA-245 in Spain. J. Antimicrob. Chemother. 68 (2 ), 317 – 321 (2013).
- Potron A, Poirel L, Rondinaud E, Nordmann P. Intercontinental spread of OXA-48 beta-lactamase-producing Enterobacteriaceae over a 11-year period, 2001 to 2011. Euro Surveill. 18 (31 ), pii:20549 (2013).
- Dimou V, Dhanji H, Pike R, Livermore DM, Woodford N. Characterization of Enterobacteriaceae producing OXA-48-like carbapenemases in the UK. J. Antimicrob. Chemother. 67 (7 ), 1660 – 1665 (2012).
- Beyrouthy R, Robin F, Dabboussi F et al. Carbapenemase and virulence factors of Enterobacteriaceae in North Lebanon between 2008 and 2012: evolution via endemic spread of OXA-48. J. Antimicrob. Chemother. 69 (10 ), 2699 – 2705 (2014).
- Zurfluh K, Nuesch-Inderbinen MT, Poirel L et al. Emergence of Escherichia coli producing OXA-48 beta-lactamase in the community in Switzerland. Antimicrob. Resist. Infect. Control 4, 9 (2015).
- Potron A, Poirel L, Dortet L et al. Characterisation of OXA-244, a chromosomally-encoded OXA-48-like beta-lactamase from Escherichia coli. Int. J. Antimicrob. Agents 47 (1 ), 102 – 103 (2015).
- Gottesman T, Agmon O, Shwartz O et al. Household transmission of carbapenemase-producing Klebsiella pneumoniae. Emerg. Infect. Dis. 14 (5 ), 859 – 860 (2008).
- Blyth CC, Pereira L, Goire N. New Delhi metallo-beta-lactamase-producing enterobacteriaceae in an Australian child who had not traveled overseas. Med. J. Aust. 200 (7 ), 386 (2014).
