Abstract
We report a 65-year old female with advanced papillary thyroid carcinoma involving the critical vessels including common carotid artery (CCA). She initially refused surgery and lenvatinib (LEN) was used in neoadjuvant setting. Primary tumor effectively shrank by LEN without any critical adverse effect. Total thyroidectomy and modified neck dissection were curatively performed. Tumor invading into internal jugular vein exhibited remarkable response to LEN and was almost replaced with necrosis and fibrosis. CCA was surrounded by fibrosis but was smoothly dissected from tumor and preserved. The patient shows no sign of recurrence for 2 years after surgery at present. Neoadjuvant LEN treatment can be new option for locally advanced papillary thyroid carcinoma involving critical vessels, particularly CCA, to reduce risk of surgical morbidity.
(A) Computed tomography examination revealed a large irregular thyroid tumor that completely encased left internal jugular vein, involving left subclavian vein. Left common carotid artery (CCA) was involved at almost 270° by tumor (arrow). Left subclavian artery was contacted with tumor at approximately 180° (arrowhead) (left column, before LEN). (B) Tumor dramatically decreased in size after 7-week LEN administration. Arrow indicates tumor necrosis that contacted with left CCA (right column, after LEN).
LEN: Lenvatinib.
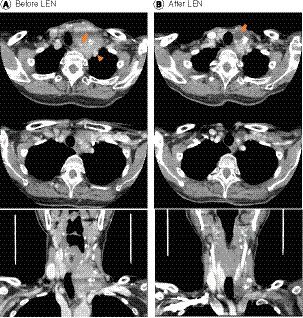
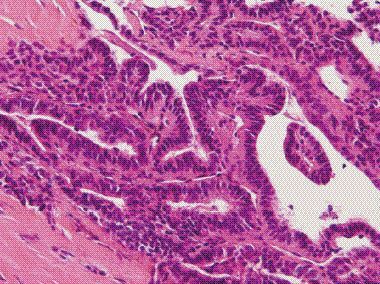
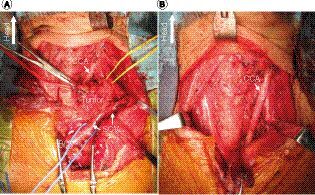
Image during surgery before (A) and after (B) tumor resection. (A) Although, the tumor size was remarkably reduced by LEN treatment, the tumor was still invasive in inferior and dorsal side, resulting in involvement of left venous angle. (B) Left CCA was successfully detached from tumor and preserved intact.
BCV: Brachiocephalic vein; CCA: Common carotid artery; LEN: Lenvatinib; SCV: Subclavian vein.
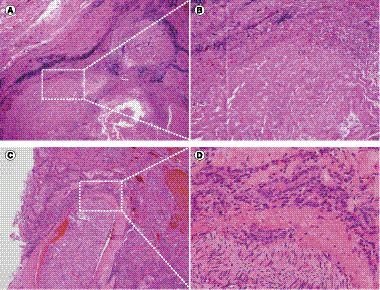
Microscopic images of surgical specimen: (A & C): 20x; (B & D): 200x. (A & B) Hematoxylin and eosin (H&E) and Elastica-van-Gieson staining focusing on encased internal jugular vein revealed that tumor was replaced with necrotic tissue and fibrosis, and viable tumor cell was not observed in this area. (C) & D) H&E staining of mediastinal part of tumor represents viable tumor cell infiltration around recurrent laryngeal nerve.
Papillary thyroid cancer (PTC) is the most common differentiated thyroid cancer (DTC) accounting for more than 90% of all thyroid cancers, and mostly exhibit excellent prognosis [Citation1,Citation2]. However, approximately 10% of patients with PTC still show locally advanced or metastatic disease [Citation1]. Locally advanced PTC can further involve important structures in the neck such as trachea, esophagus and critical blood vessels [Citation3]. In order to achieve curative resection, such critical structures may be sacrificed, leading to possible impairment of quality of life or severe complications. Although, involvement of critical arteries such as common carotid artery (CCA) predicts poor prognosis, PTC involving CCA can be curatively resected with favorable outcome in selected patients [Citation4,Citation5]. The dilemma between curability and the relatively high incidences of severe complications after curative surgery to CCA involvement makes the decision-making difficult.
Multitargeted tyrosine kinase inhibitors (TKIs) are recently indicated for treatment against radioactive iodine-refractory metastasis of DTC that can result in symptomatic or life-threatening disease [Citation1,Citation6]. The application of TKIs to neoadjuvant setting has not been recommended in the current DTC guidelines [Citation1] because of those critical risks of adverse effects such as lethal hemorrhage and fistula to trachea or skin caused by tumor shrinkage. Here, we report neoadjuvant use of lenvatinib (LEN) to a patient presenting with locally advanced PTC involving CCA, allowing curative resection without any critical adverse effect.
Case presentation
A 65-year old woman complained of growing mass on her left neck, cough and hoarseness. She presented with a large hard immobile irregular mass on her left anterior neck upon physical examination. Ultrasonography and computed tomography (CT) displayed 50 × 30 × 34 mm irregular tumor in the left thyroid lobe with invasive extension postero-laterally, which completely encased left internal jugular vein, involving part of left subclavian vein. Left CCA was involved almost 270° by tumor, suggesting CCA encasement (, left panels). Left subclavian artery was also contacted with tumor at approximately 180°. No sign of distant metastasis was detected. Fine needle aspiration cytology proved papillary thyroid carcinoma (PTC). Core needle biopsy revealed well differentiated PTC (), with 4% MIB-1 labeling index at the maximum and 70–80% p53 labeling index and poorly differentiated component was not observed. She was diagnosed eligible for curative resection with possible left carotid artery bypass. However, she refused immediate invasive surgery with artery bypass. Accordingly, after informed consent on potential severe risks of lenvatinib (LEN) especially lethal hemorrhage by rupture of carotid artery, she was treated with LEN in neoadjuvant setting. LEN administration was started at 24 mg daily. After 2 weeks, LEN was reduced to 20 mg due to grade 2 nausea and vomiting and then was further decreased to 14 mg. After 2 weeks of LEN induction, serum thyroglobulin level temporally elevated to 774.2 ng/ml 7 weeks after LEN induction, CT scan showed approximately 40% reduction of tumor in maximum diameter (, right panels). Reflecting the tumor shrinkage, serum thyroglobulin level was decreased from initial 158 ng/ml to 9.51 ng/ml. However, the remarkable tumor shrinkage was accompanied by tumor necrosis which exposed to left CCA in CT scan (, right panel). Therefore, LEN was immediately withdrawn to avoid the risk of lethal hemorrhage from CCA. After 8 months of withdrawal of LEN administration, patient finally consented to curative surgery. Pre-operative CT scan revealed no sign of obvious regrowth after 10 months of withdrawal, but consistently exist enhanced viable tumor in the posterior and inferior part similarly as in . Correspondingly, serum thyroglobulin level was stable around 11 ng/ml until curative surgery. Curative surgery was achieved by total thyroidectomy and a modified left neck dissection with combined resection of left internal jugular vein, left laryngeal recurrent nerve and left vagus nerve and wedge resection of left subclavian vein, using L-shaped partial sternotomy. Of note, left CCA was loosely adherent to the tumor, therefore, left CCA was successfully detached and preserved (). On the other hand, tumor was still invasive in inferior and dorsal side as expected on preoperative CT scan (B & A), that required resection of left vagus nerve and wedge resection of left subclavian vein. Pathological findings proved that tumor cells which encased internal jugular vein were completely replaced by necrotic tissue and fibrosis, and viable tumor cell was not observed in this area (A & B), while viable tumor cells were seen in dorsal mediastinal part of tumor, represented by infiltrating tumor cells into recurrent laryngeal nerve (C & D). The I-131 whole body scan (WBS) at adjuvant radio-active iodine (RAI) therapy (1110 MBq) revealed modest uptake only in the thyroid bed. Stimulated serum thyroglobulin level was 0.45 ng/ml at adjuvant RAI therapy. WBS (387.5 MBq) at 15 months after surgery showed disappearance of RAI uptake in thyroid bed as well as other abnormal uptake, suggesting successful RAI treatment. Stimulated serum thyroglobulin level was 0.54 ng/ml at WBS. The patient shows no sign of recurrence for 31 months after surgery at present with stable serum thyroglobulin level at around 0.09–0.21 ng/ml.
Discussion
In this report, we proposed neoadjuvant application of LEN in locally advanced PTC which involved critical vessels, particularly CCA, to reduce surgical morbidity and further contribute to complete surgical clearance of cancer. Locally advanced PTC can involve adjacent critical structures such as trachea, esophagus and critical blood vessels [Citation3]. Although the involvement of such critical structures is not a contraindication to surgery, risks of significant morbidity and mortality with uncertain survival benefits raise questions to conducting aggressive surgery [Citation7]. Particularly, an aggressive surgical approach to thyroid cancer which involves CCA is still on debate. Radical resections of tumor are important to attain oncological clearance. Indeed, a previous report demonstrated that subadventitial resection achieved good locoregional control for PTC with carotid artery invasion [Citation8]. Under the dilemma in the midst of surgical morbidity and benefits, an aggressive surgery should be carefully selected considering benefits of optional treatment, comorbidity, general condition and patient’s background.
Multitargeted TKIs are recently indicated for treatment against radioactive iodine-refractory DTC with excellent prognostic efficacy [Citation1,Citation6]. Recently, TKIs have been reported to have a potential neoadjuvant role in selected cases of locally advanced or unresectable DTC to reduce tumor volume and surgical morbidity [Citation9–15] as well as in anaplastic thyroid carcinoma [Citation16,Citation17]. However, the neoadjuvant application of TKIs has not been recommended in the current DTC guidelines [Citation1] and is still on debase because of those critical adverse effects such as lethal hemorrhage, or fistula which are caused by rapid tumor shrinkage. Particularly, TKI application to tumor encasing CCA may cause lethal hemorrhage which is hard to control once it occurs. Accordingly, to our knowledge, the present report is first report of neoadjuvant TKI application in patients with advanced thyroid carcinoma involving CCA. Indeed, in the present case, LEN significantly reduced tumor volume, but the rapid tumor shrinkage cased tumor necrosis which may widely contact CCA (B). Immediate withdrawal of LEN was required to avoid lethal hemorrhage by CCA rupture. CCA was successfully detached from tumor and preserved (). At the time of this neoadjuvant use in this patient in early 2017, since there was no article on the appropriate starting dose or efficacy in lower doses of LEN in patients with locally advanced disease, we initially started at 24 mg of LEN and gradually decreased the dose. However, as a previous article recently suggested the importance of individual dose adjustment to reduce the risks of LEN-induced fistula and bleeding [Citation18], we now recommend lower doses of LEN induction in patients with locally advanced disease involving CCA, trachea, skin or esophagus.
Great vessel, particularly CCA, invasion should be carefully evaluated prior to treatment. CCA invasion can be predicted by circumferential involvement of 180° on CT or 270° on MRI [Citation19–21]. In the present case, 270° of involvement of CCA was observed on CT (A). Most importantly, prior to decide treatment strategy of neoadjuvant TKI administration, critical risks of TKI application should be meticulously informed to patients.
Conclusion & future perspective
In conclusion, we report neoadjuvant LEN application to an invasive PTC that involved CCA. And neoadjuvant LEN treatment successfully reduced tumor and potential morbidity of surgery in advanced PTC involving critical vessels. LEN in neoadjuvant setting may be an option to reduce surgical morbidity and further perform complete clearance of cancer.
Summary points
First choice of curative treatment is undoubtedly surgery in locally advanced papillary thyroid carcinoma (PTC) if it is resectable.
However, the dilemma between curability and the relatively high incidence of severe surgical complications in case of advanced PTC involving common carotid artery makes the decision-making difficult.
Neoadjuvant lenvatinib treatment can be a new option for locally advanced PTC involving critical vessels, particularly common carotid artery, to reduce risk of surgical morbidity and further contribute to complete surgical clearance of cancer.
Since rapid tumor shrinkage by lenvatinib can cause lethal hemorrhage and fistula to trachea or skin, careful follow-up and sufficient informed consent are prerequisite.
Informed consent disclosure
Written informed consent to keep personal and clinical data and to use them for research purposes was obtained from the patient at the beginning of the therapy.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- HaugenBR, AlexanderEK, BibleKC et al. 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1), 1–133 (2016).
- ShermanSI. Thyroid carcinoma. Lancet 361(9356), 501–511 (2003).
- MorrisLG, MyssiorekD. Improved detection does not fully explain the rising incidence of well-differentiated thyroid cancer: a population-based analysis. Am. J. Surg. 200(4), 454–461 (2010).
- KrolE, BrandtCT, Blakeslee-CarterJ et al. Vascular interventions in head and neck cancer patients as a marker of poor survival. J. Vasc. Surg. 69(1), 181–189 (2019).
- ManzoorNF, RussellJO, BrickerA et al. Impact of surgical resection on survival in patients with advanced head and neck cancer involving the carotid artery. JAMA Otolaryngol. Head Neck Surg. 139(11), 1219–1225 (2013).
- SchlumbergerM, TaharaM, WirthLJ et al. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N. Engl. J. Med. 372(7), 621–630 (2015).
- GuoY, PangMC, TeoCE, ChngJK. Carotid artery involvement in advanced recurrent head and neck cancer: a case report and literature review. Ann. Vasc. Surg. 56, 355e311–355e315 (2019).
- MoritaniS. Appropriateness of subadventitial resection for invasion of the carotid artery by papillary thyroid carcinoma. World J. Surg. 43(2), 519–526 (2019).
- DanilovicDLS, CastroGJr, RoitbergFSR et al. Potential role of sorafenib as neoadjuvant therapy in unresectable papillary thyroid cancer. Arch. Endocrinol. Metab. 62(3), 370–375 (2018).
- GayS, MontiE, TrambaioloAntonelli C et al. Case report: lenvatinib in neoadjuvant setting in a patient affected by invasive poorly differentiated thyroid carcinoma. Future Oncol. 15(24s), 13–19 (2019).
- HartlDM, GuerlainJ, BresuskinI et al. Surgery in the context of kinase inhibitor therapy for locally invasive thyroid cancer. Eur. J. Surg. Oncol. 46(4 Pt A), 650–655 (2020).
- NavaCF, ScheffelRS, CristoAP et al. Neoadjuvant multikinase inhibitor in patients with locally advanced unresectable thyroid carcinoma. Front Endocrinol (Lausanne). 10, 712 (2019).
- StewartKE, StrachanMWJ, SrinivasanD, MacNeillM, WallL, NixonIJ. Tyrosine kinase inhibitor therapy in locally advanced differentiated thyroid cancer: a case report. Eur. Thyroid J. 8(2), 102–107 (2019).
- TsuboiM, TakizawaH, AoyamaM, TangokuA. Surgical treatment of locally advanced papillary thyroid carcinoma after response to lenvatinib: a case report. Int. J. Surg. Case Rep. 41, 89–92 (2017).
- IwasakiH, TodaS, ItoH et al. A case of unresectable papillary thyroid carcinoma treated with lenvatinib as neoadjuvant chemotherapy. Case Rep. Endocrinol. 2020, 6438352 (2020).
- CabanillasME, FerrarottoR, GardenAS et al. Neoadjuvant BRAF- and immune-directed therapy for anaplastic thyroid carcinoma. Thyroid 28(7), 945–951 (2018).
- WangJR, ZafereoME, DaduR et al. Complete surgical resection following neoadjuvant dabrafenib plus trametinib in BRAF(V600E)-mutated anaplastic thyroid carcinoma. Thyroid 29(8), 1036–1043 (2019).
- StaubY, NishiyamaA, SugaY, FujitaM, MatsushitaR, YanoS. Clinical characteristics associated with lenvatinib-induced fistula and tumor-related bleeding in patients with thyroid cancer. Anticancer Res. 39(7), 3871–3878 (2019).
- YooGH, HocwaldE, KorkmazH et al. Assessment of carotid artery invasion in patients with head and neck cancer. Laryngoscope 110(3 Pt 1), 386–390 (2000).
- YousemDM, HatabuH, HurstRW et al. Carotid artery invasion by head and neck masses: prediction with MR imaging. Radiology 195(3), 715–720 (1995).
- YuQ, WangP, ShiH, LuoJ. Carotid artery and jugular vein invasion of oral-maxillofacial and neck malignant tumors: diagnostic value of computed tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 96(3), 368–372 (2003).
