Abstract
Aim: Understand the frequency, nature and over-the-counter (OTC) self-management of patient-reported severe acute pain occasions. Patients & methods: A consumer-based survey of adults experiencing acute pain in Australia, Russia and the UK. Participants recorded pain type, frequency and intensity plus action taken to address pain. Results: A total of 2994 participants completed the survey; 1366 provided ≥1 diary entry (total 6527 pain occasions). Of these, 744 (11%) were reported as severe, and 72% were treated with OTC medication. Participants were somewhat satisfied/very satisfied with the action taken for 87% of pain occasions overall, and for 83% of severe pain episodes; however, participants with severe pain were somewhat/very dissatisfied with treatment in 9% of cases. Conclusion: Acute pain episodes described as ‘severe’ are not uncommon in the self-management setting; most can be managed successfully with self-medication. Individuals seeking strong OTC pain relief should be supported to consider self-management strategies first, before considering prescription medication.
Acute pain is described as “the physiologic response to and experience of noxious stimuli that can become pathologic, is normally sudden in onset, time limited, and motivates behaviors to avoid potential or actual tissue injury” [Citation1]. Acute pain is commonplace in primary care and represents one of the most frequent complaints encountered by primary care physicians; in the USA it accounts for nearly one-half of patient visits [Citation2].
Acute pain which persists for longer than 3 months is generally classified as chronic pain [Citation3], and this progression from transient to persistent pain is known as ‘chronification’ [Citation4]. Not only can suboptimal management of acute pain have immediate negative consequences for various aspects of an individual’s health, quality of life and daily functioning [Citation5], there is increasing evidence of an association between the level of acute pain and risk for developing chronic pain, with more severe pain associated with a higher risk of developing chronic pain [Citation5–8]. Therefore, early intervention to interrupt the cascade of events that enables chronification is essential, as chronic pain may involve irreversible pathophysiological changes [Citation4].
A variety of over-the-counter (OTC) analgesics exist for the self-management of acute pain relief, and their use is commonplace. The prevalence of OTC analgesic use varies by country, estimated to range from 25% of the population over three months in Germany [Citation9], to 76% over 1 month in the USA [Citation10]. However, selecting the appropriate OTC analgesic for each pain occasion involves multiple considerations, including the type/cause of pain (since they are not universally effective for all types of pain) [Citation11,Citation12], and relative efficacy and safety, both of which vary considerably [Citation13,Citation14].
In addition to pharmacological interventions, a variety of nonpharmacological interventions may also be beneficial for patients with acute pain, depending on the cause. For example, superficial heat application, transcutaneous electrical nerve stimulation, acupuncture, relaxation therapy, exercise and cognitive behavioral therapy, have been employed with varying degrees of success [Citation15,Citation16].
Studies characterizing acute pain and its treatment are frequent in the postsurgical or emergency department setting. However, studies exploring acute pain in the self-management setting – that is, pain that patients would generally manage themselves without consulting a doctor – are lacking. The aim of this survey was to explore the nature and prevalence of acute pain described as severe by a self-medicating adult population, and how well it is addressed with current self-management strategies. Our hypothesis was that acute pain described by individuals as severe would be uncommon in the OTC setting, and that self-medication of these severe pain episodes would not always be optimal.
Patients & methods
Study design
This was a two-stage, consumer-based survey carried out from September to December 2017 in Australia, Russia and the UK. It consisted of an initial online survey, followed by in-depth diary entries for individual pain occasions.
Study population
The study population consisted of men and women aged 18–65 years recruited from an established online market research panel. From this panel, an initial general population sample was selected for each country and emailed with an invitation to participate, with the aim of achieving approximately 1000 eligible participants for each country. All participants provided informed consent prior to starting the study.
Survey
The online screening survey included questions on demographics, a multiple response question on types of pain experienced and a single-response question about typical frequency (‘every day’ to ‘less than once a year’).
Eligible participants had experienced physical aches or pains within the previous month and considered taking OTC pain medication. In addition, painful episodes had to occur with an average frequency at least once a month and up to once or twice a day. Exclusions were working in healthcare-related industries, journalism, marketing or advertising.
Diaries
Diaries were completed for individual pain occasions that had occurred in the previous 24 h. Diary questions established the predominant type of pain, its severity (mild, average or severe), time of day, the action or treatment taken and why and satisfaction with treatment.
To preserve data quality, pain occasion data were collected for a maximum of seven separate occasions with each participant making daily diary entries over a period of up to 4 weeks. Data were weighted to take account of the differences in reporting period for participants reporting frequent versus infrequent pain.
Analyses
The data are presented descriptively.
Results
Study population
In total, 8811 people were screened. Of these, 2994 met the eligibility criteria and completed the online survey, including 995 from Australia, 1000 from Russia and 999 from the UK. Baseline demographics with respect to age and gender were similar across the three countries (). Of the 2994 participants who completed the online survey, 1366 provided one or more diary entries detailing their pain occasions, for a total of 6527 pain occasions. These comprised 2160 pain occasions from participants in Australia, 2205 in Russia and 2161 from the UK.
Table 1. Demographics of participants who completed the online survey and met all eligibility criteria.
Of the 6527 pain occasions, 60% were reported by women and 40% reported by men, and the occasions represented all age groups, including 18–25 years (10%), 26–35 years (24%), 36–45 years (24%), 46–55 years (24%) and 56–65 years (18%) of age.
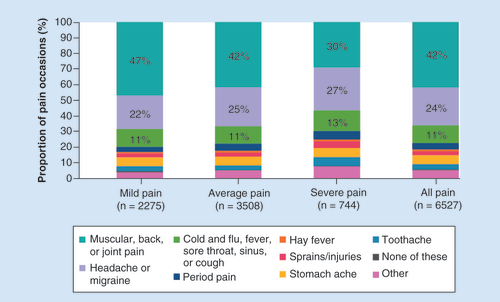
Overall, musculoskeletal pain (muscular pain, back pain and joint pain) accounted for the highest proportion of all pain occasions (42%), followed by headache and migraine (24%) and pain associated with cold and flu-related symptoms (11%) ().
Table 2. Type of pain occasion† and severity.‡
Pain intensity
Overall, 11% (744/6527) of all pain occasions were considered to be severe (); 11% (235/2160) of pain occasions in Australia, 15% (322/2205) in Russia and 9% (187/2161) in the UK. Of the 744 severe pain occasions, 68% were reported by women and 32% by men. Severe pain occasions were reported by those aged 18–25 years (12%), 26–35 years (23%), 36–45 years (23%), 46–55 years (23%) and 56–65 years (19%).
Headache or migraine accounted for 27% of the 744 severe pain occasions, with 30% due to musculoskeletal pain (back, muscular or joint pain) and 13% due to cold and flu-related symptoms (cold and flu, fever, sore throat, sinus or cough) (). Severe pain occasions were also due to toothache (6%), stomach ache (6%), sprains and injuries (4%), period pain (6%), hay fever (1%) and other (7%).
Diary question (single response): “And which of these pains was the ONE predominant/most intense pain you experienced today?” These data were broken down based on response to diary question (single response): “Thinking of this predominant/most intense symptom, how strong were these symptoms today?”.
Severe pain occasions were experienced throughout the day and night (). Nearly one in five of the 744 severe pain occasions (18%) were experienced all day long compared with 10% for average pain occasions and 8% for mild pain occasions ().
Table 3. Time of day of 6527 pain occasions.†
Pain management
Action was taken to address the pain on most of the 6527 occasions, including OTC (54%) and prescription (7%) pain relief medication (). The most frequent treatment was ibuprofen or paracetamol (data not shown). Of the 744 severe pain occasions, 72% were treated with OTC medication, 18% with prescription medication, 8% by other means and 12% of severe occasions were not treated ().
Table 4. Pain relief action taken for 6527 pain occasions.†
The most important reasons cited for choosing which treatment or action to take (n = 4238 pain occasions where treatments or actions were taken) included suitable for the pain experienced (30%), a trusted brand (22%), convenient to take (21%), good value (20%) and a fast onset of action (19%). Other frequent reasons included broad symptom relief (18%), suitable for mild pain and easy to use (both 17%), prevented pain worsening and without side effects (both 16%), as well as also giving long-lasting pain relief and allowing a return to normality (both 15%). A need for strong pain relief was cited as the reason for choosing which treatment or action to take in 14% of pain occasions (n = 4238 pain occasions where treatments or actions were taken).
Overall, most participants were somewhat satisfied/very satisfied with the treatment or action taken for most pain occasions (). With respect to the 656 severe pain occasions for which participants took treatment or action, most were associated with a report of the participant being somewhat (47%) or very (36%) satisfied with treatment, and 8% were neither satisfied nor dissatisfied. Almost one in ten severe pain occasions were associated with a report of the participant being somewhat (8%) or very (1%) dissatisfied with treatment (). Dissatisfaction rates were lower for those pain occasions described as mild or average ().
Table 5. Satisfaction with action taken or medication used for 4232 treated pain occasions.†
Discussion
Summary
This survey showed that pain occasions described by participants as severe are not uncommon in the self-management setting. Severe pain was most commonly associated with headache or migraine, musculoskeletal pain (back, muscular or joint pain) and cold and flu-related symptoms (cold and flu, fever, sore throat, sinus or cough), and to a lesser extent, toothache, stomach ache, sprains and injuries, and period pain. The majority of pain episodes were managed successfully with OTC medications, and satisfaction with pain management, even episodes described as severe, was high. However, nearly one in ten severe pain occasions were not managed satisfactorily, suggesting that there is still room for improvement of pain management in the OTC setting.
Strengths & limitations
The strength of this study was that the survey was conducted in a sizeable sample across three countries and addresses the relatively unexplored area of severe acute pain. However, this study has several limitations. Firstly, the cohort describing their pain as severe was insufficient to allow anything other than a descriptive analysis of the findings. In addition, the data did not allow for a more detailed exploration of the specific treatment/action taken for each pain occasion and its association with satisfaction. This would have helped to identify whether participants reporting dissatisfaction with their current treatment approach required stronger pain relief with an alternative OTC analgesic, a prescription analgesic and/or another form of therapy.
Lastly, codeine was not available OTC in Russia at the time of the survey due to up scheduling to prescription-only, but was available in Australia and the UK. The impact, if any, on the dissatisfaction rates in the survey is likely to have been minimal, as the majority of OTC products used by participants were ibuprofen or paracetamol (data not shown).
Comparison with existing literature
The findings of this study are consistent with results from previous research. Overall, musculoskeletal pain is one of the biggest disease burdens globally [Citation17]. Acute low back pain often becomes chronic [Citation18], and is particularly debilitating, causing more disability than any other condition on a global basis and resulting in difficulty dressing, sitting, standing, walking and lifting, as well as affecting sleep and mental state [Citation19]. Severe headache or migraine was reported in 17% of people in one US survey [Citation20], while dysmenorrhea (period pain) has been reported to affect anywhere between 37 and 91% of women of reproductive age [Citation21,Citation22], with up to a third experiencing severe pain [Citation22].
Surprisingly, in this survey over one in ten acute pain episodes were described by participants as severe. Consistent with other studies that show that sex differences exist in how individuals describe and quantify pain [Citation23,Citation24], this survey showed a higher proportion of women reporting severe pain occasions compared with men. Acute pain categorized as severe is frequently encountered in the postsurgical and emergency department settings [Citation25–29], however, in our opinion it would seem unlikely that healthcare professionals (HCPs) would consider pain intensity that can be effectively controlled in a self-management setting as comparable to these. The subjective nature of pain means it is difficult to define, so both patients and HCPs find it difficult to apply descriptions of mild, moderate and severe consistently; studies have repeatedly shown that physicians rate patients’ pain severity significantly lower than patients rate their own pain [Citation30–32]. From a clinical, ‘practical’ perspective, pain is how any individual chooses to define it at the time it occurs; however, for HCPs, being able to quantify the nature and intensity of pain is key to providing optimal pain management [Citation33]. Further research is needed to explore the relationship between patients’ and HCPs’ grading of pain severity in the self-management setting, to ensure effective communication around pain relief needs.
This survey suggests that current self-management strategies, including OTC analgesics in the majority of cases, meet the needs of most people, even those reporting severe pain episodes. However, given that there was dissatisfaction with pain relief in 9% of severe pain episodes, there is still room for improvement.
A Cochrane overview of the efficacy of 21 OTC analgesics, based on ten Cochrane reviews plus an additional study, showed that pain relief success rates varied markedly across drugs [Citation14]. Of all the regimens analyzed, fixed-dose combinations of ibuprofen–paracetamol (doses of 400/1000 and 200/500 mg) were the most effective, with a success rate of 67–70% and a number needed to treat (NNT) of 1.5–1.6. In comparison, fast-acting ibuprofen 200 and 400 mg had a success rate of 50% and an NNT of 2–3, while paracetamol alone had a success rate of 40% and an NNT of 3–5, depending on dosage [Citation14]. Aspirin was the least effective, with a success rate of only 11% [Citation14]. A separate Cochrane safety review in single-dose usage showed that combinations of ibuprofen and paracetamol were associated with significantly fewer adverse events compared with placebo [Citation13]. These findings suggest that people experiencing more intense acute pain unrelieved by single-agent therapy may benefit from ibuprofen in combination with paracetamol prior to stepping up to prescription analgesia or to codeine-based therapy [Citation34,Citation35].
Implications for practice
Even in the self-management setting, many patients experience pain that they describe as severe, and that they experience both during the day and at night. This survey has demonstrated that, in the majority of cases, this pain can be effectively treated by the individual themselves, without the need for prescription medication. Given current pressures on healthcare services, responsible and appropriate self-medication has the potential to impact positively on these pressures. Supported by pharmacists and other primary care HCPs, when appropriate, most individuals should be encouraged to explore and exhaust self-management pain relief options before seeking prescription medication.
Conclusion
This survey was conducted to assess the nature and frequency of severe pain occasions, as well as the degree of satisfaction with currently available OTC treatments. Pain episodes described by individuals as severe were not uncommon in the self-management setting, and the majority of these episodes were managed effectively with OTC medications. However, somewhat higher dissatisfaction rates were reported for pain occasions reported as severe, suggesting that some patients may require additional support from an HCP to optimize their pain management strategy on occasions when stronger pain relief is required. Given the high levels of effectiveness of self-medication in this survey, even in pain that is reported as severe, HCPs should consider encouraging individuals in an OTC setting to exhaust self-management pain strategies first, before considering prescription medication.
There is a lack of information on the nature, frequency and management of severe acute pain in the self-management setting.
This two-stage, consumer-based survey, comprised an initial online survey followed by in-depth diary entries for individual pain occasions.
Men and women aged 18–65 years were recruited from a market research panel and invited by email to participate.
Eligible participants had experienced pain within the previous month and considered taking over-the counter (OTC) medication.
They were asked to complete diaries to establish the type and severity of pain, treatment taken and satisfaction with treatment.
11% of pain episodes were described by participants as severe and these pain episodes were more likely than mild or average episodes to be experienced all day long and during the night.
Headache or migraine accounted for 27% of the 744 severe pain occasions, with 30% due to musculoskeletal pain (back, muscular or joint pain) and 13% due to cold and flu-related symptoms (cold and flu, fever, sore throat, sinus or cough).
83% of severe pain episodes were managed satisfactorily, and the majority (72%) were treated with OTC analgesia, highlighting the effectiveness of self-management strategies for pain in the OTC setting.
However, participants were dissatisfied with the pain relief achieved in almost one in ten cases of severe pain, suggesting that there is still scope for improvement in the OTC setting.
Healthcare professionals, such as pharmacists, have a key role to play in providing evidence-based guidance to people looking for stronger pain relief, and in ensuring that all self-management options (both OTC and nonpharmacological) are explored before seeking prescription analgesia.
Author contributions
All authors have contributed to the preparation of this manuscript, including its conception and critical review, and have approved the final draft and accept full responsibility for its content.
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
Acknowledgments
The authors would like to thank the participants of the study, who gave up their time to complete the survey and record in-depth diary entries.
Financial & competing interests disclosure
All the authors are employees of Reckitt Benckiser Healthcare Ltd, UK. This study was conducted by Winkle BV (477d, Keizersgracht Amsterdam, 1017 DL Netherlands) and was funded by Reckitt Benckiser Healthcare Ltd, UK. Participants received an incentive after completion of the diary phase of the study. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Medical writing assistance was provided by Sarah Johnson, Elements Communications Ltd, Westerham, UK and was funded by Reckitt Benckiser Healthcare Ltd, UK.
Additional information
Funding
References
- Kent ML , TighePJ , BelferIet al. The ACTTION-APS-AAPM pain taxonomy (AAAPT) multidimensional approach to classifying acute pain conditions . J. Pain.18 ( 5 ), 479 – 489 ( 2017 ).
- McCarberg BH . Pain management in primary care: strategies to mitigate opioid misuse, abuse, and diversion . Postgrad. Med.123 ( 2 ), 119 – 130 ( 2011 ).
- Treede RD , RiefW , BarkeAet al. A classification of chronic pain for ICD-11 . Pain.156 ( 6 ), 1003 – 1007 ( 2015 ).
- Pergolizzi JV Jr , RaffaRB , TaylorRJret al. Treating acute pain in light of the chronification of pain . Pain Manag. Nurs.15 ( 1 ), 380 – 390 ( 2014 ).
- Sinatra R . Causes and consequences of inadequate management of acute pain . Pain Med.11 ( 12 ), 1859 – 1871 ( 2010 ).
- Poleshuck EL , KatzJ , AndrusCHet al. Risk factors for chronic pain following breast cancer surgery: a prospective study . J. Pain.7 ( 9 ), 626 – 634 ( 2006 ).
- Katz J , JacksonM , KavanaghBP , SandlerAN . Acute pain after thoracic surgery predicts long-term post-thoracotomy pain . Clin. J. Pain.12 ( 1 ), 50 – 55 ( 1996 ).
- Pluijms WA , SteegersMA , VerhagenAF , SchefferGJ , Wilder-SmithOH . Chronic post-thoracotomy pain: a retrospective study . Acta. Anaesthesiol. Scand.50 ( 7 ), 804 – 808 ( 2006 ).
- Freytag A , QuinzlerR , FreitagMet al. [Use and potential risks of over-the-counter analgesics] [Article in German] . Schmerz28 ( 2 ), 175 – 182 ( 2014 ).
- Paulose-Ram R , HirschR , DillonC , LosonczyK , CooperM , OstchegaY . Prescription and non-prescription analgesic use among the US adult population: results from the third National Health and Nutrition Examination Survey (NHANES III) . Pharmacoepidemiol. Drug Saf.12 ( 4 ), 315 – 326 ( 2003 ).
- Saragiotto BT , MachadoGC , FerreiraML , PinheiroMB , Abdel ShaheedC , MaherCG . Paracetamol for low back pain . Cochrane Database Syst. Rev. ( 6 ), CD012230 ( 2016 ).
- Blondell RD , AzadfardM , WisniewskiAM . Pharmacologic therapy for acute pain . Am. Fam. Physician.87 ( 11 ), 766 – 772 ( 2013 ).
- Moore RA , DerryS , AldingtonD , WiffenPJ . Adverse events associated with single dose oral analgesics for acute postoperative pain in adults – an overview of Cochrane reviews . Cochrane Database Syst. Rev. ( 10 ), CD011407 ( 2015 ).
- Moore RA , WiffenPJ , DerryS , MaguireT , RoyYM , TyrrellL . Non-prescription (OTC) oral analgesics for acute pain - an overview of Cochrane reviews . Cochrane Database Syst. Rev. ( 11 ), CD010794 ( 2015 ).
- Chou R , DeyoR , FriedlyJet al. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline . Ann. Intern. Med.166 ( 7 ), 493 – 505 ( 2017 ).
- Tick H , NielsenA , PelletierKRet al. Evidence-based nonpharmacologic strategies for comprehensive pain care: the Consortium Pain Task Force white paper . Explore (NY).14 ( 3 ), 177 – 211 ( 2018 ).
- Rice AS , SmithBH , BlythFM . Pain and the global burden of disease . Pain.157 ( 4 ), 791 – 796 ( 2016 ).
- Wirth B , EhrlerM , HumphreysBK . First episode of acute low back pain – an exploratory cluster analysis approach for early detection of unfavorable recovery . Disabil. Rehabil.39 ( 25 ), 2559 – 2565 ( 2017 ).
- Hoy D , MarchL , BrooksPet al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study . Ann. Rheum. Dis.73 ( 6 ), 968 – 974 ( 2014 ).
- Schiller JS , LucasJW , WardBW , PeregoyJA . Summary health statistics for U.S. adults: National Health Interview Survey, 2010 . Vital Health Stat. 10. ( 252 ), 1 – 207 ( 2012 ).
- Grandi G , FerrariS , XholliAet al. Prevalence of menstrual pain in young women: what is dysmenorrhea? J. Pain Res. 5 , 169 – 174 ( 2012 ).
- Ju H , JonesM , MishraG . The prevalence and risk factors of dysmenorrhea . Epidemiol. Rev.36 , 104 – 113 ( 2014 ).
- Paller CJ , CampbellCM , EdwardsRR , DobsAS . Sex-based differences in pain perception and treatment . Pain Med.10 ( 2 ), 289 – 299 ( 2009 ).
- Fillingim RB , KingCD , Ribeiro-DasilvaMC , Rahim-WilliamsB , RileyJL3rd . Sex, gender, and pain: a review of recent clinical and experimental findings . J. Pain10 ( 5 ), 447 – 485 ( 2009 ).
- Apfelbaum JL , ChenC , MehtaSS , GanTJ . Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged . Anesth. Analg.97 ( 2 ), 534 – 540 ( 2003 ).
- Buvanendran A , FialaJ , PatelKA , GoldenAD , MoricM , KroinJS . The incidence and severity of postoperative pain following inpatient surgery . Pain Med.16 ( 12 ), 2277 – 2283 ( 2015 ).
- Tanabe P , BuschmannM . A prospective study of ED pain management practices and the patient’s perspective . J. Emerg. Nurs.25 ( 3 ), 171 – 177 ( 1999 ).
- Johnston CC , GagnonAJ , FullertonL , CommonC , LadoresM , ForliniS . One-week survey of pain intensity on admission to and discharge from the emergency department: a pilot study . J. Emerg. Med.16 ( 3 ), 377 – 382 ( 1998 ).
- Todd KH , DucharmeJ , ChoiniereMet al. Pain in the emergency department: results of the Pain and Emergency Medicine Initiative (PEMI) multicenter study . J. Pain.8 ( 6 ), 460 – 466 ( 2007 ).
- Guru V , DubinskyI . The patient vs. caregiver perception of acute pain in the emergency department . J. Emerg. Med.18 ( 1 ), 7 – 12 ( 2000 ).
- Sari O , TemizC , GolcurMet al. Pain perception differences between patients and physicians: a pain severity study in patients with low back pain . Turk. Neurosurg.25 ( 3 ), 461 – 468 ( 2015 ).
- Marquié L , RaufasteE , LauqueD , MarinéC , EcoiffierM , SorumP . Pain rating by patients and physicians: evidence of systematic pain miscalibration . Pain.102 ( 3 ), 289 – 296 ( 2003 ).
- Fink R . Pain assessment: the cornerstone to optimal pain management . Proc. (Bayl. Univ. Med. Cent.).13 ( 3 ), 236 – 239 ( 2000 ).
- Daniels SE , GoulderMA , AspleyS , ReaderS . A randomised, five-parallel-group, placebo-controlled trial comparing the efficacy and tolerability of analgesic combinations including a novel single-tablet combination of ibuprofen/paracetamol for postoperative dental pain . Pain152 ( 3 ), 632 – 642 ( 2011 ).
- Chang AK , BijurPE , EssesD , BarnabyDP , BaerJ . Effect of a single dose of oral opioid and nonopioid analgesics on acute extremity pain in the emergency department: a randomized clinical trial . JAMA318 ( 17 ), 1661 – 1667 ( 2017 ).
