Abstract
Aim: To provide real-world evidence for the effectiveness and tolerability of lidocaine 700 mg medicated plaster (LMP) compared with oral systemic first-line medications (OSM) in postherpetic neuralgia treatment. Patients & methods: Retrospective cohort study in patients refractory to at least one recommended OSM (single drug or a combination of drugs) using anonymized routine medical care data from the German Pain e-Registry. A matched pair approach using propensity score matching was employed. Results: A total of 1711 data sets of postherpetic neuralgia patients were identified per treatment group. The majority (>60%) had experienced pain for more than a year and reported a high burden of pain and reduced quality of life. Six months of LMP treatment provided significantly greater pain reductions, improvements in pain-related impairments and quality of life than OSM treatment (p < 0.001 for all parameters). Drug-related adverse events and treatment discontinuation due to drug-related adverse events also occurred less frequently under LMP treatment (p < 0.001). Conclusion: These real-world data confirm the effectiveness and good tolerability of LMP under routine medical care. The treatment was significantly more effective when compared with first-line oral systemic medications.
Lay abstract
Postherpetic neuralgia is the most common complication of shingles. It is a chronic condition causing burning pain that persists long after the shingles rash disappears. There are several oral and topical medications available for pain treatment. Our study compared the effectiveness and tolerability of the topical lidocaine 700 mg medicated plaster with oral medications using anonymized patient data from German clinical practices collected in a pain registry (1711 patient data sets per treatment). Six months of treatment with the lidocaine plaster resulted in better pain relief, fewer restrictions in daily life activities, and better quality of life for the patients than the oral medications investigated. The lidocaine plaster was also significantly better tolerated. The lidocaine 700 mg medicated plaster is effective and well tolerated in routine medical practice.
Postherpetic neuralgia (PHN), a chronic peripheral neuropathic pain condition often characterized by localized debilitating pain, is the most common complication of herpes zoster. According to the new ICD-11 classification, chronic pain is defined as pain that persists or recurs for more than 3 months [Citation1]. PHN is among the most common conditions of chronic peripheral neuropathic pain that manifests mostly as spontaneous ongoing pain (e.g., aching, burning, throbbing pain), paroxysmal electric shock-like or lancinating pain, and/or stimulus-evoked sensations such as allodynia or hyperalgesia after the acute herpes zoster rash has healed [Citation2]. PHN reduces physical and social functioning, psychological well being and the quality of life of the patients [Citation3,Citation4], and also has a significant social impact on the patients’ family [Citation5]. The condition predominantly affects the elderly [Citation2], an age group already burdened by frequent comorbidities necessitating the intake of several medications and thus at an increased risk of drug–drug interactions, adverse effects and insufficient treatment compliance. The occurrence of herpes zoster and progression to PHN adds to this burden and causes a marked decline in the overall functional status of affected patients [Citation6]. In contrast to expectations created with the advent of herpes zoster vaccines, a recent large epidemiological study from 1994 to 2018 showed that the overall incidence rates of PHN continued to increase annually in the USA [Citation7].
Pharmacological treatment options for PHN treatment include oral systemic medications such as tricyclic antidepressants, the antiepileptics pregabalin and gabapentin, the selective serotonin–norepinephrine reuptake inhibitors duloxetine and venlafaxine, and opioids, as well as the topical treatments lidocaine 700 mg medicated plaster (LMP) and capsaicin 8% patch [Citation8,Citation9]. Systemic medications are often limited by side effects and might result in poor compliance or treatment discontinuation, whereas topical treatments applied directly at the site of the pain have very little systemic exposure and thus a limited liability for drug–drug interactions and adverse effects [Citation10].
There is increasing recognition that analyses of real-world data, in other words, “routinely collected data relating to a patient’s health status or the delivery of healthcare from a variety of sources other than traditional clinical trials” [Citation11] can support benefit/risk evaluations of a treatment [Citation11,Citation12], as they reflect realistic outcomes in patient populations that may be far more diverse than preselected trial populations. Main sources of real-world data include electronic health records, health insurance claims data bases, prescription data and patient registries [Citation11]. For LMP, analgesic efficacy and improvements in sleep and quality of life have been demonstrated in clinical trials [Citation13,Citation14,Citation15,Citation16,Citation17,Citation18,Citation19,Citation20,Citation21]. Lidocaine is continuously released at the plaster application site, with only approximately 3 ± 2% reaching systemic circulation [Citation22] thus making adverse reactions based on systemic lidocaine effects unlikely. The treatment has indeed shown good short- and long-term tolerability [Citation23]. To provide supporting real-world evidence for the use of LMP in PHN treatment, the present noninterventional retrospective cohort study analyzed real-world practice data from the German Pain e-Registry.
Patients & methods
This noninterventional retrospective cohort study compared the effectiveness and tolerability of LMP with oral systemic first-line treatments (recommended according to the current German guideline for the treatment of neuropathic pain [Citation24]) in PHN patients refractory to at least one recommended oral systemic first-line medication (single drug or a combination of drugs).
Description of the German Pain e-Registry
The analysis used anonymized data of the German Pain e-Registry, a national web-based pain treatment registry developed on behalf of the German Pain Association. The registry prospectively collects routine data of pain patients via the online documentation service iDocLive®. Data are entered predominantly by patients and serve to inform their pain physicians about demographic specifics, pain and pain-related issues such as impairments of daily activities and quality of life, response to new treatments and other information deemed necessary for individual patient care. At practice visits, these data are reviewed together with the patient and checked for completeness and validity. The patient questionnaires recommended by the German Pain Association, the German Pain Society, and the German Pain League for use on iDocLive® (and set to default) are two standard instruments for pain documentation, the German Pain Questionnaire and the German Pain Diary [Citation25]. They were developed to fulfill formal requirements for quality-assured and standardized documentation of all treatment-relevant data for the routine care of chronic pain patients in Germany. The questionnaires include a variety of validated instruments for the assessment of intensity, severity, phenomenology and chronification stage of pain, pain-related impairments of daily life, quality of life, well-being, depression, anxiety and stress and also collect data on pain treatment and treatment-related adverse events (AEs). According to standard operating procedures of the German Pain e-Registry, anonymized data made available for healthcare research are temporarily extracted from the database and deleted after completion of the analyses specified in the research project.
Data selection
There was no formal sample size calculation for this analysis. All data sets of patients with newly initiated treatment with one of the study medications before 31 December 2018 were selected from the database of the German Pain e-Registry as of 31 July 2019 according to defined inclusion and exclusion criteria. Eligible data were of adult outpatients with a pain history of at least 3 months and medically confirmed peripheral neuropathic pain classified as PHN and refractory to treatment with at least one first-line oral systemic medication for peripheral neuropathic pain (single drug or a combination of drugs such as gabapentin, pregabalin, amitriptyline or duloxetine). Exclusion criteria included a diagnosis of cancer and/or cancer-related pain, chemotherapy-induced neuropathic pain, any type of evidence for HIV and/or HIV-related neuropathy, and a diagnosis of low back pain, osteoarthritis, complex regional pain syndrome, myofascial pain, trigeminal autonomic cephalalgia, and any painful lesions of the cranial nerves not caused by peripheral neuropathic pain. Treatment initiation was defined as no study medication use in the 12 weeks prior to treatment; the date of first dose was set as the starting date for the 24-week assessment period.
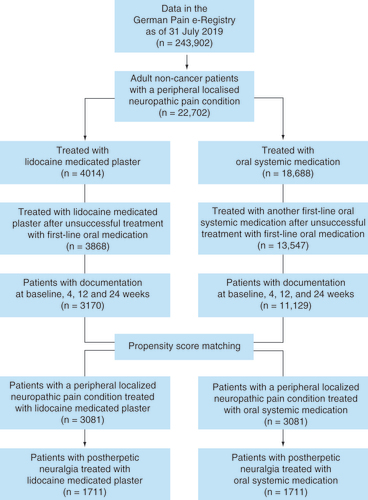
shows the data selection process. A matched pair approach using propensity score matching was chosen to obtain comparable study cohorts. This was carried out on eligible data including 3170 peripheral neuropathic pain patients with data sets receiving LMP and 11,129 peripheral neuropathic pain patients with data sets with oral systemic first-line treatment using the nearest neighbor method for the predefined confounding factors. These factors included age, sex, 24-h pain intensity index, pain severity [Citation26], chronification stage [Citation27], pain duration, comorbidities (ICD-10 code, first three digits), indications/diagnosis for treatment, previous medication (Anatomical Therapeutic Chemical code, first 3 digits and/or medication group) and reason for switching (effectiveness, tolerability, drug-related AEs). In total, 1711 pairs of data sets from patients with a diagnosis of PHN could be included in the analysis.
Study & concomitant analgesic medication
Study medications were LMP and recommended first-line oral systemic medications (OSM). All treatment decisions (e.g., selection of medication, initial dosing, dose adjustments) were at the discretion of the treating physician and were based on the individual patient needs, but might not always have been in accordance with product information recommendations for PHN treatment. The administration of concomitant analgesic medications was also solely based on individual patient needs.
Outcome measures
Treatment effectiveness was determined using patient-reported information on pain intensity, pain-related impairments in daily activities and quality of life, overall quality of life and global impression of change. Pain intensity was rated on a 100 mm visual analogue scale (VAS) with 0 = no pain to 100 = worst imaginable pain. A pain intensity index (PIX) was calculated as the arithmetic mean of the lowest, average, and highest 24-h pain intensities. Pain-related disabilities in daily activities related to ‘home and family’, ‘recreation’, ‘social activities’, ‘occupation’, ‘self-care/personal maintenance’, ‘sleep’ and ‘overall quality of life’ were reported using a modified version of the pain disability index [Citation28] (mPDI) on a 100 mm VAS (0 = none to 100 = worst imaginable). Pain-related quality of life was measured by the quality of life impairment by pain inventory questionnaire (QLIP). This instrument rates well-being, sleep, pain, impairments, and mood with a sum score ranging from 0 to 40 points. A sum score of ≤20 points indicates severe impairment. Overall quality of life was assessed with the eight physical and mental domains of the Short Form 12 questionnaire [Citation29] and summarized in a physical and a mental component score. The average scores for the German population norm are 49.6 for the physical component score and 52.3 for the mental component score [Citation30]. Patients also reported their change in health status using the Patient Global Impression of Change scale ranging from 1 = very much improved to 7 = very much worse [Citation31].
Tolerability assessments were based on the occurrence of drug-related adverse events (DRAEs) and treatment discontinuation due to DRAEs. A DRAE was defined as an AE assessed as possibly, probably, or definitely related to the studied medication by the treating physician.
Statistical analysis
All analyses were conducted using PASW Statistics version 18. AEs were encoded using the Medical Dictionary for Regulatory Activities (MedDRA version 22.0, 2019). The analysis set comprised the data of patients who received at least one dose of the relevant treatment under assessment and for whom at least one postbaseline measure had been recorded. For the primary effectiveness end point, missing data were imputed using the baseline observation carried forward approach for data sets from patients who discontinued treatment (due to an AE, death or lack of effectiveness). Otherwise, the last observation carried forward method was used for the primary and all secondary variables.
The primary effectiveness end point was the absolute change in the average PIX from baseline following 4, 12 and 24 weeks of treatment. Secondary effectiveness end points were the change from baseline after 4, 12 and 24 treatment weeks in average 24-h PIX (relative change), in highest 24-h pain intensity, in pain-related disabilities in daily life, in quality of life impairment by pain, and in overall quality of life, response to treatment (defined as ≥30 and ≥50% reduction in PIX), patients’ global impression of change in health status, patients with DRAEs, reasons for premature discontinuation, discontinuation of treatment due to DRAEs, and change in concomitant medications during the observation period. A mixed-model repeated measures covariance analysis (adjusted for potential confounding factors such as age, gender, pain severity [von Korff scale], stage of chronification, history/duration of pain, comorbidity, comedication and prior and current medication at baseline as well as baseline value) was the analytical technique for the primary effectiveness measure. The difference in least squares mean between treatments (LMP minus OSM) after 1, 3 and 6 months of treatment along with their 2-sided 95% CI was calculated for the analysis set based on the model, and its effect size was determined with Cohen’s d. Fisher’s exact test and Pearson’s chi-square test were used for comparisons of secondary end points between the groups using a two-sided significance level of 0.05. All secondary analyses were classified as exploratory and not adjusted for multiplicity.
Results
Patients
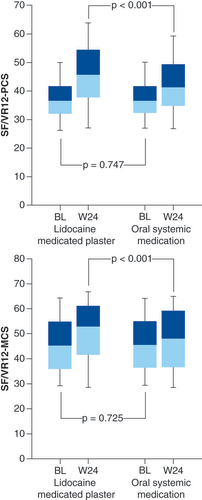
Propensity score matching resulted in the selection of 3081 patients with peripheral neuropathic pain including 1711 PHN patients with comparable baseline data in each treatment group () for the analysis. The majority (66%) was female, nearly half were >60 years old (LMP patients 47.1%, OSM patients 47.7%), and almost all (>94%) suffered from comorbidities and received concomitant medications. More than 60% of patients documented a pain duration of more than a year. Despite the administration of on average more than seven previous analgesic medications, pain intensity at baseline was high and was accompanied by considerable impairments in daily activities (). Overall quality of life, in particular in the physical domain, was markedly affected ().
Table 1. Baseline characteristics before and after propensity score matching.
Table 2. Effectiveness assessment parameters at baseline and end of observation.
Analgesic treatment
LMP patients received a mean 1.8 ± 0.9 patches/day (range 1–4) with a mean treatment duration of 145 ± 46.3 days (95% CI 142.8–147.2). Premature discontinuation of the study medication was documented for 26.6% of the patients. The main reason was ‘pain treatment no longer required’ (15.7% of patients) followed by ‘due to DRAEs’ (4.8%), ‘lack of efficacy’ (3.9%) and ‘unclear information’ (2.2%).
Patients in the OSM group received tricyclic antidepressants (32.3%), selective serotonin–norepinephrine reuptake inhibitors (32.3%) or antiepileptic medication (35.5%). provides an overview of medications and doses used. Main medications were pregabalin (29.3%), duloxetine (24.7%) and amitriptyline (15.4%). Mean treatment duration was 102.9 ± 66.7 days (95% CI: 99.8–106.1). A total of 53.8% of OSM patients discontinued treatment prematurely, mainly due to DRAEs (33.1%) followed by ‘lack of efficacy’ (11.5%), ‘pain treatment no longer required’ (6.4%) and ‘unclear information’ (2.8%).
Table 3. Oral systemic recommended first-line medications documented for postherpetic neuralgia treatment in the oral systemic first-line medication group after switch from previous medication (n = 1711).
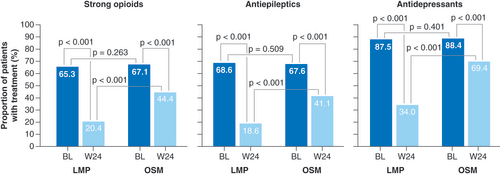
At baseline, all patients in both treatment groups received concomitant analgesic medications and most (64.6%) took up to two concomitant treatments for peripheral neuropathic pain. The types of concomitant analgesic medications used were well balanced between the groups. After 24 weeks of treatment with the study medication, a reduction was observed in significantly more LMP patients than OSM patients (94.1 vs 70.9%; p < 0.001). shows changes in concomitant analgesic medications (taken by >60% of patients at baseline) over the observation period.
Strong opioids included morphine, hydromorphone, oxycodone ± naloxone, fentanyl, buprenorphine, tapentadol and others.
BL: Baseline; LMP: Lidocaine 700 mg medicated plaster; OSM: Oral systemic medication; W: Week.
Pain intensity
Pain intensity was reduced in both treatment groups over the observation period, but to a greater extent in LMP patients (). Reductions in the primary effectiveness end point, the absolute change in the average PIX from baseline, were significantly greater for LMP than OSM patients at the three timepoints 4, 12 and 24 weeks of treatment (A) with a strong effect size (Cohen’s d >1.0 at all timepoints). The least squares mean absolute difference over all evaluation timepoints was -13.0 ± 14.5 (95% CI -13.8 to -12.3) mm VAS (p < 0.001), and the corresponding effect size was 1.1 (95% CI 1.1–1.2; ). After 24 weeks the relative mean change from baseline in PIX was 52.5% for LMP patients and 29.4% for OSM patients (p < 0.001, Cohen’s d = 0.878).
(A) Change from baseline over the observation period. Boxplots show median (middle horizontal line in the box), 25 and 75% quartiles (bottom and top lines of the box), and five and 95% percentiles (whiskers). Improvement is shown by reductions in pain intensity index and modified pain disability index, and by increases in quality of life impairment by pain. (B) Improvement versus baseline in pain intensity index at end of observation.
LMP: Lidocaine 700 mg medicated plaster; NRS: Numerical rating scale; OSM: Oral systemic medication; PIX: Pain intensity index; VAS: Visual analogue scale.
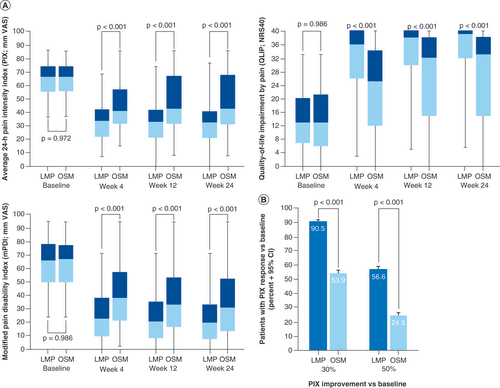
Table 4. Absolute change versus baseline in pain intensity index (primary effectiveness end point).
Response to treatment after 24 weeks (defined as ≥30 and ≥50% reduction in PIX) was also significantly better in the LMP than in the OSM group (B).
Pain-related impairments & quality of life
At baseline, patients reported considerable impairments in daily life activities (), which improved under both treatments over the observation period (A). Improvements (i.e., reductions in mPDI) were significantly greater in the LMP group (p < 0.001).
There were marked pain-related impairments of quality of life at baseline: 75.5% of LMP patients and 72.8% of OSM patients were severely affected with a QLIP sum score of ≤20 (). The QLIP improved in both treatment groups but with a significant treatment difference in favor of LMP (p < 0.001; A). At week 24, 10.8% of LMP and 30.3% of OSM patients were still severely affected ().
Change in health status & overall quality of life
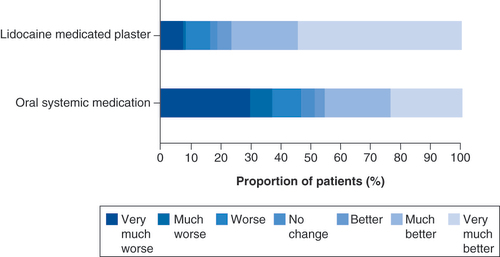
shows the patients’ impression of change after 24 weeks of treatment with the study medication. Significantly more LMP patients than OSM patients (76.5 vs 45.7%, p < 0.001) reported improvements of ‘much better’ and ‘very much better’.
p < 0.001 in favor of lidocaine 700 mg medicated plaster.
Overall quality of life was markedly affected at baseline (). The physical component score had improved to a greater extent in the LMP than the OMS group at 24 weeks (p < 0.001; ) with relative increases from baseline of 13.3 and 7.4%, respectively. Changes in the mental component score were only slight but still significantly different between the groups ().
Boxplots show median (middle horizontal line in the box), 25 and 75% quartiles (bottom and top lines of the box), and five and 95% percentiles (whiskers).
BL: Baseline; MCS: Mental component score; PCS: Physical component score; W: Week.
Tolerability
The proportion of patients with DRAEs was significantly lower under LMP treatment (8.9 vs 58.1% for OSM patients; p < 0.001; ). LMP patients mainly reported application site reactions and other skin-related reactions (). In the OSM group, 24.2% of patients had nervous system disorders, 23.2% psychiatric disorders and 17.1% gastrointestinal disorders (). The most common DRAE was somnolence (15.8% of patients) followed by dizziness, nausea and hyperhidrosis (all 5.1%).
DRAE: Drug-related adverse event; LMP: Lidocaine 700 mg medicated plaster; OSM: Oral systemic medication.
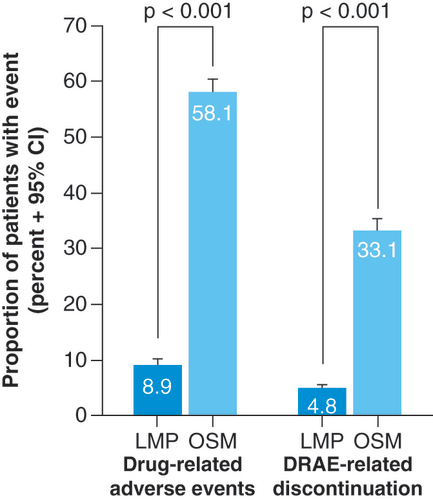
Table 5. All drug-related adverse events documented in patients receiving lidocaine 700 mg medicated plaster during the observation period (n = 1711).
Table 6. Main drug-related adverse events documented in patients receiving oral systemic first-line medication during the observation period (n = 1711).
A significantly smaller proportion of patients in the LMP group discontinued treatment due to DRAEs (4.8 vs 33.1% for OSM patients; p < 0.001; ).
Discussion
The routine clinical practice data presented here show that treatment with LMP provided effective pain treatment over 24 weeks for PHN patients unsuccessfully treated with recommended first-line oral systemic medications. This result is consistent with the known mode of action of LMP that delivers lidocaine to the dermis and provides mechanical protection of the skin [Citation32,Citation33]. Lidocaine is a voltage-gated sodium channel inhibitor capable of blocking abnormally functioning (sensitized) Nav1.7 and Nav1.8 sodium channels in nociceptors of A delta and C fibres of the dermis, has an inhibitory effect on inflammatory processes through the regulation of T cell activity and the suppression of the production of nitric oxide and may directly activate the transient receptor potential channels TRPV1 and TRPA1 expressed in nociceptive sensory neurons, reducing the electrical activity in TRP-containing nerves and consequently inducing analgesia by membrane depolarization [Citation10,Citation33,Citation34,Citation35]. Pain relief was accompanied by significant improvements in daily living activities and led to a better general health status and improved overall quality of life of the patients. Moreover, when these outcomes were compared with matched pairs of patients treated with alternative oral treatments (after a first-line treatment failed), LMP was significantly more effective. A previous network meta-analysis of randomized controlled trials suggested similar levels of pain relief for LMP and gabapentin, but a higher effectiveness for LMP compared with pregabalin or high-dose capsaicin in the treatment of PHN [Citation36]. The patient-reported outcomes reported here indicate a better treatment response to LMP than to oral systemic medications in the routine daily care of chronic PHN patients.
As expected for a topical treatment with low systemic exposure, AEs related to LMP treatment were mainly associated with the application of the plaster and other skin-related tolerability issues and did not include systemic side effects. In contrast to oral systemic medications, the plaster was well tolerated with an overall low incidence of drug reactions and a premature treatment discontinuation rate below 5%. The findings support the previously reported good short- and long-term tolerability of the plaster [Citation23] and the generally better AEs profile of LMP compared with pregabalin in a recent network meta-analysis [Citation37]. A better safety profile compared with pregabalin, gabapentin, amitriptyline and duloxetine was also documented by European general practice data for neuropathic pain treatment [Citation38].
Restoring or preserving patients’ independence and quality of life is an important goal of pain management. PHN has a substantial impact on quality of life affecting physical, social, functional and mental health of the patients [Citation3]; the elderly are particularly affected [Citation39]. Physical function impairments such as fatigue, loss of appetite, weight loss, reduced mobility, physical inactivity and insomnia may lead to difficulties with even basic tasks of daily living and to a loss of independence, social withdrawal and isolation [Citation3]. The previously noted marked improvements in quality of life under LMP treatment [Citation21,Citation40] were confirmed in this real-world data analysis. Considerable improvements were observed in particular for the outcome measure pain-related quality of life which were significantly greater than improvements under OSM treatment.
Of note is that concomitant analgesic medications could be reduced over time and more so with LMP compared with oral treatments. This is of particular importance as a decline in concomitant systemic pain treatments reduces the burden of therapy, the risk of AEs and potential drug–drug interactions with medications used for other comorbidities. Moreover, the reduced intake of concomitant analgesic medications in the LMP group suggests that the efficacy outcomes with LMP are not confounded by increasing use of concomitant analgesic medications.
Overall, LMP proved effective and well tolerated as an alternative treatment option for PHN patients under routine medical care who did not respond to first-line treatment with systemic medications.
Although randomized controlled trials are the best available standard of evidence of treatment efficacy [Citation11], this trial design has narrowly defined trial criteria and thus very specific trial populations. Observational data can provide a more heterogenous study population and can therefore complement clinical trial results. An electronic data registry represents a broad spectrum of patients under routine medical care with a focus on patient-relevant outcomes established to improve patient care. In contrast to clinical trials which are usually restricted to a few months, a large database of long-term data might be available. Analyses using registry data face the limitations inherent to all observational retrospective studies, but the validity of the results can be strengthened by employing a good methodological standard. A study protocol and a statistical analysis plan were established for the present study prior to data extraction from the registry. Physicians made treatment decisions during routine clinical care and selection bias for one or the other treatment might thus have occurred based on patient characteristics, familiarity with available treatments, etc. As all tested treatments have been well established and healthcare professionals well familiar with the treatment of pain are making use of the registry, the latter likely plays a minor role. However, to avoid bias based on patient characteristics that are thought to influence treatment, a matched pair approach with propensity score matching was used, which generated a large study population of 3081 patients with peripheral neuropathic pain including 1711 data sets of patients with PHN per treatment group.
Conclusion
The analysis of real-world data from PHN patients extracted from the German Pain e-Registry confirmed the effectiveness and good tolerability of the lidocaine 700 mg medicated plaster under routine medical care. Moreover, when compared with first-line oral systemic medications, LMP treatment was significantly more effective in reducing pain intensity and in improving quality of life with a significantly better tolerability profile.
Postherpetic neuralgia (PHN), a chronic peripheral neuropathic pain condition often characterized by localized debilitating pain, is a common complication of herpes zoster. It predominantly affects the elderly.
Clinical trials have shown the good efficacy and excellent safety profile of the lidocaine 700 mg medicated plaster (LMP) in PHN treatment.
In order to provide real-world evidence for the use of LMP in PHN treatment, real-world practice data were extracted from the German Pain e-Registry and analyzed in a noninterventional retrospective cohort study.
The study compared the effectiveness and tolerability of LMP and first-line oral systemic medications (OSM) over a 6-month period in PHN patients refractory to at least one OSM treatment. Propensity score matching provided 3081 data sets of patients with peripheral neuropathic pain patients including 1711 PHN patients per treatment group.
More than 60% of patients had experienced pain for more than a year and reported a high burden of pain and reduced quality of life.
Six months of LMP treatment provided significantly greater pain reductions and improvements in pain-related impairments of daily living and quality of life than OSM treatment (p < 0.001 for all parameters).
The proportion of patients with drug-related adverse events was significantly lower under LMP treatment (8.9 vs 58.1% for OSM patients; p < 0.001) and consisted mainly of application site reactions. The treatment discontinuation rate due to drug-related adverse events was also significantly lower (4.8 vs 33.1% for OSM patients; p < 0.001).
In routine daily care, chronic PHN patients unsuccessfully treated with recommended first-line oral systemic medications had a significantly better response to newly initiated LMP treatment with a significantly better tolerability profile when compared with OSM treatment.
Author contributions
MA Überall, I Bösl, I Sabatschus, E Hollanders and M Eerdekens contributed in conception and design. MA Überall contributed in data extraction and data analysis. MA Überall, I Bösl, I Sabatschus, E Hollanders, M Eerdekens contributed in data interpretation. All authors critically revised for important intellectual content, approved the final manuscript version and agreed to the submission.
Ethical conduct of research
The study is registered in the European Union electronic Registry of Post-Authorization Studies (EUPAS 32826) through the European Network of Centers for Pharmacoepidemiology and Pharmacovigilance® coordinated by the European Medicines Agency and was conducted in accordance with the Declaration of Helsinki and relevant national and regulatory requirements; approval was granted by the independent ethics committee of the German Pain Association. All patients provided written informed consent prior to participation in the registry. All analyses were carried out using only anonymized data to comply with German guidelines on protection of data privacy and with the European Union General Data Protection Regulation.
Acknowledgments
The authors thank GHH Müller-Schwefe for his critical assessment and interpretation of the data.
Financial & competing interests disclosures
MA Überall is a physician, pain specialist, medical director of the Institute of Neurological Sciences, and CEO of O Meany-MDPM GmbH, which was responsible for data extraction and biometrical analyses. Data extraction and biometrical analyses have been paid for by Grünenthal GmbH, Germany. MA Überall received financial support and/or expenses in form of research money, consultancy fees and/or remunerations for lecture activities from: Allergan, Almirall, Amicus Therapeutics, Aristo Pharma, Bionorica, Glaxo Smith Kline, Grünenthal, Hapa Medical, Hexal, IMC, Kyowa-Kirin, Labatec, Mucos, Mundipharma, Nestle, Pfizer, Recordati, Servier, SGP-Pharma, Shionoghi, Spectrum Therapeutics, Teva, and Tilray. M Eerdekens, I Bösl, E Hollanders, and I Sabatschus are employees of Grünenthal GmbH, Germany. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Writing and editorial assistance was provided by E Grosselindemann and B Brett and was paid for by Grünenthal GmbH, Germany.
Additional information
Funding
References
- Scholz J , FinnerupNB , AttalNet al. The IASP classification of chronic pain for ICD-11: chronic neuropathic pain. Pain160, 53–59 (2019).
- Johnson RW , RiceASC. Postherpetic neuralgia. N. Engl. J. Med.371, 1526–1537 (2014).
- Johnson RW , BouhassiraD , KassianosG , LeplègeA , SchmaderKE , WeinkeT. The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med.8, 37 (2010).
- Curran D , Schmidt-OttR , SchutterU , SimonJ , AnastassopoulouA. Impact of herpes zoster and postherpetic neuralgia on the quality of life of Germans aged 50 or above. BMC Infect. Dis.18, 496 (2018).
- Weinke T , GloggerA , BertrandI , LukasK. The societal impact of herpes zoster and postherpetic neuralgia on patients, life partners, and children of patients in Germany. Sci World J. article ID 749698 (2014).
- Pickering G , GavazziG , GaillatJ , PaccalinM , BlochK , BouhassiraD. Is herpes zoster an additional complication in old age alongside comorbidity and multiple medications? Results of the post hoc analysis of the 12-month longitudinal prospective observational ARIZONA cohort study. BMJ Open6, e009689 (2016).
- Thompson RR , KongCL , PorcoT , KimE , EbertCD , AcharyaNR. Herpes zoster and postherpetic neuralgia: changing incidence rates from 1994 to 2018 in the United States. Clin. Infect. Dis. doi:10.1093/cid/ciaa1185 (2020) ( Epub ahead of print).
- Attal N , CruccuG , BaronRet al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur. J. Neurol.17, 1113–e88 (2010).
- Finnerup NB , AttalN , HaroutounianSet al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol.14, 162–173 (2015).
- Baron R , AllegriM , Correa-IllanesGet al. The 5% lidocaine-medicated plaster: its inclusion in international treatment guidelines for treating localized neuropathic pain, and clinical evidence supporting its use. Pain Ther.5, 149–169 (2016).
- Cave A , KurzX , ArlettP. Real-world data for regulatory decision making: challenges and possible solutions for Europe. Clin. Pharm. Ther.106, 36–39 (2019).
- Bolislis WR , FayM , KühlerTC. Use of real-world data for new drug applications and line extensions. Clin. Ther.42, 926–938 (2020).
- Rowbotham MC , DaviesPS , VerkempinckCet al. Lidocaine patch: double-blind controlled study of a new treatment method for post-herpetic neuralgia. Pain65, 39–44 (1996).
- Galer BS , RowbothamMC , PeranderJet al. Topical lidocaine patch relieves postherpetic neuralgia more effectively than a vehicle topical patch: results of an enriched enrollment study. Pain80, 533–538 (1999).
- Baron R , MayoralV , LeijonG , BinderA , SteigerwaldI , SerpellM. 5% lidocaine medicated plaster versus pregabalin in post-herpetic neuralgia and diabetic polyneuropathy: an open-label, non-inferiority two-stage RCT study. Curr. Med. Res. Opin.25, 1663–1676 (2009).
- Binder A , BruxelleJ , RogersP , HansG , BöslI , BaronR. Topical 5% lidocaine (lignocaine) medicated plaster treatment for post-herpetic neuralgia. Results of a double-blind, placebo-controlled, multinational efficacy and safety trial. Clin. Drug Investig.29, 393–408 (2009).
- Rehm S , BinderA , BaronR. Post-herpetic neuralgia: 5% lidocaine medicated plaster, pregabalin, or a combination of both? A randomized, open, clinical effectiveness study. Curr. Med. Res. Opin.26, 1607–1619 (2010).
- Hans G , SabatowskiR , BinderAet al. Efficacy and tolerability of a 5% lidocaine medicated plaster for the topical treatment of post-herpetic neuralgia: results of a long-term study. Curr. Med. Res. Opin.25, 1295–1305 (2009).
- Sabatowski R , HansG , TackenI , KapanadzeS , BuchheisterB , BaronR. Safety and efficacy outcomes of long-term treatment up to 4 years with 5% lidocaine medicated plaster in patients with post-herpetic neuralgia. Curr. Med. Res. Opin.28, 1337–1346 (2012).
- Sabatowski R , BöslI , KönigS , BuchheisterB , MeierT , BaronR. Treatment of postherpetic neuralgia with 5% lidocaine medicated plaster in elderly patients – subgroup analyses from three European clinical trials. Curr. Med. Res. Opin.33, 595–603 (2017).
- Binder A , RogersP , HansG , BaronR. Impact of topical 5% lidocaine-medicated plasters on sleep and quality of life in patients with postherpetic neuralgia. Pain Manag.6, 229–239 (2016).
- Campbell BJ , RowbothamM , DaviesPS , JacobPIII , BenowitzNL. Systemic absorption of topical lidocaine in normal volunteers, patients with post-herpetic neuralgia, and patients with acute herpes zoster. J. Pharm. Sci.91, 1343–1350 (2002).
- Navez ML , MonellaC , BöslI , SommerD , DelormeC. 5% lidocaine medicated plaster for the treatment of postherpetic neuralgia: a review of the clinical safety and tolerability. Pain Ther.4, 1–15 (2015).
- Schlereth T et al. Diagnosis and noninterventional treatment of neuropathic pain, S2k guideline (in German). In: Guidelines for Diagnosis and Treatment in Neurology.German Society of Neurology (2019). https://www.awmf.org/uploads/tx_szleitlinien/030-114l_S2k_Diagnose-nicht-interventionelle-Therapie-neuropathischer-Schmerzen_2020-04_1.pdf
- German Pain Society . Manual for the German Pain Questionnaire (in German). https://www.schmerzgesellschaft.de/fileadmin/pdf/DSF_Handbuch_2020.pdf
- von Korff M , OrmelJ , KeefeFJ , DworkinSF. Grading the severity of chronic pain. Pain50, 133–149 (1992).
- Schmitt N , GerbershagenHU. The Mainz Staging System (MPSS) for chronic pain. Pain41(Suppl. 5), S484 (1990).
- Tait RC , ChibnallJT , KrauseS. The pain disability index: psychometric properties. Pain40, 171–182 (1990).
- Ware J Jr , KosinskiM , KellerSD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med. Care34, 220–233 (1996).
- Gandek B , WareJE , AaronsonNKet al. Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: results from the IQOLA project. J. Clin. Epidemiol.51, 1171–1178 (1998).
- Guy W . ECDEU Assessment Manual for Psychopharmacology (DHEW Publication no. ADM 76–338).US Government Printing Office, DC, USA (1976).
- Lin PL , FanSZ , HuangCHet al. Analgesic effect of lidocaine patch 5% in the treatment of acute herpes zoster: a double-blind and vehicle-controlled study. Reg. Anesth. Pain Med.33, 320–325 (2008).
- Garnock-Jones KP , KeatingGM. Lidocaine 5% medicated plaster. A review of its use in postherpetic neuralgia. Drugs69, 2149–2165 (2009).
- de León-Casasola OA , MayoralV. The topical 5% lidocaine medicated plaster in localized neuropathic pain: a reappraisal of the clinical evidence. J. Pain Res.9, 67–79 (2016).
- Sheets PL , JareckiBW , CumminsTR. Lidocaine reduces the transition to slow inactivation in NaV1.7 voltage-gated sodium channels. Br. J. Pharmacol.164, 719–730 (2011).
- Wolff RF , BalaMM , WestwoodM , KesselsAG , KleijnenJ. 5% lidocaine-medicated plaster vs other relevant interventions and placebo for post-herpetic neuralgia (PHN): a systematic review. Acta Neurol. Scand.123, 295–309 (2011).
- Buksnys T , ArmstrongN , WorthyGet al. Systematic review and network meta-analysis of the efficacy and safety of lidocaine 700 mg medicated plaster vs. pregabalin. Curr. Med. Res. Opin.36, 101–115 (2020).
- Katz P , PegoraroV , LiedgensH. Characteristics, resource utilization and safety profile of patients prescribed with neuropathic pain treatments: a real-world evidence study on general practices in Europe - the role of the lidocaine 5% medicated plaster. Curr. Med. Res. Opin.33(8), 1481–1489 (2017).
- Pickering G , LeplegeA. Herpes zoster pain, postherpetic neuralgia, and quality of life in the elderly. Pain Pract.11, 397–402 (2011).
- Überall MA , Müller-SchwefeGHH. Patient perceptions associated with the 5% lidocaine medicated plaster in daily practice. Curr. Med. Res. Opin.28, 901–909 (2012).