Abstract
Aim: This study evaluated use of liposomal bupivacaine (LB) versus standard bupivacaine (SB) alone in quadratus lumborum (QL) blocks for laparoscopic colorectal surgery. Materials & methods: In this prospective, randomized controlled trial, patients received QL1 blocks with either LB (40 ml 0.125% SB plus 20 ml of LB) or SB (60 ml of 0.25% SB) with 30 ml per side. Opioid usage, pain scores, side effects and other medications were recorded. Results: For 78 patients (38 LB; 40 SB), all parameters were similar between groups, except that the LB group had a higher 48 h need for metoclopramide. Conclusion: LB provided no analgesic benefit over SB alone for QL blocks.
Clinical Trials registration number: NCT03702621
Lay abstract
This study evaluated use of extended release bupivacaine (LB) versus standard bupivacaine (SB) alone in nerve blocks for laparoscopic colorectal surgery. Patients undergoing colorectal surgery received nerve blocks with either LB combined with SB, or SB alone. Opioid usage, pain scores, side effects and other medications were recorded. For 78 patients (38 LB + SB; 40 SB), all parameters were similar between groups, except that the LB group had a higher 48 h need for anti-nausea medication. LB provided no pain control benefit over SB alone for nerve blocks in colorectal surgery.
Thousands of laparoscopic colorectal surgeries are performed every year, and this surgery is often complicated by postoperative pain. In the attempt to reduce the use of opioid analgesics, many institutions have implemented enhanced recovery after surgery (ERAS) protocols including peripheral nerve blocks, neuraxial analgesia and new formulations of anesthetics. These pathways seek to improve pain control after surgery with goals of increased patient satisfaction and reduced postoperative complications [Citation1,Citation2]. One regional block that may be used for colorectal surgery is the quadratus lumborum (QL) block, targeting the T7–T12 branches of thoracolumbar nerves, with more recent studies suggesting coverage from T7-L2 depending on technique [Citation3–6].
Liposomal bupivacaine (LB) is a novel anesthetic that has shown promise when added to blocks [Citation4] for theoretically longer-lasting analgesia when compared with standard bupivacaine HCl alone (SB). The LB product contains bupivacaine encapsulated in multivesicular liposomes, with the local anesthetic released over time. It may be used in conjunction with SB to ensure that the patient experiences the immediate analgesic benefits of SB. The manufacturer indicates that LB may be administered in the same syringe as SB, as long as the ratio of milligram dose of SB to LB is not greater than 1:2 [Citation5]. The analgesic effects of LB may last for up to 72 h postoperatively, and it has been suggested to reduce postoperative opioid use [Citation6].
Many of the studies assessing the efficacy of LB versus SB come from studies in orthopedic surgery settings (especially joint replacements) and show varying results in pain control up to 72 h [Citation7,Citation8]. Several meta-analyses have examined the efficacy of LB, with varying conclusions ranging from excellent analgesia to no difference compared with other non-liposomal anesthetics [Citation9–15]. For colorectal surgeries specifically, postoperative opioid use was similar with LB or SB [Citation10]. Raman et al. performed a meta-analysis evaluating LB in both laparoscopic and open colectomies and found that LB was associated with decreased pain scores and lower opioid use. However, those authors questioned the reliability of results given the paucity of colorectal studies of LB [Citation11].
The aim of this study was to evaluate the clinical value of LB in postoperative pain control following colorectal surgery. We directly compared equal volumes of (1) LB + SB and (2) SB alone in QL blocks for laparoscopic colorectal surgery in the setting of ERAS with primary end points of pain scores, opioid usage, nausea and sedation scores and patient satisfaction.
Materials & methods
Study design & approvals
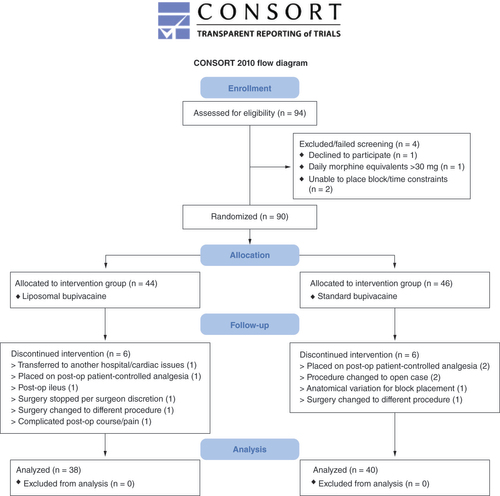
The study was a prospective double-blinded randomized controlled trial performed from 2018 through 2020. The study was reviewed and approved by the authors’ Institutional Review Board. This clinical trial was registered at ClinicalTrials.gov (https://clinicaltrials.gov/ct2/show/NCT03702621; registration number NCT03702621; date of registration 6 August 2018; patient enrollment date 19 September 2018). Patients provided written informed consent. Patient demographic information was collected including age, sex and body mass index (BMI). Opioid usage, visual analog pain scores and opioid side effects were monitored for 72 h after surgery. The study protocol is summarized in the Consolidated Standards of Reporting Trials (CONSORT) flow diagram ().
Patient population
Patients undergoing laparoscopic colorectal surgery at Indiana University Health, University Hospital were approached pre-operatively about their desire for regional analgesia after the surgery. Risks, benefits and alternatives were discussed with each prospective subject. Those patients expressing interest in regional pain control were freely offered the opportunity to participate in the study. Inclusion criteria were: patients undergoing colorectal surgery at Indiana University Hospital, American Society of Anesthesiologists (ASA) physical status classification 1–4, age of 18 years or older, male or female, desiring regional analgesia for postoperative pain control. Exclusion criteria were: any contraindication to the QL block; history of substance abuse in the past 6 months; opioid tolerance (defined as patient taking >30 mg of morphine equivalents daily); any physical, mental or medical conditions which might confound quantifying postoperative pain after surgery; known allergies to study medications (acetaminophen, gabapentin, bupivacaine, ketamine, lidocaine or dexamethasone); postoperative intubation; and BMI >40.0. Patients were randomly assigned to a study group (SB or LB) by a computer program (Research Randomizer; https://www.randomizer.org). Both the research team and the patient were blinded to the group assignment.
QL block procedure
All QL blocks were performed by anesthesiology residents (under direct supervision by an experienced attending anesthesiologist from the Acute Pain Service) after induction of general anesthesia. A total volume of 60 ml of local anesthetic solution was used for the block in both study groups. Patients in the LB group received a mixture of 40 ml 0.125% SB plus 20 ml of LB, with 30 ml injected on each side. Patient in the SB group received 60 ml of 0.25% SB, with 30 ml injected on each side. All blocks were QL1 blocks performed with ultrasound guidance with the patient in a supine position. A linear transducer was placed in the axial plane in the midaxillary line and moved posteriorly until the posterior aponeurosis of the transversus abdominis muscle became visible. The block target was the fascial plane between the end of the transversus abdominus aponeurosis and the lateral margin of the QL muscle. Fascial unzipping with injection was observed and 30 ml of injectate was delivered on each side.
ERAS protocol
All patients were enrolled in the same ERAS protocol regardless of the study group. They received pre-operative acetaminophen (1 g) and gabapentin (600 mg, reduced to 300 mg for patients >70 years). All patients received intraoperative lidocaine and ketamine infusions and at least 4 mg of intravenous dexamethasone prior to emergence from general anesthesia.
Scheduled postoperative oral gabapentin (300 mg daily) and acetaminophen (1 g, three-times daily) were administered per the hospital ERAS protocol. For severe breakthrough pain (visual analog scale score >7), intravenous hydromorphone was used as needed and switched to oral oxycodone once the patient was tolerating a regular diet.
Patients received anti-emetic medications at the discretion of the postoperative nurses. The ERAS protocol stated that ondansetron was to be used as the first line of therapy, followed by metoclopramide for continued nausea/vomiting.
Monitoring
All data were collected by study coordinators who were blinded to the study group allocation. Opioid usage was recorded daily. Pain scores were also measured at rest or with movement (ambulation) using the visual analog scale from 0 to 10 (0 = no pain, 10 = worst pain imaginable). Opioid side effects including nausea, sedation, ileus, urinary retention and respiratory depression were monitored and recorded. The requirement for other drugs (haloperidol, promethazine, ondansetron, metoclopramide or other) was recorded. All parameters were monitored at 1, 12, 24, 36, 48, 60 and 72 h after the QL block. Patients were encouraged to ambulate and were placed on an oral diet with advancement as tolerated. Discharge criteria included adequate pain control, tolerance of oral diet and passing of first flatus. Average day of discharge was postoperative day 3.
Statistical analysis
Analysis was performed using SAS 9.4 software (SAS Institute Inc). Demographic and post-surgical data were compared using a Wilcoxon rank sum test for continuous variables and Fisher’s exact test for categorical variables. Either median, 25th percentiles and 75th percentiles, or % counts were also established for each group and individual categories. Differences between groups were measured using a p-value, with significance being less than 5%.
Outcome variables of pain with rest or with movement, opioid usage and other drug usage were measured at 1, 24, 48 and 72 h postoperatively. Pain scores were compared using a using a mixed effect model repeat measurement (MMRM). These models included fixed effects for type of anesthesia, time and type of anesthesia by time interaction along with a random intercept effect. Differences between the two types of anesthesia at each time point were computed via LSMEANS. We employed Šidák correction to adjust these resulting p-values for multiple comparisons. The same type of model was used for opioid usage, except that due to non-normality, the rank values for opioid usage were modeled as opposed to the actual measured values. Drug usage was analyzed via Fisher’s exact test and values were unadjusted for multiple comparisons.
Nausea, sedation and satisfaction scores were also measured at 1, 24, 48 and 72 h and the groups were compared using the Cochran-Mantel-Haenszel test. Group sample sizes were determined from a statistical power analysis. Based on previous data analysis, our study would be able to detect a 60% decrease in opioid usage between the two groups with a sample size of 40 per group (30 assuming a 25% dropout rate), assuming a two-sided test conducted at a 5% significance level [Citation12].
Results
A total of 78 patients completed the study, including 38 in the LB group and 40 in the SB group. Demographic characteristics (age, sex, race, BMI) were similar between groups, as was the duration of surgery ().
Table 1. Characteristics of study participants.
Analysis showed no difference between the groups in reported pain scores either at rest or with movement at 1, 24, 48 and 72 h (; p > 0.05). Opioid usage was also similar between the groups at all time points (). Sedation and nausea scores and patient satisfaction were all similar between both groups at all time points (). Patient satisfaction was very high, with 100% of patients reporting ‘satisfied’ or ‘very satisfied’ at 24 h and 97% reporting those categories at 48 h. The LB group had a significantly higher requirement for metoclopramide at 48 h postoperatively (8/38 patients [21.1%] vs 0/40 patients in the SB group; p = 0.002; ).
Table 2. Postoperative pain scores, opioid consumption and requirement for other drugs following colorectal surgery with either liposomal or standard bupivacaine in quadratus lumborum blocks.
Table 3. Nausea and sedation scores and patient satisfaction results following colorectal surgery with either liposomal or standard bupivacaine in quadratus lumborum blocks.
Discussion
In this study of patients receiving QL blocks for pain control after colorectal surgery, the liposomal form of bupivacaine provided no analgesic benefit – in terms of postoperative pain scores, opioid consumption or hospital length of stay – over standard bupivacaine alone. LB has been presented as a promising novel analgesic agent with a duration of action of up to 72 h, with a much higher cost than SB. The cost difference at our institution in July 2020 was approximately US$333, making the use of LB difficult to justify even if it provided a marginal benefit in efficacy. Since our study results showed no benefit, we have discontinued the use of LB for QL blocks.
The LB group even showed a trend toward higher opioid requirements and increased pain scores compared with the SB group, although there was no statistical difference. The use of LB did lead to a significant increase in requirement for metoclopramide to treat nausea at 48 h postoperative. This is another factor to dissuade one from using LB for this application.
Given the marketing of LB and its efficacy in some other block applications, we had originally anticipated that it would provide superior analgesia in QL blocks. However, the results were contrary to our original hypothesis. One possible reason is that LB leads to a lower concentration of bupivacaine released at the sensory nerves, and this may not be high enough to provide effective nerve blockade. Equivalent block volumes were delivered between LB and SB groups, so there should have been equal initial spread between the two groups along the sensory nerves. Since bupivacaine is released from the liposomal product in small amounts over time, the concentration of anesthetic at a given time may be too low for effective analgesia.
The possibility of QL block failure could be considered as an explanation for the study results. However, other studies have demonstrated good efficacy of QL blocks – as indicated by lower postoperative opioid requirement and/or pain scores compared with no block or transversus abdominis plane block [Citation13–23]. The attending anesthesiologists at our large academic hospital perform a high volume of regional analgesia, as most have experience with well over 100 QL block procedures. Resident involvement in study procedures is unavoidable, but the trainees are closely monitored by an attending anesthesiologist. We do not anticipate that there was a large number of block failures, although this is recognized as a limitation of the study.
There are several other potential limitations to our study. Although our sample size was adequate to measure our study end points, a larger sample size might have revealed other findings. Also, although the patients and the study coordinators who collected the study data were blinded, we were unable to blind the proceduralists because LB has a different physical appearance than SB. We perform only QL1 blocks at our hospital since we do all our blocks after induction, while the patient is in supine position. Other anesthesiologists may perform transmuscular QL blocks which require a lateral patient position; therefore, different results might be obtained with other QL block techniques.
Conclusion
In conclusion, this comparison of QL blocks with liposomal or standard bupivacaine for patients undergoing colorectal surgery showed that LB combined with SB did not provide superior analgesia over SB alone. These findings are clinically relevant for analgesic protocols in colorectal surgery, and might be expanded to other abdominal surgeries. The use of LB cannot be justified given its increased cost and lack of benefit to the patient compared with SB. Further studies should be performed to determine the effectiveness of LB in truncal blocks, but based on our results, we cannot recommend the use of LB in the QL block for postoperative analgesia following colorectal surgery. We will continue to evaluate LB for other applications at our institution.
Pain after surgery increases opioid usage, thus increasing opioid-related side effects.
Regional procedures to decrease postoperative pain can decrease opioid usage.
Liposomal bupivacaine (Exparel®) combined with bupivacaine HCl does not prolong duration of analgesia from quadratus lumborum (QL) blocks compared with bupivacaine HCl (standard bupivacaine) alone.
Exparel® is significantly more expensive than standard bupivacaine, so its higher cost does not justify routine usage for QL blocks.
Liposomal and standard bupivacaine have a similar side effect profile.
Standard bupivacaine is the agent of choice for cost–effectiveness in the setting of ERAS practice for laparoscopic colorectal surgery.
Author contributions
Y Yeap, J Wolfe, J Stewart, A McCutchan and G Chawla contributed to the conception or design of the work and acquisition, analysis or interpretation of data for the work. B Robb, B Holcomb and B Vickery contributed to the acquisition, analysis or interpretation of data for the work. All authors contributed to drafting the work or revising it critically for important intellectual content and final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved. The authors state that they obtained verbal and written informed consent from the patient/patients for the inclusion of their medical and treatment history within this case report.
Acknowledgments
The authors acknowledge PF Castelluccio (Department of Biostatistics, Indiana University, Indianapolis, Indiana, USA) for assistance with statistics.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Medical writing, editing, reference management and data preparation support was provided by JS Renschler (Department of Anesthesia, Indiana University, Indianapolis, Indiana, USA) and was funded by Indiana University in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Data sharing statement
The authors certify that this manuscript reports original clinical trial data. Individual, de-identified participant data that underlie the results reported in this article (text, tables, figures) are available from the corresponding author following publication, including the clinical study report and study protocol.
References
- Helander EM , BilleaudCB , KlineRJet al. Multimodal approaches to analgesia in enhanced recovery after surgery pathways. Int. Anesthesiol. Clin.55(4), 51–69 (2017).
- Helander EM , WebbMP , BiasM , WhangEE , KayeAD , UrmanRD. Use of regional anesthesia techniques: analysis of institutional enhanced recovery after surgery protocols for colorectal surgery. J. Laparoendosc Adv. Surg. Tech. A27(9), 898–902 (2017).
- El-Boghdadly K , ElsharkawyH , ShortA , ChinKJ. Quadratus Lumborum Block Nomenclature and Anatomical Considerations. Reg. Anesth. Pain Med.41(4), 548–549 (2016).
- Dasta J , RamamoorthyS , PatouG , SinatraR. Bupivacaine liposome injectable suspension compared with bupivacaine HCl for the reduction of opioid burden in the postsurgical setting. Curr. Med. Res. Opin.28(10), 1609–1615 (2012).
- EXPAREL [package insert]. Pacira Pharmaceuticals, CA, USA (2018).
- Gorfine SR , OnelE , PatouG , KrivokapicZV. Bupivacaine extended-release liposome injection for prolonged postsurgical analgesia in patients undergoing hemorrhoidectomy: a multicenter, randomized, double-blind, placebo-controlled trial. Dis. Colon Rectum54(12), 1552–1559 (2011).
- Ma TT , WangYH , JiangYFet al. Liposomal bupivacaine versus traditional bupivacaine for pain control after total hip arthroplasty: a meta-analysis. Medicine (Baltimore)96(25), e7190 (2017).
- Yu ZX , YangZZ , YaoLL. Effectiveness of liposome bupivacaine for postoperative pain control in total knee arthroplasty: a PRISMA-compliant meta-analysis of randomized controlled trials. Medicine (Baltimore)97(13), e0171 (2018).
- Abildgaard JT , ChungAS , TokishJM , HattrupSJ. Clinical efficacy of liposomal bupivacaine: a systematic review of prospective, randomized controlled trials in orthopaedic surgery. JBJS Rev.7(7), e8 (2019).
- Knudson RA , DunlavyPW , FrankoJ , RamanSR , KraemerSR. Effectiveness of liposomal bupivacaine in colorectal surgery: a pragmatic nonsponsored prospective randomized double blinded trial in a community hospital. Dis. Colon Rectum59(9), 862–869 (2016).
- Raman S , LinM , KrishnanN. Systematic review and meta-analysis of the efficacy of liposomal bupivacaine in colorectal resections. J. Drug Assess.7(1), 43–50 (2018).
- Yeap YL , WolfeJW , Backfish-WhiteKMet al. Randomized prospective study evaluating single-injection paravertebral block, paravertebral catheter, and thoracic epidural catheter for postoperative regional analgesia after video-assisted thoracoscopic surgery. J. Cardiothorac. Vasc. Anesth.34(7), 1870–1876 (2020).
- Krohg A , UllensvangK , RosselandLA , LangesæterE , SauterAR. The analgesic effect of ultrasound-guided quadratus lumborum block after cesarean delivery: a randomized clinical trial. Anesth. Analg.126, 559–565 (2018).
- Elsharkawy H , El-BoghdadlyK , BarringtonM. Quadratus lumborum block: anatomical concepts, mechanisms, and techniques. Anesthesiology130(2), 322–335 (2019).
- La Colla L , Ben-DavidB. Quadratus lumborum block: conundrums and questions. Reg. Anesth. Pain Med.42(1), 127–128 (2017).
- Ueshima H , OtakeH , LinJA. Ultrasound-guided quadratus lumborum block: an updated review of anatomy and techniques. Biomed. Res. Int.2017, https://doi.org/10.1155/2017/2752876 (2017).
- Kolade O , PatelK , IhejirikaRet al. Efficacy of liposomal bupivacaine in shoulder surgery: a systematic review and meta-analysis. J. Shoulder Elbow Surg.28(9), 1824–1834 (2019).
- Liu Y , ZengY , ZengJ , LiM , WeiW , ShenB. The efficacy of liposomal bupivacaine compared with traditional peri-articular injection for pain control following total knee arthroplasty: an updated meta-analysis of randomized controlled trials. BMC Musculoskelet. Disord.20(1), 306 (2019).
- Vyas KS , RajendranS , MorrisonSDet al. Systematic review of liposomal bupivacaine (exparel) for postoperative analgesia. Plast. Reconstr. Surg.138(4), 748e–756e (2016).
- Mieszkowski MM , Mayzner-ZawadzkaE , TuyakovBet al. Evaluation of the effectiveness of the quadratus lumborum block type I using ropivacaine in postoperative analgesia after a cesarean section: a controlled clinical study. Ginekol. Pol.89, 89–96 (2018).
- Ishio J , KomasawaN , KidoH , MinamiT. Evaluation of ultrasound-guided posterior quadratus lumborum block for postoperative analgesia after laparoscopic gynecologic surgery. J. Clin. Anesth.41, 1–4 (2017).
- Blanco R , AnsariT , GirgisE. Quadratus lumborum block for postoperative pain after caesarean section: a randomised controlled trial. Eur. J. Anaesthesiol.32, 812–818 (2015).
- Oksüz G , BilalB , GürkanYet al. Quadratus lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery: a randomized controlled trial. Reg. Anesth. Pain Med.42, 674–679 (2017).