Abstract
Aim: To compare the effectiveness and tolerability of the lidocaine 700 mg medicated plaster (LMP) and oral first-line medications (OM) for the treatment of postsurgical neuropathic pain (PSNP) in routine clinical practice. Patients & methods: Data from a noninterventional, retrospective 24-week cohort study in patients with localized peripheral NP refractory to at least one recommended OM using anonymized German Pain eRegistry data were retrieved. A subgroup analysis was conducted on 531 datasets of PSNP patients. Results: Pain relief, improvements in pain-related impairments of daily living and quality of life, and tolerability were significantly greater under LMP than under OM (p < 0.001 for all parameters). Conclusion: These real-world data show the effectiveness and good tolerability of LMP for PSNP treatment in routine clinical practice.
Plain language summary
Surgical procedures may lead to chronic postsurgical neuropathic pain often described as burning or shooting pain. This pain can be treated with medications that are swallowed (oral) or applied to the skin (topical). Our study compared the effectiveness and tolerability of the topical lidocaine 700 mg medicated plaster with oral medications in 531 anonymized patient data sets from a German pain registry. Patients on the lidocaine 700 mg medicated plaster had significantly better pain relief, significantly lower impact of pain on activities of daily life and quality of life and tolerated their treatment significantly better than those on oral medications. The lidocaine 700 mg medicated plaster can be considered as an alternative effective and well-tolerated treatment option for postsurgical neuropathic pain in routine clinical practice.
Chronic postsurgical pain is a complication of surgical procedures, which persists beyond the healing process (at least 3 months following surgery) [Citation1,Citation2] and can substantially affect functioning and quality of life [Citation3]. A neuropathic pain component is often observed, but its presence varies greatly depending on the type of surgery [Citation3,Citation4]: for surgeries such as amputation or inguinal herniotomy, proportions can be as high as 80% [Citation3]. Chronic neuropathic pain is characterized by spontaneous (burning, shooting and lancinating) and/or stimulus-evoked amplified pain [Citation5]. It is defined as chronic pain caused by a lesion or disease of the peripheral or central somatosensory nervous system [Citation6].
Chronic postsurgical pain and postsurgical neuropathic pain have both been characterized, and specific clinical research has been conducted to identify appropriate treatments [Citation7]. Unfortunately, however, the International Classification of Diseases (ICD), 10th revision (ICD-10) did not offer appropriate diagnostic categories for the classification of many chronic pain conditions, including postsurgical pain [Citation8]. Owing to the lack of ability to code accurately, identification and diagnosis are hindered, and these conditions may fail to appear in health statistics, which in turn has an impact on research and health policies.
As for other neuropathic pain conditions, symptomatic treatment of chronic postsurgical neuropathic pain (PSNP) is challenging. Main oral and topical medications recommended for neuropathic pain treatment include tricyclic antidepressants (TCAs), the antiepileptics pregabalin and gabapentin, the selective serotonin-norepinephrine reuptake inhibitors (SSNRIs) duloxetine and venlafaxine, lidocaine 700 mg medicated plaster, and the capsaicin 8% patch [Citation9,Citation10]. However, results obtained in randomized controlled clinical trials with currently available pharmacological treatments have been mixed [Citation11–17]. Real-world data obtained from, for example, the German Pain e-Registry (GPeR) could assist in determining the value of the available neuropathic pain medications for the treatment of PSNP. GPeR data were analyzed in a noninterventional retrospective cohort study assessing both the topical treatment lidocaine 700 mg medicated plaster and oral medications for the treatment of localized peripheral neuropathic pain [Citation18]. Here, we present a subgroup analysis of the datasets of all patients with PSNP.
Methods
This subgroup analysis assessed the datasets of all PSNP patients included in a noninterventional retrospective cohort study in patients with localized peripheral neuropathic pain described earlier [Citation18]. The original study compared the effectiveness and tolerability of lidocaine 700 mg medicated plaster (LMP) with oral first-line treatments (recommended by the current German guideline for the treatment of neuropathic pain [Citation19]) in patients refractory to at least one recommended oral first-line medication (OM; single drug or a combination of drugs). Data had been extracted from the previously described GPeR, a national web-based pain treatment registry [Citation18,Citation20]. The GPeR was developed to provide patients and physicians with a standardized electronic documentation program to gather and evaluate all patient-reported information deemed necessary for the individual routine medical care of pain patients. Patient demographics, medical history, previous treatment and all pain treatment-related data are prospectively obtained by standardized questionnaires with a broad spectrum of validated assessment instruments [Citation21] via the online documentation service iDocLive®. According to GPeR standard procedures, data made available for healthcare research are anonymized, temporarily extracted from the database, and deleted after completion of the analyses specified in the research project.
Data selection
There was no formal sample size calculation for this analysis. The original study included all data sets of patients with newly initiated treatment with one of the medications under evaluation before 31 December 2018 (cut-off 31 July 2019) according to defined inclusion and exclusion criteria [Citation18]. Eligible data sets were of adult outpatients with medically confirmed localized peripheral neuropathic pain and a pain history of at least 3 months who were unsuccessfully treated with at least one first-line OM (single drug or a combination of drugs). This subgroup analysis included all PSNP patients. Treatment initiation was defined as no use of a medication under evaluation in the 12 weeks prior to treatment; the date of first treatment dose was set as the starting date for the 24-week assessment period. All treatment decisions such as selection of analgesic medication and concomitant analgesics, initial dosing and dose adjustments were at the discretion of the treating physician and were solely based on individual patient needs.
The data selection process has been previously described [Citation20]. As of 31 July 2019, the database of the original study contained data sets of 22,702 patients with a localized peripheral neuropathic pain condition [Citation18]. LMP treatment was documented for 4014 patients, OM treatment for 18,688 patients. A matched pair approach using propensity score matching was chosen to obtain comparable study cohorts and employed the nearest neighbor method for the predefined confounding factors age, sex, 24-h pain intensity index, pain severity [Citation22], chronification stage [Citation23], pain duration, comorbidities (ICD-10 code, first three digits), indications/diagnosis for treatment, previous medication (ATC code, first three digits and/or medication group) and reason for switching (effectiveness, tolerability, drug-related adverse events [DRAEs]). The matching was carried out on eligible data of 3170 LMP patients and 11,129 OM patients and resulted in the inclusion of 531 pairs of data sets from patients with a diagnosis of PSNP in this subgroup analysis.
Outcome measures
This subgroup analysis used the same outcome measures as the original study [Citation18]. Treatment effectiveness was assessed using the following parameters:
Pain intensity, rated on a 100 mm visual analogue scale (VAS) with 0 = no pain to 100 = worst imaginable pain. A pain intensity index (PIX) was calculated as the arithmetic mean of the lowest, average, and highest 24-h pain intensities.
Pain-related impairments in daily activities related to ‘home and family’, ‘recreation’, ‘social activities’, ‘occupation’, ‘self-care/personal maintenance’, ‘sleep’ and ‘overall quality of life’, reported with a modified version of the original pain disability index [Citation24] (mPDI) on a 100 mm VAS (0 = none to 100 = worst imaginable).
Pain-related quality of life, measured by the quality of life impairment by pain inventory questionnaire (QLIP) rating well-being, sleep, pain, impairments, and mood with a sum score ranging from 0 to 40 points. A sum score of ≤20 points indicates severe impairment.
Overall quality of life, assessed with the eight physical and mental domains of the Short Form 12 version 2 (SF-12v2) questionnaire [Citation25] and summarized in a physical and a mental component score (PCS/MCS).
Patients’ clinical pain phenotype, determined using the modified 7-item version of the validated PainDETECT questionnaire (PDQ7 [Citation26]). A sum score of 0–10 indicates that a neuropathic pain component is unlikely (negative), of >10 to <18 that a neuropathic component might be present (unclear), and of ≥18 that a neuropathic component is likely present (positive).
Patients’ change in health status, assessed by the Patient Global Impression of Change (PGIC) scale ranging from 1 = very much improved to 7 = very much worse [Citation27].
Tolerability assessments were based on the occurrence of DRAEs and treatment discontinuation due to DRAEs. A DRAE was defined as an adverse event (AE) assessed to be possibly, probably, or definitely related to the medication under evaluation.
Statistical analysis
Statistical analyses were carried out as stated for the original study [Citation18]. Patients were included in the analysis if they received at least one dose of the relevant medication under evaluation and had at least one post-baseline/post-dose measure. Assessments of changes from baseline to endpoint included only data, if there was both a baseline and corresponding post-baseline measure. For the primary effectiveness endpoint, missing data were imputed using the baseline observation carried forward approach for data sets from patients who discontinued treatment (due to an AE, death or lack of effectiveness). Otherwise, the last observation carried forward method was used for the primary and all secondary variables.
The primary effectiveness endpoint was the absolute change in average 24-h PIX from baseline following 4, 12 and 24 weeks of treatment and over the entire treatment period. Secondary effectiveness endpoints were the change from baseline at the three timepoints in average 24-h PIX (relative change), in pain-related impairments in daily life, in clinical pain phenotype, in quality of life impairment by pain and in overall quality of life, response to treatment (defined as ≥30% and ≥50% reduction in PIX), patients’ impression of change in health status, patients with DRAEs, reasons for premature discontinuation, discontinuation of treatment due to DRAEs, and change in concomitant medications during the observation period. Treatment differences were compared by conducting mixed-model repeated measures covariance analyses (adjusted for potential confounding factors such as age, gender, pain severity, stage of chronification, history/duration of pain, comorbidity, comedication and prior and current medication at baseline, as well as baseline value). Student’s t-test, Pearson’s chi-square test and Fisher’s exact test were used for between-group comparisons of continuous and categorical variables. For within-group comparisons, paired samples t-tests were performed. All statistical tests were carried out using a two-sided significance level of 0.05. There were no adjustments for multiplicity. The effect size of the comparisons for the primary variable was determined with Cohen’s d. All analyses were performed with PASW Statistics version 18. AEs were encoded using the Medical Dictionary for Regulatory Activities (MedDRA version 22.0).
Results
Patients
A total of 3081 patients with localized peripheral neuropathic pain including 531 PSNP patients per treatment group could be matched by the propensity score approach. shows the baseline data for the two PSNP treatment groups. The majority of patients (LMP 64.6%/OM 66.7%) had suffered from pain for more than a year; they had visited a median of eight physicians.
Table 1. Baseline characteristics of all patients with postsurgical neuropathic pain.
Analgesic treatment
Mean treatment duration in the LMP group was 144.8 ± 47.5 days (95% CI: 140.8–148.9). A total of 26.2% of LMP patients discontinued treatment earlier than 24 weeks. The main reason was ‘pain treatment no longer required’ (13.6% of patients) followed by ‘lack of efficacy’ (4.7%), ‘due to DRAEs’ (4.5%), and ‘unclear information’ (3.4%).
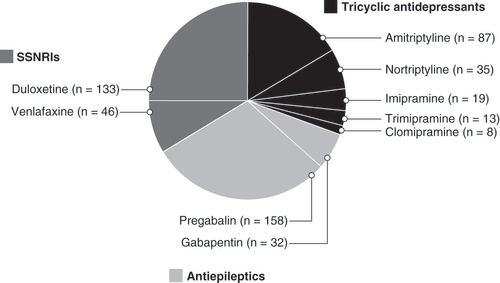
Patients in the OM group received antiepileptic medications (35.8%), selective serotonin-norepinephrine reuptake inhibitors (SSNRIs; 33.7%) or tricyclic antidepressants (TCAs; 30.5%; ). Pregabalin (29.8%), duloxetine (25%), and amitriptyline (16.4%) were prescribed most often. Mean treatment duration was 105.8 ± 66.2 days (95% CI: 100.1–111.4). Premature treatment discontinuation was documented for 52.7% of OM patients; main reasons were due to DRAEs (30.7%) followed by ‘lack of efficacy’ (12.8%), ‘pain treatment no longer required’ (6.4%), and ‘unclear information’ (2.8%).
OM: Oral first-line medication; SSNRI: Selective serotonin-norepinephrine reuptake inhibitor.
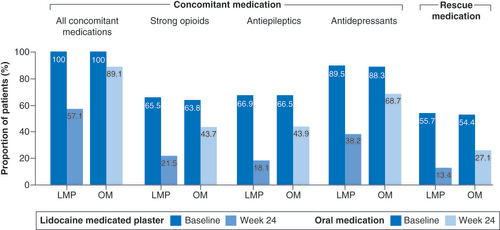
At baseline, all patients in both treatment groups received concomitant analgesic medications (). After 24 weeks of treatment, a reduction in concomitant analgesic use (93 vs 69.9%; p < 0.001) as well as in rescue medication (48.6 vs 38.2%; p < 0.001) was observed in significantly more LMP than OM patients. At the end of observation, a greater proportion of LMP than OM patients had discontinued concomitant analgesic and rescue medication ().
Pain intensity
The mean PIX at baseline was 65.6 ± 14.5 mm for LMP and 65.5 ± 14.4 mm for OM patients. Pain intensity improved in both treatment groups over the observation period. Reductions in the primary effectiveness endpoint, the absolute change in average 24-h PIX from baseline were, however, significantly greater for LMP than OM patients at the three timepoints 4, 12 and 24 weeks of treatment (A) with an effect size of 0.62 at end of observation. The mean (standard error [SE]) change in absolute scores for average 24-h PIX over the 24-week treatment period was -30.7 mm (0.43) and -18.33 mm (0.59) in LMP and OM patients, respectively. At the end of observation, the relative mean change from baseline in PIX was 51.3% for LMP patients and 29.9% for OM patients (p < 0.001, Cohen’s d = 0.82).
(A) Change from baseline over the observation period. (B) Improvement versus baseline at end of observation.
PIX: Pain intensity index.
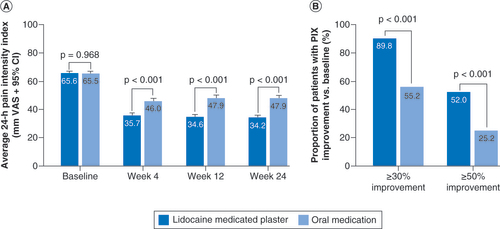
Response to treatment after 24 weeks (defined as ≥30 and ≥50% reduction in PIX) was also significantly better in the LMP than in the OM group (B).
Further outcome measures
Mean PDQ7 scores had decreased from 27.1 ± 3.4 (95% CI: 26.8–27.4) in both treatment groups at baseline to 15.3 ± 4.3 (95% CI: 15.0–15.7) for LMP and 21.7 ± 4.8 (95% CI: 21.3–22.1) for OM patients at end of week 24 (p < 0.001 in favor of LMP).
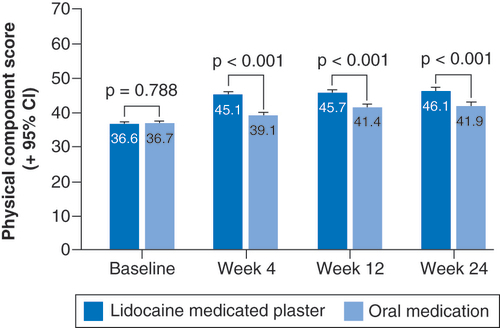
At baseline, the physical component score of the overall quality of life SF-12 parameter was markedly affected in both patient groups (). Under LMP treatment, it had already considerably improved after 4 treatment weeks with a further slight increase until the end of observation. Improvements at 24 weeks were significantly greater than in the OM group (p < 0.001) with relative increases from baseline of 14.4 and 8%, respectively.
Analysis of pain-related disability, further quality of life parameters and change in health status all showed a significant difference in favor of LMP compared to OM after 24 treatment weeks (p < 0.001; ).
Table 2. Outcome of further effectiveness parameters at the end of observation.
Tolerability
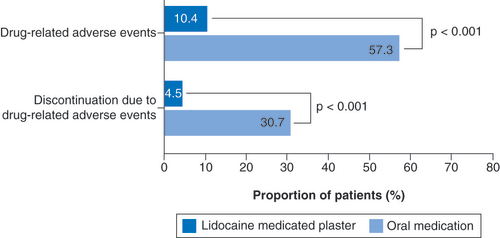
Significantly fewer LMP than OM patients reported DRAEs (10.4 vs 57.3%; p < 0.001; ). In the LMP group, the events were mainly application site reactions and other skin-related reactions (7.5%; ). OM patients reported mostly nervous system disorders (24.1%), psychiatric disorders (23.4%) and gastrointestinal disorders (18.6%; ). The most common event in this group was somnolence (14.5% of patients). A significantly smaller proportion of patients in the LMP group discontinued treatment due to DRAEs (4.5 vs 30.7% for OM patients; p < 0.001; ).
Table 3. All drug-related adverse events reported in patients receiving lidocaine 700 mg medicated plaster during the observation period (n = 531).
Table 4. Main drug-related adverse events reported in patients receiving oral first-line medication during the observation period (n = 531).
Discussion
Chronic postsurgical pain is a common complication of surgical procedures, which persists beyond the healing process and can substantially affect functioning and quality of life [Citation3]. The aim of this study was to investigate the effectiveness and tolerability of the lidocaine 700 mg medicated plaster and oral first-line medications in routine medical care of patients with PSNP.
More than half of all patients in this multimorbid study population had experienced pain after surgery for more than a year; treatment with at least one oral first-line medication had been insufficient, pain burden was high, and quality of life, in particular the physical component, was markedly affected. The 24-week treatment with LMP resulted in pronounced reductions in pain intensity, improvements in daily functioning, and a better health status. Effectiveness was maintained over the treatment period, and quality of life improved despite reduction (observed in 93% of LMP patients) or discontinuation of concomitant analgesic medications (observed in over 40% of LMP patients). In addition, treatment with the plaster was well tolerated. The overall incidence of LMP-related adverse events was low and was mainly associated with plaster application and other skin-related tolerability issues.
The comparison with matched patients treated with oral medications revealed significantly greater improvements in pain intensity, in pain-related impairments of daily living and quality of life for LMP. The observed reduction in neuropathic pain symptoms was also significantly greater in the LMP group. In addition, the lack of systemic side effects of the plaster provided a significantly better tolerability profile in contrast to more than 50% of OM patients with mainly nervous system, psychiatric and gastrointestinal drug-related adverse events. Treatment discontinuation due to DRAEs was also significantly lower in the LMP compared to the OM group (4.5 vs 30.7%). These findings confirm the previously reported good tolerability of the plaster [Citation28] and the generally better adverse event profile compared to oral medications [Citation29,Citation30].
The efficacy of LMP in PSNP treatment has been the subject of several recent randomized clinical trials [Citation14,Citation16,Citation17,Citation31]. LMP treatment was well tolerated and showed effective pain relief after different surgeries; however, statistical significance was not reached in one of these trials [Citation17]. LMP relieved localized neuropathic pain and improved several neuropathic characteristics and clinical allodynia symptoms after knee surgery [Citation16], significantly alleviated pain and sleep disturbances in the treatment of chronic post-thoracotomy neuropathic pain [Citation14] and led to neuropathic pain reduction over time in patients with foot and ankle orthopedic surgery and provided a high degree of patient satisfaction [Citation31]. The real-world data analysis reported here supports the findings obtained from randomized controlled trials and indicates a better response to LMP than to oral medications in the routine practice treatment of PSNP.
The GPeR uses standardized processes to collect data from various pain practices around Germany. Medications are prescribed at the discretion of the treating physicians, and their use is not necessarily consistent with the product label. Nevertheless, it is remarkable that only 531 of the 3081 matched patients with localized peripheral neuropathic pain were identified as having PSNP (i.e., 17.2%). This proportion seems to be very low based on an assumed much higher PSNP prevalence compared to postherpetic neuralgia prevalence, which is considered to be an orphan disease by the FDA (i.e., a condition affecting fewer than 200,000 patients in the US) [Citation32]. It might be the result of the current restricted LMP product label in the European Union but might also be due to an underdiagnosis of the condition given the limitations of the current ICD-10 classification. In the new ICD-11, a diagnostic coding is offered for ‘chronic postsurgical pain’ and may be accompanied by a code for ‘chronic peripheral neuropathic pain’ in case neuropathic pain is present [Citation1]. This new coding system offering clear diagnostic categories for chronic pain conditions as well as neuropathic pain conditions will in the future ensure better understanding of the prevalence of these conditions.
This subgroup analysis has all the limitations noted for the original noninterventional retrospective cohort study [Citation18]. Although a study protocol and a statistical analysis plan were developed a priori and a matched pair approach with propensity score matching was employed and eliminated the main confounding factors, other confounders might have been present. It is not known if study outcomes were influenced by the prescription of specific PSNP treatments based on individual patient needs and the response to previous therapies or if physicians prescribing oral medications might have paid closer attention to side effects. Data not captured by the standard documentation in iDocLive® include patient compliance in taking the prescribed medications under evaluation and reasons for the prescription of concomitant analgesics. An information bias based on documentation errors and misclassifications can also not be ruled out, as only anonymized data were available due to data protection regulations.
Conclusion
The lidocaine 700 mg medicated plaster was effective and well tolerated in the routine medical treatment of postsurgical neuropathic pain. It not only relieved pain but also improved pain-related impairments of daily living and quality of life. The lidocaine 700 mg medicated plaster represents an attractive treatment alternative to oral medications given its reduced risk of systemic side effects and improved treatment compliance resulting in better treatment outcomes.
Chronic postsurgical pain is a complication of surgical procedures, which persists beyond the healing process (at least 3 months following surgery). It can substantially affect functioning and quality of life. If a neuropathic pain component is present (which is often the case), this would be labeled as postsurgical neuropathic pain.
The topical lidocaine 700 mg medicated plaster (LMP) has demonstrated good efficacy with a good tolerability profile in the treatment of localized peripheral neuropathic pain.
To determine the value of LMP and other currently available neuropathic pain medications for the treatment of postsurgical neuropathic pain (PSNP) in routine clinical practice, a subgroup analysis of the datasets of all patients with PSNP from a noninterventional retrospective cohort study was carried out. Data in the original study were extracted from the German Pain eRegistry.
The study compared the effectiveness and tolerability of LMP and first-line oral medications (OM) over a 24-week period in PSNP patients refractory to at least one OM treatment. Propensity score matching provided 3081 data sets of patients with localized peripheral neuropathic pain including 531 PSNP patients per treatment group.
More than 60% of patients had experienced pain for more than a year and reported a high burden of pain and reduced quality of life.
LMP treatment provided significantly greater pain reductions and improvements in pain-related impairments of daily living and quality of life than OM treatment over the 24-week observation period (p < 0.001 for all parameters). A significantly greater reduction in neuropathic pain symptoms was observed in the LMP group.
Almost all LMP patients were able to reduce concomitant analgesic medication and more than 40% discontinued these medications.
The proportion of patients with drug-related adverse events (DRAEs) was significantly lower under LMP treatment (p < 0.001); DRAEs consisted mainly of application site reactions. Significantly fewer LMP than OM patients discontinued treatment due to DRAEs (p < 0.001).
In routine medical care, chronic PSNP patients unsuccessfully treated with first-line oral medications had a significantly better response to newly initiated LMP treatment with a significantly better tolerability profile when compared to OM treatment.
Author contributions
Conception and design: All authors. Data extraction: MA Überall. Data analysis: MA Überall. Data interpretation: All authors. All authors critically revised for important intellectual content, approved the final manuscript version, and agreed to the submission.
Ethical conduct of research
The original study is registered in the European Union electronic Registry of Post-Authorization Studies (EUPAS 32826) through the European Network of Centers for Pharmacoepidemiology and Pharmacovigilance (ENCePP®) coordinated by the European Medicines Agency and was conducted in accordance with the Declaration of Helsinki and relevant national and regulatory requirements. The concept and use of the German Pain e-Registry have been reviewed and approved by the steering committees of the German Pain Association and the German Pain League. All patients provided written informed consent prior to participation in the registry. All analyses were carried out using only anonymized data to comply with German guidelines on protection of data privacy and with the European Union General Data Protection Regulation.
Financial & competing interest disclosures
MA Überall is a physician, pain specialist, medical director of the Institute of Neurological Sciences, and CEO of O.Meany-MDPM GmbH, which was responsible for data extraction and biometrical analyses. Data extraction and biometrical analyses have been paid for by Grünenthal GmbH, Germany. MA Überall has received financial support and/or expenses in form of research funds, consultancy fees and/or renumerations for lecture activities from: Allergan, Almirall, Amicus Therapeutics, Aristo Pharma, Bionorica, Esanum, GlaxoSmithKline, Grünenthal, Hapa Medical, Hexal, IMC, Kyowa-Kirin, Labatec, Mucos, Mundipharma, Nestle, Pfizer, Recordati, Servier, SGP-Pharma, Shionogi, Spectrum Therapeutics, Strathmann, Teva and Tilray. I Bösl, E Hollanders, I Sabatschus and M Eerdekens are employees of Grünenthal GmbH, Germany. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Writing and editorial assistance was provided by Elke Grosselindemann and Birgit Brett and was paid for by Grünenthal GmbH, Germany.
Additional information
Funding
References
- Treede RD , RiefW , BarkeAet al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International Classification of Diseases (ICD-11). Pain160, 19–27 (2019).
- Schug SA , Lavand’hommeP , BarkeA , KorwisiB , RiefW , TreedeRD. The IASP classification of chronic pain for ICD-11: chronic postsurgical or posttraumatic pain. Pain160, 45–52 (2019).
- Schug SA , BruceJ. Risk stratification for the development of chronic postsurgical pain. Pain Rep.2, e627 (2017).
- Haroutiunian S , NikolajsenL , FinnerupNB , JensenTS. The neuropathic component in persistent postsurgical pain: a systematic literature review. Pain154, 95–102 (2013).
- Baron R , BinderA , WasnerG. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol.9, 807–819 (2010).
- Scholz J , FinnerupNB , AttalNet al. The IASP classification of chronic pain for ICD-11: chronic neuropathic pain. Pain160, 53–59 (2019).
- Shipton E . Post-surgical neuropathic pain. ANZ J Surg.78, 548–555 (2008).
- Rief W , KaasaS , JensenRet al. The need to revise pain diagnoses in ICD-11. Pain149, 169–170 (2010).
- Attal N , CruccuG , BaronRet al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur. J. Neurol.17, 1113–e88 (2010).
- Finnerup NB , AttalN , HaroutounianSet al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol.14, 162–173 (2015).
- Cheville AL , SloanJA , NorthfeltDWet al. Use of a lidocaine patch in the management of postsurgical neuropathic pain in patients with cancer: a phase III double-blind crossover study (N01CB). Support. Care Cancer17, 451–460 (2009).
- van Seventer R , BachFW , TothCCet al. Pregabalin in the treatment of post-traumatic peripheral neuropathic pain: a randomized double-blind trial. Eur. J. Neurol.17, 1082–1089 (2010).
- Bischoff JM , RingstedTK , PetersenM , SommerC , ÜçeylerN , WernerMU. A capsaicin (8%) patch in the treatment of severe persistent inguinal postherniorrhaphy pain: a randomized, double-blind, placebo-controlled trial. PLoS One9, e109144 (2014).
- Sansone P , PassavantiMB , FiorelliAet al. Efficacy of the topical 5% lidocaine medicated plaster in the treatment of chronic post-thoracotomy neuropathic pain. Pain Manage.7, 189–196 (2017).
- Markman J , ResnickM , GreenbergSet al. Efficacy of pregabalin in post-traumatic peripheral neuropathic pain: a randomized, double-blind, placebo-controlled phase 3 trial. J. Neurol.265, 2815–2824 (2018).
- Pickering G , VouteM , MacianN , GanryH , PereiraB. Effectiveness and safety of 5% lidocaine-medicated plaster on localized neuropathic pain after knee surgery: a randomized, double-blind controlled trial. Pain160, 1186–1195 (2019).
- Palladini M , BoeslI , KoenigS , BuchheisterB , AttalN. Lidocaine medicated plaster, an additional potential treatment option for localized post-surgical neuropathic pain: efficacy and safety results of a randomized, placebo-controlled trial. Curr. Med. Res. Opin.35, 757–766 (2019).
- Überall MA , BöslI , HollandersE , SabatschusI , EerdekensM. Localized peripheral neuropathic pain – topical treatment with lidocaine 700 mg medicated plaster in routine clinical practice. Pain Manage.12, 521–533 (2022).
- Schlereth T . Guideline “diagnosis and non interventional therapy of neuropathic pain” of the German Society of Neurology (Deutsche Gesellschaft für Neurologie). Neurol Res Pract.2, 16 (2020).
- Überall MA , EerdekensM , BöslI , HollandersE , SabatschusI. Lidocaine 700 mg medicated plaster for postherpetic neuralgia: real-world data from the German Pain e-Registry. Pain Manage.12, 195–209 (2022).
- German Pain Society . Manual for the German pain questionnaire (in German). https://www.schmerzgesellschaft.de/fileadmin/pdf/DSF_Handbuch_2020.pdf
- von Korff M , OrmelJ , KeefeFJ , DworkinSF. Grading the severity of chronic pain. Pain50, 133–149 (1992).
- Schmitt N , GerbershagenHU. The Mainz Staging System (MPSS) for chronic pain. Pain41(Suppl. 5), S484 (1990).
- Tait RC , ChibnallJT , KrauseS. The pain disability index: psychometric properties. Pain40, 171–182 (1990).
- Hayes CJ , BhandariNR , KatheN , PayakachatN. Reliability and validity of the medical outcomes study short form-12 version 2 (SF-12v2) in adults with non-cancer pain. Healthcare (Basel)5, 22 (2017).
- Cappelleri JC , BienenEJ , KoduruV , SadoskyA. Measurement properties of painDETECT by average pain severity. Clinicoecon Outcomes Res.6, 497–504 (2014).
- Guy W . ECDEU assessment manual for psychopharmacology (DHEW Publication no. ADM 76–338). US Government Printing Office, DC, USA (1976).
- Navez ML , MonellaC , BöslI , SommerD , DelormeC. 5% lidocaine medicated plaster for the treatment of postherpetic neuralgia: a review of the clinical safety and tolerability. Pain Ther.4, 1–15 (2015).
- Buksnys T , ArmstrongN , WorthyGet al. Systematic review and network meta-analysis of the efficacy and safety of lidocaine 700 mg medicated plaster vs. pregabalin. Curr. Med. Res. Opin.36, 101–115 (2020).
- Katz P , PegoraroV , LiedgensH. Characteristics, resource utilization and safety profile of patients prescribed with neuropathic pain treatments: a real-world evidence study on general practices in Europe - the role of the lidocaine 5% medicated plaster. Curr. Med. Res. Opin.33, 1481–1489 (2017).
- Macedo RDR , SantosJPGD , LobatoES , MendesJP , IkemotoRY , RodriguesLMR. Application of 5% lidocaine adhesive patch in painful surgical scars: clinical trial. Rev. Bras. Ortop. (Sao Paulo)56, 601–614 (2021).
- Businesswire . FDA grants orphan drug designation to postherpetic neuralgia treatment. https://www.businesswire.com/news/home/20130927005456/en/Zalicus%E2%80%99-Z160-Receives-Orphan-Drug-Designation-for-the-Management-of-Postherpetic-Neuralgia