Abstract
Calcification of the medial collateral ligament is a rare cause of medial knee pain along with functional impairment. Most cases are asymptomatic but those that are symptomatic typically respond to conservative management. However, in those instances with persistent symptoms that desire further intervention but want to minimize the risks associated with surgery, we present a novel approach for calcium removal with an ultrasound-guided percutaneous needle tenotomy with TenJet™ as a reasonable treatment modality.
Calcific tendinopathy most commonly occurs within the rotator cuff of the shoulder but also presents in the hip, thigh, knee, ankle and foot [Citation1]. Although rare and often asymptomatic in the knee, those cases producing symptoms can result in debilitating pain and function. Several instances have been described in the current literature affecting the medial collateral ligament (MCL) of the knee often involving the ligament itself or Voshell’s bursa [Citation2,Citation3]. Treatments range from supportive with observation, physical therapy, corticosteroid injections, extracorporeal shockwave therapy and arthroscopic or open surgical removal [Citation3–6]. The current literature on calcification within the MCL is scant and to date there are no universally agreed treatment guidelines.
Alternatively, minimally invasive techniques have been described to treat calcifications through an ultrasound-guided percutaneous lavage [Citation2,Citation7]. This usually involves a double-needle approach while repeated fenestration of the calcification leads to fragmentation of the calcific deposits [Citation2]. However, over recent years percutaneous ultrasonic tenotomy needle devices have been shown to successfully treat tendinopathy and fasciopathy [Citation8,Citation9]. To date only one prior case report has been recently published on using Tenex (Tenex Health, CA, USA) for removal of calcific debris [Citation10]. This report describes the first ever case of calcification within the MCL that was successfully treated with a percutaneous ultrasound-guided resection using the TenJet™ (HydroCision Inc., MA, USA).
Case report
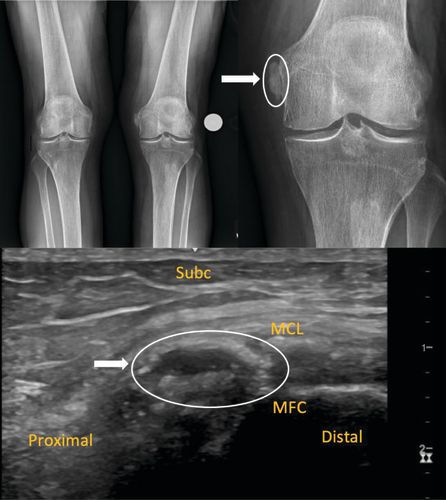
An 81 year-old female with a past medical history of hypertension, hypothyroidism and chronic kidney disease presented with chronic left medial knee pain for 3 years. The pain was rated as an 8/10 and described as dull localized to the superior medial border of the knee and described to have a limited range of motion due to the stiffness and pain. Prior to our initial evaluation, the patient attempted ice, heat, oral nonsteroidal anti-inflammatory drugs (NSAIDs) and started physical therapy. She denied any fevers, weight loss or gain, history of trauma and history of knee surgery. On examination, she could ambulate without assistance or antalgic. No erythema or effusion was noted. She had a full range of motion passively but actively experienced tightness in the medial knee. There was focal tenderness over the proximal MCL and crepitus with knee extension. The remainder of the examination was normal. Plain films showed mild tricompartmental osteoarthritis, chonedrocalcinosis and a lobulated calcification measuring 2.4 cm at the medial femoral condyle. (). Diagnostic musculoskeletal ultrasound was performed showing a multi-lobulated calcification in the superficial fibers of the proximal MCL measuring 2.4 × 0.8 × 1.2 cm with posterior acoustic shadowing (). There was no noted neovascularization with power doppler within the calcification. The MCL was intact without laxity upon valgus stress dynamic testing. A diagnostic 5 ml 0.5% Ropivacaine injection was performed intra-articular without any pain relief. A follow-up diagnostic injection with 2 ml of 0.5% Ropivacaine was performed using a 25 gauge 1.5” needle under ultrasound guidance directly into the calcification noted within the MCL to confirm the source of pain. Following this injection into the MCL calcification, the patient’s knee was pain-free and had a full range of passive and active range of motion. Various modalities including surgical removal or percutaneous ultrasound-guided vacuum resection were discussed in which the patient proceeding with a percutaneous approach.
Initial evaluation where a 2.4 mm calcification is noted at the left femoral medial condyle (white arrow), also showed lateral compartment chondrocalcinosis and mild osteoarthritis (upper panel). Initial diagnostic musculoskeletal ultrasound imaging of the medial knee in a longitudinal view showing a lobulated calcium at the medial femoral condyle within the proximal medial collateral ligament. White arrow indicated the calcification of the MCL (lower panel).
Subc: Subcutaneous tissue; MCL: Medial collateral ligament; MFC: Medial femoral condyle.
The procedure was performed in an ambulatory surgical center under sterile conditions. The patient was placed supine and the calcification within the MCL was identified with ultrasound. A total volume of 3 ml of 0.5% Ropivacaine was used on a 25g 1.5” needle to anesthetize the MCL and subcutaneous tissue. A skin wheal with 2 ml lidocaine and 1% epinephrine was performed in the superficial layer. Then, using a No. 11 blade a small 3 mm incision was made through which the TenJet device was placed and advanced into the area of calcification. Under ultrasound guidance, the TenJet device was utilized to deliver high-velocity sterile saline with a Venturi suction effect at the 12-gauge needle tip creating a cutting window to remove the calcific debris (). The total treatment time was for approximately 3 min until there was a sonographic resolution of the calcification. The incision was closed with Steri-Strips (3M; MN, USA) and then covered with a Tegaderm (3M) dressing. Patients were then placed in a hinged knee brace for 2 weeks post-procedure.
Plain radiographs AP from the 2 week-post procedure appointment showing resolution of the calcification at the medial femoral condyle with persisting lateral compartment chondrocalcinosis and mild osteoarthritis (upper panel). Ultrasound examination in long-axis to the medial collateral ligament during the TenJet™ procedure showing the needle tip (white arrow) penetrating the calcium within the MCL with decreased lucency of the calcium and reduction in size of the calcium (lower panel).
MCL: Medial collateral ligament; Subc: Subcutaneous tissue.
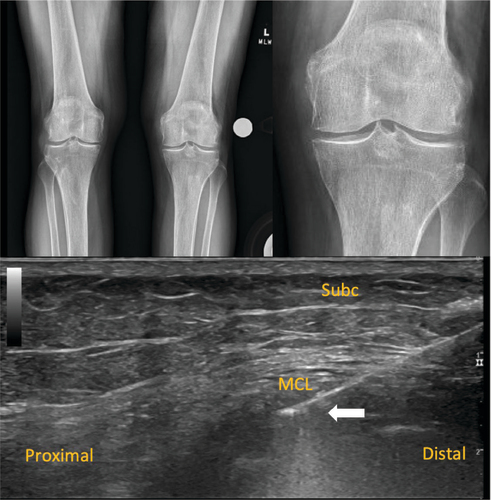
At 2 weeks post-procedure there was complete resolution of the calcification on radiographs (). The patient reported complete relief of her symptoms with a visual analogue scale (VAS) score of 0/10 and subsequently weaned out of the knee brace. Given her resolution of symptoms a shared decision was made not to initiate a physical therapy program. The patient remained without clinical or radiographic evidence of recurrence at her 6 week, 3 month and 1 year follow-up appointments.
Discussion
Calcification of the MCL is a rare cause of medial knee pain and most commonly occurs following a traumatic ligamentous injury to the MCL [Citation11]. However, in our case, there was no known or reported history of trauma. Through the authors’ literature review, there are very few cases ever reported to date describing calcium within the MCL [Citation2–7,Citation10,Citation12–15]. Typically most cases are not symptomatic, but for those that become symptomatic, it is reasonable to initially treat with a conservative approach [Citation15]. However, for those cases in which symptoms persist options remain limited and no current standard of care exists for removal of these lesions. Recalcitrant cases often have been historically treated with surgery as the mainstay of treatment [Citation3].
There are only three other reports of removal through a percutaneous ultrasound-guided approach utilizing previously described techniques [Citation2,Citation10]. Two cases involved the utilization of Tenex which has several differences from TenJet. Tenex uses ultrasonic energy and simultaneously irrigates the tendon with sterile saline while TenJet utilizes high-pressurized saline jet through a cutting window to resect tissue and waste fluid through a Venturi effect at the needle tip [Citation9,Citation16]. Aside from these devices as treatment options, the other modality described in previous literature involves multiple operators with a double needle approach with repeated fenestration [Citation2]. Both scenarios have shown to be an effective and reasonable option. In our case our patient reported to have a faster recovery period compared with prior approaches as the two other patients were noted to have 60 and 80% relief at the first follow-up visit between 10 to 14 days post procedure. To our knowledge, this is the first description of MCL calcification of the knee that was treated with a percutaneous ultrasound-guided resection device utilizing TenJet.
Conclusion
The occurrence of calcification within the MCL is a rare phenomenon that can result in medial knee pain. Clinicians should be aware that this condition may arise without any history of trauma and can lead to considerable pain with functional limitations. Early diagnosis through plain radiographs and advanced imaging is important to further evaluate adjacent structures and other causes of medial knee pain. Although a majority of cases are often asymptomatic, this case report highlights the importance of identifying an unusual presentation in the management of MCL calcification that had not responded to conservative management. Ultrasound-guided percutaneous tenotomy with TenJet is a low-risk procedure and a reasonable treatment option for symptomatic recalcitrant cases.
Calcification of the medial collateral ligament (MCL) is a rare but significant cause of medial knee pain, often treated conservatively, with few cases requiring more invasive interventions.
The report presents a novel, minimally invasive technique using ultrasound-guided percutaneous approach with TenJet™, effectively treating MCL calcification in a patient unresponsive to conservative treatments.
This case highlights the importance of considering MCL calcification in the differential diagnosis of medial knee pain and introduces an effective, low-risk alternative to surgical intervention for symptomatic cases.
Writing disclosure
No writing assistance was utilized in the production of this manuscript.
Ethical conduct of research
The authors state that they have obtained verbal and written informed consent from the patient for the inclusion of their medical and treatment history within this case report.
Acknowledgments
Thanks to the Cleveland Clinic Orthopaedic and Rheumatologic Institute, specifically Cleveland Clinic Sports Medicine research team, staff, and research personnel whose efforts related to this project made this consortium successful.
Financial disclosure
The author has no financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Competing interests disclosure
M Dakkak does consult work with Hydrocision. The author, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article. The author has no other competing interests or relevant affiliations with any organization or entity with the subject matter or materials discussed in the manuscript apart from those disclosed.
References
- Holt PD , Keats TE . Calcific tendinitis: a review of the usual and unusual. Skeletal Radiol. 22(1), 1–9 (1993).
- Galletti L , Ricci V , Andreoli E , Galletti S . Treatment of a calcific bursitis of the medial collateral ligament: a rare cause of painful knee. J. Ultrasound 22(4), 471–476 (2019).
- Muschol M , Müller I , Petersen W , Hassenpflug J . Symptomatic calcification of the medial collateral ligament of the knee joint: a report about five cases. Knee Surg. Sports Traumatol. Arthrosc. 13(7), 598–602 (2005).
- Chang WC , Huang GS , Lee CH , Kao HW , Chen CY . Calcification of medial collateral ligament of the knee: an uncommon cause of medial knee pain. J. Clin. Rheumatol. 12(4), 204–205 (2006).
- Song K , Dong J , Zhang Y et al. Arthroscopic management of calcific tendonitis of the medial collateral ligament. Knee 20(1), 63–65 (2013).
- Vampertzis T , Agathangelidis F , Gkouliopoulou E , Papastergiou S . Massive non-traumatic calcification of the medial collateral ligament of the knee. BMJ Case Rep. 2016, bcr2016217743 (2016).
- Del Castillo-González F , Ramos-Álvarez JJ , González-Pérez J , Jiménez-Herranz E , Rodríguez-Fabián G . Ultrasound-guided percutaneous lavage of calcific bursitis of the medial collateral ligament of the knee: a case report and review of the literature. Skeletal Radiol. 45(10), 1419–1423 (2016).
- Wong AK , Swami PN , Reed TF , Bitterman A , Grande DA . Efficacy and safety of a percutaneous tenotomy system for debridement of tendinopathic tissues. J. Long Term Eff. Med. Implants 28(3), 199–203 (2018).
- Vajapey S , Ghenbot S , Baria MR , Magnussen RA , Vasileff WK . Utility of percutaneous ultrasonic tenotomy for tendinopathies: a systematic review. Sports Health 13(3), 258–264 (2021).
- Sung K , Raja AE , Tunis JG , Tunis BG , Zheng K , Sussman WI . Heterotopic mineralization of the medial collateral ligament: our experience treating two cases of calcific versus ossific lesions with ultrasonic vacuum debridement. Cureus 15(3), e36127 (2023).
- Majewski M , Susanne H , Klaus S . Epidemiology of athletic knee injuries: a 10-year study. Knee 13(3), 184–188 (2006).
- Kamawal Y , Steinert AF , Holzapfel BM , Rudert M , Barthel T . Case report - calcification of the medial collateral ligament of the knee with simultaneous calcifying tendinitis of the rotator cuff. BMC Musculoskelet. Disord. 17, 283 (2016).
- Fernández-Cuadros ME , Albaladejo-Florín MJ , Álava-Rabasa S , Pérez-Moro OS . Calcification of the medial collateral ligament of the knee: rehabilitative management with radial electro shock wave therapy plus iontophoresis of a rare entity. Clinical case and review. Rehabilitacion (Madr). 56(4), 388–394 (2022).
- Siddiq MAB , Jahan I . Medial collateral ligament calcification: a rare knee pain entity with literature review. Acta Radiol. Open 6(11), 2058460117738549 (2017).
- Mansfield HL , Trezies A . Calcific tendonitis of the medial collateral ligament. Emerg. Med. J. 26(7), 543 (2009).
- Kamineni S , Butterfield T , Sinai A . Percutaneous ultrasonic debridement of tendinopathy-a pilot Achilles rabbit model. J. Orthop. Surg. Res. 10, 70 (2015).
