Juvenile fibromyalgia (JFM) is characterized by chronic widespread musculoskeletal pain and painful tender points, along with a number of other symptoms including fatigue, sleep disturbance, headaches and increased anxiety. JFM primarily affects adolescent females and causes substantial disruption in physical and psychosocial functioning Citation[1–5]. Symptoms (and related interference with functioning) often persist for many years into early adulthood Citation[6]. There is no cure for JFM and currently available medical treatments are of limited benefit. Recent efforts have focused on the integration of cognitive–behavioral techniques into usual medical care to assist adolescents with JFM to better manage their symptoms using muscle relaxation, distraction, pacing activities and cognitive restructuring. This type of cognitive–behavioral therapy (CBT) proved very effective in adolescents with JFM in a randomized clinical trial that demonstrated superior effects of CBT relative to nonspecific psychological support and education Citation[7]. CBT resulted in marked reductions in functional disability and depressive symptoms, and at postintervention follow-up, the study patients treated with CBT fell in the mild range of disability and were within the nonclinical range for depressive symptoms. However, unlike other studies in pediatric pain conditions characterized by localized pain – such as chronic headache or abdominal pain Citation[8] – CBT did not result in clinically significant reductions in pain symptoms for adolescents with JFM. Treatment of widespread pain symptoms, therefore, continues to be a challenge in adolescent patients with this painful musculoskeletal condition.
Physical exercise is routinely prescribed for patients with JFM and is recommended by the American Pain Society guidelines for management of fibromyalgia (FM) pain Citation[9]. The guidelines recommend moderately intense aerobic exercise and muscle strengthening exercises at least two-times a week. These recommendations are supported by a number of studies that demonstrate the benefits of exercise on the reduction of pain and fatigue, along with improved quality of life in adult FM. A recent meta-analytic review of aerobic exercise treatments in 35 randomized clinical trials (>2000 adult FM patients) concluded that significant pain reductions could be achieved with low-to-moderate intensity exercise with a frequency of two- to three-times per week Citation[10]. These authors also reported that continuation of exercise was associated with positive outcomes at long-term follow-up. In our research, we have found that the most vigorously active (actigraphy measured) JFM patients also demonstrated significantly lower clinical pain levels Citation[11]. Despite the strong evidence for the benefits of physical exercise, the majority of patients with FM, including adolescents with JFM, are very sedentary, with over 75% of adolescents spending less than 30 min per day in moderate or vigorous activity Citation[11]. Older adolescent girls (15–18 years old) were more sedentary compared with younger girls (11–14 years old), which indicates decreasing activity levels with age in JFM patients. The positive effects of exercise interventions for JFM/widespread musculoskeletal pain have been reported in one small-scale trial and from a clinical program focusing on intensive exercise Citation[12,13]. However, none of these protocols included CBT for training in psychological coping strategies combined with physical exercise, and it is unclear whether these gains were maintained over time (i.e., beyond completion of the active treatment phase). The typical experience in most pediatric rheumatology settings is that adherence to exercise is poor in patients with JFM when the adolescents are not in a strictly supervised program. The question then arises about how best to motivate adolescents to engage in and integrate physical exercise into their lifestyles so they can receive the beneficial effects of exercise and maintain these benefits through a lifetime of reduced pain and supported physical fitness.
One advantage to CBT as a self-management strategy is that treatment gains are maintained even 6 months after active treatment is completed Citation[7], which indicates that the CBT self-management program supports adolescent patients with internalizing these learned skills to maintain long-term benefit. If a readily available integrated treatment program could be designed to build on the benefits of CBT with specialized physical exercise training geared to the developmental level of JFM patients, it may be possible to achieve synergistic and more lasting positive outcomes. We have observed that JFM patients vary widely in their physical fitness, motor competence, tolerance for exercise and fear of pain flare-ups related to increased activity. Therefore, it would be essential to start by ensuring that adolescents with JFM develop the requisite psychological coping skills (provided through CBT techniques) and knowledge about basic movement fundamentals even before they are asked to increase participation in moderate–vigorous exercise. An excellent model for this type of specialized neuromuscular training can be found in the field of pediatric exercise science and sports medicine, where there already exists a substantial literature in injury prevention. Interestingly, to our knowledge, such models have thus far not been applied to the treatment of pain, although they are beginning to be explored in school-based physical activity programs.
With the increasing public health concern about reduced free-time physical activity among youths and its related health risks, there has been a call for promotion of physical fitness programs in schools Citation[14]. At the same time, participation in sports is highly valued by school-age children, and many of them enter into programs without sufficient preparation. For children who have been mostly sedentary, there is a risk of increased injury or overexertion when initiating exercise. This parallels the experience of young JFM patients who have never initiated or who have stopped recreational or competitive sports, and complain about pain flare-ups or excessive fatigue when they do exercise. It may be counterproductive, in such cases, to provide medical recommendations to increase exercise without focusing first on whether they have mastered the fundamentals of proper movement and exercise technique. Pediatric exercise scientists have long known that preparing children and adolescents for active play and sports is quite different from that for adults. For example, children tend to prefer short bursts of intense physical activity interspersed with periods of rest (similar to natural play), whereas adults may have a preference for longer, more graded programs of exercise. Therefore, exercise training geared towards youths with JFM should be designed with their developmental needs in mind. Prolonged periods of aerobic exercise or higher-volume resistance training will likely be discomforting for these patients and should therefore be avoided.
Myer et al. recently published a paper describing how age-appropriate integrative neuromuscular training can be effectively used to reduce sports-related injuries and enhance athletic performance in children and adolescents Citation[15]. These programs include specific training in posture, balance, gait and strengthening activities that ensure safe participation in sports for otherwise healthy children. These can be easily adapted for use in children with musculoskeletal pain who have a propensity for biomechanical deviations Citation[16] and need to be taught basic skills so they can more confidently initiate previously avoided activities, as demonstrated in a tailored neuromuscular program designed for a child with quiescent juvenile arthritis who wished to return to sports Citation[17]. In a similar fashion, exercises for JFM youths should focus on general (e.g., fundamental movements) and specific (e.g., exercises targeted at motor control deficits) activities, such as resistance, dynamic stability and core focused strength training. A specialized progressive and resistive protocol for JFM would ideally employ four phases:
| ▪ | Isometric exercises | ||||
| ▪ | Concentric (shortening) exercises | ||||
| ▪ | Eccentric (lengthening) exercises | ||||
| ▪ | Functional exercises | ||||
These should be designed specifically to reduce risk of muscle pain during exercise and soreness following exercise. In the case of JFM, it would be especially important to keep delayed-onset muscle soreness at a minimum so that pain flare-ups that mimic the symptoms of JFM can be avoided. Furthermore, the prescribed exercises, sets and repetitions for a JFM exercise program should be individualized and also modified as needed. A gradual and sensible progression of neuromuscular training based upon baseline fitness of JFM patients should be built into the program with sufficient variety to prevent boredom.
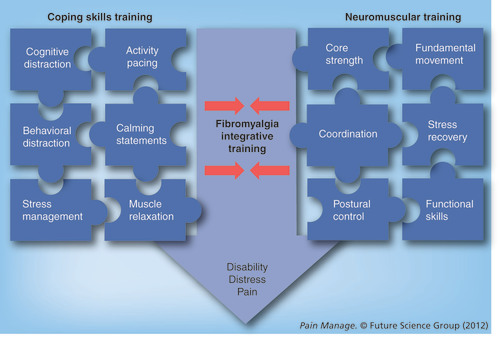
When adolescents with JFM engage in an integrative training program (see ) with both physical and psychological modalities, the combinatorial effects of coping skills training and improved preparation for exercise could provide a much more powerful behavioral/self-management approach than has been tried thus far. Although it has a strong intuitive appeal, this systematic approach to the development of a comprehensive program has never been rigorously tested to evaluate potential benefits compared with standard medical management approaches. If, in fact, it can be demonstrated that adolescents with JFM with a strong foundation of psychological and physical skills have greater confidence, lower disability and pain and improved quality of life, such an integrated program would be a key component for the successful long-term management of this disabling condition.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Kashikar-Zuck S , LynchAM, GrahamTB, SwainNF, MullenSM, NollRB. Social functioning and peer relationships of adolescents with juvenile fibromyalgia syndrome. Arthritis Rheum.57(3) , 474–480 (2007).
- Kashikar-Zuck S , LynchAM, SlaterS, GrahamTB, SwainNF, NollRB. Family factors, emotional functioning, and functional impairment in juvenile fibromyalgia syndrome. Arthrit. Rheumat.59(10) , 1392–1398 (2008).
- Kashikar-Zuck S , ParkinsIS, GrahamTB et al. Anxiety, mood, and behavioral disorders among pediatric patients with juvenile fibromyalgia syndrome. Clin. J. Pain 24(7) , 620–626 (2008).
- Kashikar-Zuck S , VaughtMH, GoldschneiderKR, GrahamTB, MillerJC. Depression, coping and functional disability in juvenile primary fibromyalgia syndrome. J. Pain3(5) , 412–419 (2002).
- Yunus MB , MasiAT. Juvenile primary fibromyalgia syndrome. A clinical study of thirty-three patients and matched normal controls. Arthrit. Rheumat.28(2) , 138–145 (1985).
- Kashikar-Zuck S , ParkinsIS, TingTV et al. Controlled follow-up study of physical and psychosocial functioning of adolescents with juvenile primary fibromyalgia syndrome. Rheumatology (Oxford) 49(11) , 2204–2209 (2010).
- Kashikar-Zuck S , TingTV, ArnoldLM et al. A randomized clinical trial of cognitive behavioral therapy for the treatment of juvenile fibromyalgia. Arthritis Rheum. doi:10.1002/art.30644 (2012) (Epub ahead of print).
- Palermo TM , EcclestonC, LewandowskiAS, WilliamsAC, MorleyS. Randomized controlled trials of psychological therapies for management of chronic pain in children and adolescents: an updated meta-analytic review. Pain148(3) , 387–397 (2010).
- American Pain Society. Guideline for the Management of Fibromyaglia Syndrome Pain in Adults and Children. American Pain Society, IL, USA (2005).
- Hauser W , KloseP, LanghorstJ et al. Efficacy of different types of aerobic exercise in fibromyalgia syndrome: a systematic review and meta-analysis of randomised controlled trials. Arthrit. Res. Ther. 12(3) , R79 (2010).
- Flowers SR , Kashikar-ZuckS, JohnsonM et al. Physical activity monitoring in children and adolescents with juvenile primary fibromyaglia syndrome. J. Pain 10(4) , S62 (2009).
- Sherry DD . Diagnosis and treatment of amplified musculoskeletal pain in children. Clin. Exp. Rheumatol.19(6) , 617–620 (2001).
- Stephens S , FeldmanBM, BradleyN et al. Feasibility and effectiveness of an aerobic exercise program in children with fibromyalgia: results of a randomized controlled pilot trial. Arthrit. Rheum. 59(10) , 1399–1406 (2008).
- Myer GD , FaigenbaumAD, FordKR, BestTM, BergeronMF, HewettTE. When to initiate integrative neuromuscular training to reduce sports-related injuries and enhance health in youth? Curr. Sports Med. Rep.10(3) , 155–166 (2011).
- Myer GD , FaigenbaumAD, ChuDA et al. Integrative training for children and adolescents: techniques and practices for reducing sports-related injuries and enhancing athletic performance. Phys. Sports Med. 39(1) , 74–84 (2011).
- Ford KR , MyerGD, MelsonPG, DarnellSC, BrunnerHI, HewettTE. Land–jump performance in patients with Juvenile idiopathic arthritis (JIA): a comparison to matched controls. Int. J. Rheumatol.2009 , 478526 (2009).
- Myer GD , BrunnerHI, MelsonPG, PaternoMV, FordKR, HewettTE. Specialized neuromuscular training to improve neuromuscular function and biomechanics in a patient with quiescent juvenile rheumatoid arthritis. Phys. Ther.85(8) , 791–802 (2005).