Abstract
Conclusion: The rate of severe complications was low and cochlear implantation is a relatively safe procedure. Standardization is crucial when reporting on cochlear implant complications to ensure comparability between studies. A consensus on the reporting of complications proposed by a Danish team of researchers was applied, evaluated and found beneficial. Objectives: To report the surgical complications following cochlear implantation at our centre, applying and evaluating a proposed reporting consensus. Methods: A retrospective file review of 308 consecutive adult implantations in 269 patients between 1994 and 2010 at Odense University Hospital was performed. Results: The three most common major complications were wound infection (1.6%), permanent chorda tympani syndrome (1.6%) and electrode migration/misplacement/accidental removal (1.3%). Permanent facial nerve paresis occurred following one implantation (0.3%). Transient chorda tympani syndrome (30.8%), vertigo/dizziness (29.5%) and tinnitus (4.9%) were the most frequent minor complications.
Keywords::
Introduction
Knowledge of the risks associated with cochlear implantation (CI) is important. It is a necessity for accurate preoperative information and a prerequisite for the patient to give informed consent. CI is a procedure that increases the quality of life [Citation1], but it is not life-saving, and comparison of the advantages and risks associated with implantation is important.
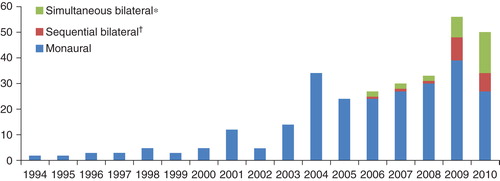
The annual numbers of implantations performed at our centre (), as well as at other Danish [Citation2,3] and international centres [Citation4] are rising. Currently more than 70 adults are implanted each year at Odense University Hospital (OUH), and as of December 2010, approximately 219 000 people worldwide had received a cochlear implant [Citation5]. Moreover, sequential and simultaneous bilateral implantations are becoming more frequent in many centres including ours (), and knowledge of possible complications related to bilateral implantation is necessary.
Figure 1. Annual numbers of cochlear implantations (CIs). *A simultaneous bilateral implantation accounts for two implantations. †Sequential bilateral covers implantations where the first CI was also performed at our centre.
Retrospective file reviews are often used for investigating the possible complications related to CI [Citation2]. It is an easy and inexpensive method for evaluating various complications at the same time. However, different classifications and methods of registration have been applied. Therefore direct comparison of study results is often not possible and differences in complication rates can at least in part be attributed to differences in method. An international reporting consensus is called for.
The aim of this study was to report the frequency of surgical complications following 308 consecutive CIs in adults at Odense University Hospital. The international consensus on the reporting of cochlear implant complications proposed by Hansen et al. [Citation2] was used and evaluated.
Material and methods
Material
The medical records of consecutive adult patients undergoing implantation between April 1994 and December 2010 at our centre were examined retrospectively. All available files from the Departments of Otorhinolaryngology and Audiology at Odense University Hospital, both pre- and postoperative, were examined. If a patient's postoperative follow-up examinations were not performed at our hospital, the medical records were accessed using the E-journal (an electronic system that grants access to patient medical records at other Danish hospitals). If not available through the E-journal, the given hospital was contacted, and the medical records were sent in writing. Hence all implanted patients were eligible for complete follow-up.
Patients were generally discharged the day after surgery. If complications had developed, they stayed in hospital until the problem was either resolved or discharge was considered safe. Patients were instructed to contact the department in case of complications following discharge (e.g. signs of infection, severe vertigo, etc.). Regular follow-up examinations at the Department of Otorhinolaryngology were not scheduled.
Approximately 1 month after surgery the patients had the external part of the cochlear implant attached at the Department of Audiology. Regular follow-up examinations performed by a doctor at the department of audiology and adjustments by an assistant audiologist were typically scheduled 1, 6 and 12 months later. Subsequently patients were offered further follow-up examinations on request. Otomicroscopy, audiometric testing, vestibular testing, auditory brainstem response (ABR), medical history and computed tomography (CT) or magnetic resonance imaging (MRI) of the temporal bone were included in the preoperative evaluation of candidacy for cochlear implant surgery in all patients.
Methods
The medical records were examined for complications arising between April 1994 and 1 January 2012. Implantations performed after 31 December 2010 were not included in the study, as a time frame of 1 year after implantation was considered the minimum to allow for complications to arise. As a rule, paediatric patients (defined as under the age of 15) are not operated at our centre and were not included in the study.
A surgical complication was defined as an unexpected medical event related to the procedure itself and causing additional morbidity (e.g. vertigo or infection) or a need for additional surgery (e.g. electrode migration) [Citation2].
The surgical complications were characterized as major or minor. A major complication was defined as: (1) a significant medical problem (e.g. meningitis); (2) an event leading to additional major surgery due to a patient-related problem (e.g. cholesteatoma or explantation of the device for any other reason than device-related failure); (3) any degree of permanent disability (e.g. permanent facial nerve paresis).
Any complication not falling into at least one of the above-mentioned categories was classified as minor (for further details on the classification of minor complications see Hansen et al. [Citation2]). The following were not classified as surgical complications: (1) medical complications (e.g. allergic reactions, drug adverse effects); (2) technical complications (e.g. facial stimulation, device failure); (3) conditions existing preoperatively (e.g. recurrent otitis media); (4) intra- and preoperative findings (e.g. abnormal anatomy, middle ear/cochlear fibrosis).
All registered complications were divided into three categories according to time of onset: (1) perioperative (occurring during or within 24 h after surgery); (2) early postoperative (occurring between 24 h and 1 week after surgery); (3) late postoperative (occurring later than 1 week after surgery).
The dates of any patient deaths and/or re-implantations were registered, and the length of follow-up was calculated as the time elapsing from implantation until re-implantation, death or the end of the study period.
Complications were sorted according to time of onset, major/minor and type of implantation that had caused them (monaural, simultaneous bilateral or re-implantation). Complication rates were calculated as proportions of the total number of implantations. In case of doubt as to whether an incident was caused by the procedure, we reported it as a complication. Changes in preoperatively existing conditions (e.g. tinnitus and vertigo), although highly relevant, were not reported, as the method of retrospective file review was not considered suitable for this.
Results
In all, 308 implantations were performed in 269 adult patients: 273 monaural or sequential, 30 simultaneous bilateral (15 patients) and 5 re-implantations. The median age at implantation was 52 years (range 16–85 years). The median length of follow-up was 60 months (range 0.39–213 months). The annual numbers of implantations at our centre are shown in . Hearing loss aetiology and the implant systems used are presented in and , respectively. Five different surgeons performed 140 (45.5%), 107 (34.7%), 30 (9.7%), 2 (0.7%) and 1 (0.3%) implantations each, and 28 implantations were performed in collaboration between surgeons. In 22 (7.1%) implantations, the patient had previously had surgery on the operated ear.
Table I. Reasons for loss of hearing.
Table II. Cochlear implant systems used.
The surgical procedure included a mastoidectomy and a posterior tympanotomy. In four cases, however, the cochlea could not be adequately accessed through a posterior tympanotomy, and a cochleostomy was performed through the ear canal. Patients with a radical cavity usually had a subtotal petrosectomy performed before CI. Full insertion was achieved in 292 of the implantations. In the remaining 16 implantations, the surgeon could not insert all electrodes into the cochlea (median number of electrodes outside the cochlea was 3, range 1–15).
Fourteen (4.5%) of the 308 implants were later explanted for various reasons described in the following. Three were in accordance with the European Consensus Statement on Cochlear Implant Failures and Explantations (ECSCIFE) [Citation6] classified as C(Device failure) and 11 as D(Medical reason).
Surgical complications
A total of 168 (62.5%) of the 269 patients experienced at least 1 surgical complication; 23 (8.6%) patients experienced at least 1 major complication and 159 (59%) patients experienced at least 1 minor complication. Complication numbers are presented in and complication rates in . Preoperative CT/MR imaging of the cochlea was normal unless otherwise stated in the relevant sections.
Table III. Occurrence of surgical complications.
Table IV. Complication rates.
Minor complications
Wound infections
Minor infections developed a median of 28 days (range 3–358) after implantation. These comprised superficial as well as more extensive infections. All resolved following treatment with different combinations of topically administered substances and oral and intravenous antibiotics.
Labyrinthitis/vestibular neuritis
Three patients were diagnosed with labyrinthitis/vestibular neuritis at 1, 2 and 34 months after implantation. It was not possible to discern the two conditions from the file data. All three patients recovered spontaneously.
Transient facial nerve paresis
One patient developed paresis on the operated side immediately after surgery, primarily involving the inferior branches of the facial nerve. Two developed mild pareses a few days after implantation. Late postoperative paresis occurred in four patients between 9 and 20 days after implantation. Three of these were treated with prednisolone, two in combination with antibiotics. The facial nerve was not abnormally located or exposed in any of the seven patients, nor did any of them show signs of infection. Complete resolution was seen in all patients.
Ear canal fenestration
The posterior wall of the external auditory meatus was accidently fenestrated in eight patients during drilling of the posterior tympanotomy. One of these was accompanied by a tympanic membrane perforation (described below). The fenestrations were repaired using muscle, fascia or cartilage taken from the tragus.
The fenestrations healed well without complications. None of these patients developed cholesteatomas during the observation period.
Eardrum perforation
Three patients had iatrogenic eardrum perforations, of which two were repaired during surgery using temporalis fascia placed as an underlay graft. One of the patients had been implanted through the ear canal. All three healed during the following 1–2 months.
Tinnitus
The patients were routinely asked about tinnitus at the preliminary medical examinations and at follow-up. Only tinnitus not present preoperatively was regarded as a complication.
Complaints of tinnitus arose after 15 implantations. One was a simultaneous bilateral implantation, but as tinnitus was only registered in the right ear, it was considered a complication of this implantation only. All cases were intermittent and categorized as minor.
Transient vertigo/dizziness
Cochlear implant recipients were routinely asked about vertigo/dizziness before and after surgery. Only cases where vertigo was not present preoperatively were regarded as having a complication. Vertigo following simultaneous bilateral implantation was considered a complication to only one of the implantations.
Dizziness started within 24 h after surgery in 59.3% of the patients who complained of this, and in 27.5% it started within a week. The remaining 13.2% complained of dizziness at the follow-up visit 1 month after surgery, and the exact onset of dizziness for these patients could not be determined from the medical records.
The duration of dizziness ranged from 1 day to 2 months.
Transient chorda tympani syndrome
This syndrome was defined as changes in sense of taste, mouth dryness or tongue paresthesia [Citation7,8] that developed postoperatively. The classification of chemosensory disorders described by Schiffmann et al. [Citation9] was used.
Transient complaints were reported subsequent to 83 unilateral implantations (82 patients as 1 was a sequential bilateral implantation) and 9 simultaneous bilateral implantations (18 implantations). Three of the latter patients had bilateral complaints and were thus counted as having two complications.
An altered sense of taste occurred either in the form of hypogeusia (n = 22), dysgeusia (n = 21, in the form of taste hallucinations), both (n = 6) or were unspecified (n = 40). Patients with dysgeusia discriminated between the following taste perceptions: metallic (n = 18), sweet (n = 5), salty (n = 2), bitter (n = 1) and sour (n = 1). One case of dysgeusia was described as tactile (dysgeusia happened upon touching of the cicatrice) [Citation10]. Complaints of altered taste in 10 patients were accompanied by paresthesia of the tongue and in two of the bilaterally implanted patients by mouth dryness. In six cases tongue paresthesia alone was present.
The surgeon reported severing of or other damage to the chorda tympani nerve in eight implantations resulting in chorda tympani syndrome and another eight implantations that were unaccompanied by symptoms.
Major complications
Cholesteatoma
One patient experienced secretion and a sensation of pressure in the ear 4.5 years after implantation. A cholesteatoma was detected. The patient underwent surgical removal of the cholesteatoma, without removal of or damage to the implant. At 43 years before implantation the patient had already suffered from cholesteatoma in the same ear and been surgically treated. However, implantation could not be ruled out as the cause of the new cholesteatoma.
Another patient was implanted through the ear canal, as satisfactory access could not be achieved through the posterior tympanotomy. Two months later she was explanted due to electrode misplacement in the vestibule, and re-implanted in the same procedure. The patient later developed a cholesteatoma in the mastoid and epitympanum, surrounding the misplaced electrode originating from the primary cochlear implant, which had not been removed. The cholesteatoma as well as the implant, which had not been useful to the patient, were removed 4 years after the re-implantation.
Both cases have so far been without recurrence.
Electrode migration/misplacement/accidental removal
In two patients postoperative CT confirmed electrode placement in the vestibule, and in another two patients the electrodes were displaced to the middle ear. During all four implantations, the surgeon evaluated the electrodes as fully inserted. In one of the two latter patients, the electrode had not with certainty migrated out of the cochlea. It had gone through the posterior wall of the ear canal though, and was accidentally removed during an otoscopy performed by the patient's own otologist. All four were explanted and re-implanted in the same procedure. Preoperative CT was abnormal in one of the patients (cochlear fibrosis and decreased fluid signal in the basal turn).
Magnet displacement
The internal magnet of a Nucleus CI24R(CA) implant was displaced following MRI in one patient. The displaced magnet was returned in place simultaneously with a sequential bilateral CI.
Permanent facial nerve paresis
A 44-year-old woman developed facial nerve palsy on the operated side 4 days after surgery. It involved all three branches of the facial nerve, and was rated as House-Brackmann grade III palsy. The middle ear was found to be normal during surgery and the facial nerve was not reported as injured by the drill or otherwise. The patient was treated with 25 mg prednisolone twice a day for 10 days, and the facial function improved. At 2 years and 8 months later the woman still suffered from a mild paresis of the nerve, and it was considered permanent.
Wound infection
Major infections supervened between 4 and 38 months after implantation. Four were considered abscesses and one a phlegmonous infection. One infection was treated successfully (resolution occurred following revision surgery using Gentacoll® and intravenous cefuroxime). The remaining four implants were ultimately explanted. Two of the patients were later implanted on the other ear, the other two were re-implanted on the same ear. None of the patients experienced new infections.
Permanent vertigo/dizziness
New-onset vertigo/dizziness following implantation present for at least 1 year was considered permanent.
This was found in four patients who all started feeling dizzy on the day of or the day after surgery and still had complaints after a minimum of 4 years follow-up. Treatment included vestibular rehabilitation exercises.
Permanent chorda tympani syndrome
Permanent chorda tympani syndrome (present more than 1 year after surgery) occurred following five implantations. These patients complained of an altered sense of taste. Two experienced hypogeusia, two dysgeusia (salty taste) and one a combination, with the dysgeusia experienced as metallic taste. In one patient dysgeusia was accompanied by numbness of the operated side of the tongue and severe mouth dryness. One patient lost the ability to season food, whereas another always had to carry a bottle of water due to severe dryness of the mouth. The surgeon did not report the tympanic chord severed or damaged in any of the five permanent cases.
Persistent pain/discomfort
Pain and discomfort in association with anterior displacement of a 54-year-old woman's receiver/stimulator occurred 2 years after implantation. The symptoms led the woman to refrain from using her implant. The receiver/stimulator was replaced in a new well and her pain and discomfort subsided. Due to severe postauricular pain two other CIs were explanted at the request of the patients, and the symptoms vanished.
Technical complications
Approximately seven (data might be slightly inaccurate) patients showed signs of non-auditory stimulation following attachment of the external part of the implant (six cases of facial tics and one of ringing in the ear and headache). In three of these not all electrodes could be inserted during implantation (three, four and eight electrodes outside the cochlea, respectively). In four cases the symptoms were alleviated by adjustment of the stimulation profile (e.g. switching off one or more electrodes). In two the symptoms resolved spontaneously. In one patient the symptoms could not be alleviated and the patient stopped using the implant.
In two patients that were simultaneously bilaterally implanted, one implant, a MED-EL SONATA TI-100 and a Nucleus CI24RE(CA), ceased functioning after 5 and 47 months, respectively. In a monaurally implanted patient the implant, a Nucleus CI24RE(CA), failed 13 months after implantation. Technical examinations showed device failure. All three were explanted and re-implanted in the same procedure.
Discussion
This is to our knowledge the first study to use the consensus on cochlear implant complications proposed by Hansen et al. [Citation2] besides the authors. Complications following CI at Odense University Hospital were frequent, with more than half of the implantations (57.1%) being accompanied by at least one surgical complication (62.5% of the patients). However, the majority of these complications were minor and self-resolving. Major complications were observed following 24 implantations only (7.8%) and we therefore consider CI to be a safe procedure. In all, 4.5% (n = 14) of the cochlear implants implanted at our centre were later explanted for various reasons.
The minor complication rates found in the present study were generally similar to the adult complication rates found by Hansen et al., who studied complication rates after CI at Gentofte University Hospital Copenhagen (GUHC) [Citation2]. The differences in complication rates for eardrum perforations, ear canal fenestrations, transient facial nerve pareses and vestibular neuritis/labyrinthitis did not exceed 3 percentage points. For transient vertigo/dizziness the complication rate at OUH was higher than at GUHC (the rates were 29.6% and 25.0% at OUH and GUHC, respectively). In another retrospective study 34.7% of the patients reported subjective episodes of vertigo soon after implantation [Citation11], whereas 21.3% of patients reported new onset vertigo in a study by Fina et al. [Citation12]. The rate of transient facial nerve paresis was 0.71% in a combined group of children and adults in a retrospective study by Fayad et al. [Citation13]. Although we found a complication rate of 2.3%, we consider both rates low and paresis of the nerve a relatively uncommon complication. Thus, for all the above-mentioned complications, our findings corresponded well with those found in other studies.
The rates of transient chorda tympani syndrome were 30.8% and 5.7% at OUH and CUHG, respectively. It is mentioned by Hansen et al. [Citation2] that their rate was probably an underestimation, as taste changes were not addressed routinely in their study, and we consider this to be the most plausible explanation for the considerable difference. Further, only incidents including taste changes (not cases of tongue paresthesia or xerostomia alone) were reported in the latter study [Citation2]. Other studies in the field have reported subjective changes in the sense of taste in up to 45% of the implanted patients [Citation14]. It should be noted that 60% of the simultaneous bilateral implantations, compared with 31.7% of other implantations, were accompanied by chorda tympani syndrome in the present study. Bilateral implantations are thus associated with a doubled risk, which should be remembered in preoperative information. Additionally the syndrome may be more severe than in unilateral implantation, which should be investigated in prospective studies.
Tinnitus was not reported by Hansen et al. [Citation2], as the file data were considered inadequate. A prospective multicentre study [Citation15] reported the complication rate of newly developed tinnitus to be 10.2% (5 cases in 49 implantations). This is more than twice the rate found in our study (4.9%). The difference might be explained by a lack of addressing this issue during postoperative follow-up in the present study.
The discrepancy between the complication rates of minor wound infections at GUHC and OUH (8.85% vs 3.57%) may at least in part be explained by some infections at OUH turning into major complications, whereas all were successfully treated with intravenous antibiotics at GUHC.
The major complication rates found in the two studies were highly similar regarding permanent facial nerve pareses and electrode migration/misplacement/accidental removal. None of the remaining major complications found in the present study were observed at GUHC though. This difference may be explained by the symptoms not being routinely addressed at GUHC during postoperative visits at the outpatient clinic [Citation2], the shorter follow-up time (36 months vs 60 months) and a lack of a minimum length of follow-up (1 year in the present study).
In other studies [Citation16,17] the remaining major complications were observed as well.
We found no cases of excessive/sustained bleeding, electrode kinking, dural tear, flap necrosis, mastoiditis, meningitis or death related to implantation.
Direct comparison of rates between studies is difficult because of methodological differences. Variations in the existing literature include the following.
Complications included (e.g. some studies report obviously related complications like vertigo [Citation2] and some do not [Citation4]). Others include non-auditory stimulation [Citation4], device failures [Citation16] and facial nerve exposure [Citation18], although these are clearly technical problems and perioperative findings.
Definitions of a surgical complication. (For example, some studies fail to define what they consider a surgical complication. Furthermore different definitions are used.)
Definitions of major and minor complications (e.g. some define these terms [Citation2], others do not [Citation3]). Some consider a permanent disability major opposed to others.
Definitions of a complication rate (e.g. some calculate rates as proportions of the total number of implantations [Citation2], whereas others use the total number of patients implanted).
Populations used (e.g. some calculate complication rates for children and adults separately [Citation2], others do not [Citation19], although variability has been documented in the literature between these two groups [Citation2]).
Methods of following up (some describe the postoperative follow-up procedure, e.g. number of scheduled follow-up visits [Citation16], at which departments they were carried out, etc., whereas others do not [Citation2]).
Reporting of the surgical approach is not reported in all studies [Citation2], although studies have found different complication rates depending on the surgical approach [Citation20].
The different approaches used are especially problematic when pooled overall, minor and major complication rates are calculated and compared as if they express equal information. Further it is the separate complication rates that should be the basis of patient information, not the pooled rates. The purpose of calculating pooled rates can thus be questioned, and we decided not to present pooled rates in this paper.
The proposal of a reporting consensus by Hansen et al. [Citation2] is to our knowledge the first of its kind, although single suggestions for reporting have been mentioned in other studies. The proposed consensus was employed in our study and we found it easily applicable and with a logical construction. However, we did encounter some minor problems in the proposed consensus that would benefit from further elaboration: (i) the question of when a disability should be considered permanent (we used presence > 1 year); (ii) clarity on how to categorize if there is doubt about the temporal occurrence of complications (in the present study we used the time of reporting if the time of occurrence could not be established). As a rule cases of doubt should be described.
We endorse the notion that an international reporting consensus on cochlear implant complications should be established and recommend that it is based on the proposal presented by Hansen et al. [Citation2]. Further we present added suggestions for the reporting consensus as they appear in . We consider these items important because surgical approach and length of follow-up are associated with the complication rate. Further we assume the symptoms addressed during follow-up and the type of medical records reviewed to be related to the complication rates (e.g., most cases of chorda tympani syndrome were reported at follow-up examinations at the Department of Audiology in our setting, hence a review of otorhinolaryngologic medical records only would have seriously underestimated this complication).
Table V. A proposal for the reporting of surgical complications in cochlear implantations.
Further, we suggest a preset lower limit in the length of follow-up to be necessary, as studies including implantations performed right up to the start of a review will underestimate complication rates. This problem is not solved completely by applying a lower limit (ideally all patients should undergo lifelong follow-up), but as most complications develop within the first year after implantation, we assume this will greatly reduce the underestimation of the complication rates.
Moreover, like the pooling and analysis of children and adults as one material obscures potential variability related to age [Citation2], the pooling of unilateral, simultaneous bilateral and re-implantations obscures potential variability related to the type of implantation. However, the small numbers of re-implantations and simultaneous bilateral implantations in our study preclude meaningful separate statistical analysis of these groups.
Further research is warranted, especially regarding chorda tympani syndrome, vertigo and tinnitus, as these complications are possibly more severe in case of bilateral surgery. Especially vertigo has been somewhat investigated, and there is slight evidence of an increased risk of symptoms associated with bilateral implantation. However, these findings are based on small populations and prospective studies with long-term follow-up are essential, to clarify the risk and severity of bilateral damage to the vestibular system. Furthermore, the value and relevance of preoperative vestibular testing is highly debated, as poor correlation between preoperative vestibular hypofunction and postoperative symptoms has been described.
Finally, we recommend that complication rates should be calculated as proportions of the total number of implantations, not the number of patients. Calculations based on patient numbers do not take bilateral implantations and re-implantations into account, thus compromising comparability. Furthermore relevant preoperative information should provide patients with knowledge of the risks associated with the impending procedure, making calculations per implantation the clinically relevant measure.
We now consider the strengths and limitations of the present study. A retrospective file review is associated with inherent imprecision, as all complications are not necessarily addressed routinely in the outpatient follow-up after surgery. At our centre chorda tympani syndrome, vertigo/dizziness and tinnitus were generally addressed, but the minor complications in particular may have been underestimated, and this is a possible bias in our study. Further, this might explain why some of the previously mentioned prospective studies found slightly higher rates. Especially in bilateral implantations, subjective complaints are difficult to evaluate, as there can be doubt about the side of implantation causing the symptoms, or even both implantations being the cause. Major complications (e.g. the ones leading to explantation) are presumably registered more consistently, and as a result not subject to the same variation as the minor complications. Further some of the registered data (e.g. cause of deafness) are to a certain degree based on self-reported patient experiences (e.g. meningitis in childhood) and might be subject to misclassification errors.
Even using the same consensus, inter-observer variation is never avoided in retrospective file reviews. It exists between doctors examining and questioning the patients, and between the researchers reviewing the files. This might contribute to some of the variation found between different studies. At best this is avoided through controlled prospective studies, as they can be used to investigate causality. This is not an argument for avoiding retrospective file reviews, nor is it a reason to stop pursuing consensus, as researchers should always strive for uniform reporting.
Conclusion
CI is generally considered a safe procedure, which was confirmed in our study. However, the use of different definitions and reporting criteria has obscured the overview necessary for satisfactory comparison between studies and preparation of adequate patient information. An international consensus on the reporting of CI complications is warranted.
Acknowledgments
The study was financially supported by the Oticon Foundation, the Danish Association of the Hard of Hearing (Ingeborg & Emanuel Jensens Legat), the Board of Clinical Directors at OUH (Else Poulsens Minde Legat) and the Danish Association of Otolaryngology, Head and Neck Surgery (Poul Traun-Pedersens Mindelegat).
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the study design; collection, analysis and interpretation of data; content and writing of the paper; and the decision to submit the report for publication. The retrospective file review was performed by the first author, who is not one of the surgeons at our centre, to ensure that no surgeon decided which incidences were classified as complications.
References
- Wanscher JH, Faber CE, Grontved AM. [Cochlear implantation in deaf adults: effect on quality of life]. Ugeskr Laeger 2006;168:2656–9; in Danish.
- Hansen S, Anthonsen K, Stangerup SE, Jensen JH, Thomsen J, Caye-Thomasen P. Unexpected findings and surgical complications in 505 consecutive cochlear implantations: a proposal for reporting consensus. Acta Otolaryngol 2010;130:540–9.
- Ovesen T, Johansen LV. Post-operative problems and complications in 313 consecutive cochlear implantations. J Laryngol Otol 2009;123:492–6.
- Arnoldner C, Baumgartner WD, Gstoettner W, Hamzavi J. Surgical considerations in cochlear implantation in children and adults: a review of 342 cases in Vienna. Acta Otolaryngol 2005;125:228–34.
- Disorders NIoDaOC. NIDCD Fact Sheet: Cochlear Implants. 2011. cited 10 August 2012 Available from http://www.nidcd.nih.gov.
- European consensus statement on cochlear implant failures and explantations. Otol Neurotol 2005;26:1097–9.
- McManus LJ, Dawes PJ, Stringer MD. Clinical anatomy of the chorda tympani: a systematic review. J Laryngol Otol 2011;125:1101–8.
- Perez R, Fuoco G, Dorion JM, Ho PH, Chen JM. Does the chorda tympani nerve confer general sensation from the tongue? Otolaryngol Head Neck Surg 2006;135:368–73.
- Schiffman SS, Gatlin CA. Clinical physiology of taste and smell. Annu Rev Nutr 1993;13:405–36.
- Chen JM, Bodmer D, Khetani JD, Lin VV. Tactile dysgeusia: a new clinical observation of middle ear and skull base surgery. Laryngoscope 2008;118:99–103.
- Filipo R, Patrizi M, La Gamma R, D'Elia C, La Rosa G, Barbara M. Vestibular impairment and cochlear implantation. Acta Otolaryngol 2006;126:1266–74.
- Fina M, Skinner M, Goebel JA, Piccirillo JF, Neely JG, Black O. Vestibular dysfunction after cochlear implantation. Otol Neurotol 2003;24:234–42; discussion 242.
- Fayad JN, Wanna GB, Micheletto JN, Parisier SC. Facial nerve paralysis following cochlear implant surgery. Laryngoscope 2003;113:1344–6.
- Lloyd S, Meerton L, Di Cuffa R, Lavy J, Graham J. Taste change following cochlear implantation. Cochlear Implants Int 2007;8:203–10.
- Kompis M, Pelizzone M, Dillier N, Allum J, DeMin N, Senn P. Tinnitus before and 6 months after cochlear implantation. Audiol Neurootol 2012;17:161–8.
- Venail F, Sicard M, Piron JP, Levi A, Artieres F, Uziel A, et al. Reliability and complications of 500 consecutive cochlear implantations. Arch Otolaryngol Head Neck Surg 2008;134:1276–81.
- Trotter MI, Backhouse S, Wagstaff S, Hollow R, Briggs RJ. Classification of cochlear implant failures and explantation: the Melbourne experience, 1982-2006. Cochlear Implants Int 2009;10:105–10.
- Hou JH, Zhao SP, Ning F, Rao SQ, Han DY. Postoperative complications in patients with cochlear implants and impacts of nursing intervention. Acta Otolaryngol 2010;130:687–95.
- Ding X, Tian H, Wang W, Zhang D. Cochlear implantation in China: review of 1,237 cases with an emphasis on complications. ORL J Otorhinolaryngol Relat Spec 2009;71:192–5.
- Migirov L, Yakirevitch A, Kronenberg J. Surgical and medical complications following cochlear implantation: comparison of two surgical approaches. ORL J Otorhinolaryngol Relat Spec 2006;68:213–19.