Abstract
Conclusion: The new mattress and pillow for prone positioning (MPP) is efficient in reducing the apnoea-hypopnoea index (AHI) and oxygen desaturation index (ODI) in most patients with obstructive sleep apnoea (OSA), with satisfactory compliance. Objective: The aim of the present study was to evaluate the effect of the prone body and head sleep position on severity of disease in patients with OSA after 4 weeks of adaptation to a mattress and pillow facilitating prone positioning. Methods: Fourteen patients with mild to severe OSA, 11 men and 3 women with a mean AHI of 26 (min, 6; max, 53) and mean ODI of 21 (min, 6; max, 51) were evaluated. Two polysomnographic (PSG) studies were performed. The first PSG study was without any treatment and the second was after 4 weeks of adaptation to the MPP for prone positioning of the body and the head. Results: Mean AHI and ODI decreased from 26 and 21 to 8 and 7, respectively (p < 0.001) with treatment. The mean time spent in the supine position was reduced from 128 to 10 min (p = 0.02) and the prone time increased from 42 to 174 min (p = 0.02) with the MPP. The mean total sleep time was 390 min during the first PSG study night without treatment and 370 min during the second night with the MPP (p = 0.7). Ten patients (71%) reduced their AHI by at least 50% and reached a value < 10 during treatment. All patients managed to sleep on the MPP for > 4 h per night during the 4-week study.
Introduction
The number and duration of respiratory disturbances during sleep are influenced by the body position in most patients with obstructive sleep apnoea (OSA) [Citation1]. More than 50% of patients with OSA are considered to have positional OSA (POSA), a condition in which the apnoea-hypopnoea index (AHI) is at least twice as high in the supine position compared with non-supine positions [Citation2,3]. In approximately 80% of all patients with OSA the AHI is higher in the supine position compared with the non-supine positions [Citation2,3].
Many patients with OSA cannot tolerate continuous positive airway pressure (CPAP) or they use it incidentally [Citation4,5]. Many patients with OSA have contraindications for using oral devices [Citation6]. Previous positional therapies for patients with OSA have focused primarily on avoiding the supine position and/or sleeping in the lateral position [Citation3,7,8].
One of the first described therapies to reduce snoring and to improve OSA was the so-called ‘tennis ball technique’. A tennis ball is sewn into the pyjamas or fastened by a belt to the back of the patient to reduce the time spent in the supine position [Citation9]. This treatment has been shown to reduce the supine time and to improve AHI in patients with POSA [Citation9,10]. Due to the limited compliance with all the variations of the tennis ball technique, several newer positional methods have been developed primarily to reduce the time spent in the supine position [Citation7,11,12].
There is limited experience regarding the effect of the prone position on severity of OSA [Citation13]. In a previous study from our research group [Citation14], the effect of prone positioning of the body and the head was evaluated in patients with OSA. The mean AHI and ODI were significantly improved in the prone position, with higher efficiency observed in patients with POSA. The long-term efficiency and the compliance of prone positioning were not assessed.
The aim of the present study was to evaluate the effect of the prone body and head sleep position on severity of disease in patients with OSA after 4 weeks of adaptation to a mattress and pillow facilitating prone positioning.
Material and methods
Study design and subjects
The patients included were referred to the Department of Otorhinolaryngology, Sahlgrenska University Hospital in Gothenburg, Sweden, due to sleep-disordered breathing. We recruited 15 patients with mild to severe OSA [Citation15]. Five patients were treated with CPAP and one with an oral device at baseline. All patients underwent two ambulatory polysomnographic (PSG) studies. The first of these studies was without any treatment and the second was with a mattress and pillow for prone positioning (MPP) after 4 weeks of adaptation to the treatment at home.
Exclusion criteria were neurologic disease that might influence the muscle tonus, heart failure, uncontrolled high blood pressure, body mass index (BMI) > 40, age < 18 years and pregnancy. All patients gave written informed consent to participate in the study. The patients were enrolled from December 2012 to April 2013.
The study was approved by the Local Medical Ethics Committee for Clinical Trials, 2011/131-11. All patients gave written informed consent to participate in the study.
Mattress and pillow for prone positioning
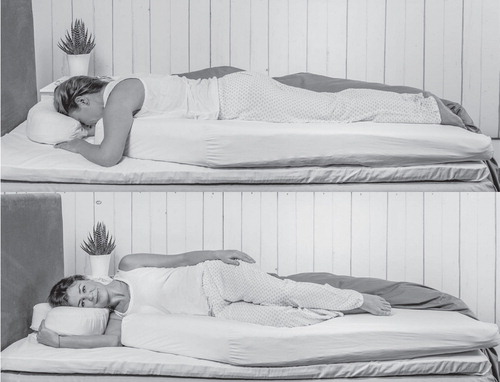
The MPP model from the previous study [Citation14] was used to facilitate prone positioning during sleep. The MPP consisted of a combination of visco-elastic (memory) and normal foam ().
Figure 1. The mattress and pillow for prone positioning (MPP) of the body and the head with the nose mostly perpendicular to the underlying bed.
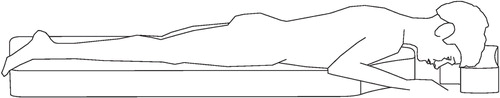
A T-shaped pillow, with a height of 12 cm and a width of 40 cm, enabled cheek and forehead support with a relatively well aerated space for breathing, allowing for a prone head position. A mattress with a height of 12 cm, width of 80 cm and length of 120 cm was provided to ensure a comfortable and stable prone body position during sleep. At the upper end the mattress had excavations of the sides for positioning of the arms and anatomical angles in the shoulders and elbows. The support of the chin on the mattress was optional ().
The MPP could be placed upon a normal mattress and hence would be compatible with the existing bed at home. The main purpose of the MPP was to provide a comfortable prone sleep position. After lying on the MPP, the temperature-sensitive visco-elastic material moulded to the body shape, which helped the subject maintain the prone position during the night. Although lateral positioning would be possible, supine positioning was difficult ().
Sleep recordings
Ambulatory PSG equipment was used (Embla, Flaga Medical, Reykjavik, Iceland). The sleep studies included registration of breathing efforts by chest and abdominal movements, airflow and snoring by oronasal flowmetry and thermistor, and body position by a position sensor that could differentiate between upright, supine, left, right and prone positions. Heart rate and oxygen saturation were registered by a finger pulse-oximeter. Electroencephalography (EEG) monitoring (sensors C3-A2, O1-A2, O2-A1, C4-A1 derivations), electro-oculogram (left and right) and submental electromyogram (EMG) were recorded.
Data interpretation
The sleep studies were analyzed and scored by an independent technician blinded to the assignment of the patients. Sleep efficiency, sleep stages and arousals were scored according to the criteria proposed by the American Association of Sleep Medicine (AASM) [Citation15].
The total number of apnoeas and hypopnoeas was divided by the sleep time, giving the AHI. The oxygen desaturation index (ODI) was calculated in the same manner based on the total number of desaturations divided by the sleep time. The respiratory parameters, sleep time and the time slept in the supine, lateral and prone positions were compared for each patient without and with the MPP.
Compliance/side effects
Inspired by the CPAP definition of compliance [Citation4], patients with a sleep time < 4 h per night with the MPP were considered non-compliant to the treatment. An instruction video was provided for correct positioning on the MPP and a sleep diary was implemented for registration of compliance and side effects during treatment. The Epworth Sleepiness Scale (ESS) was used for the evaluation of daytime sleepiness before and after treatment [Citation16].
Statistical analysis
A power analysis was conducted to estimate the appropriate sample size, using the results from the previous study [Citation14]. To achieve the observed AHI improvement of 19 in the previous study, at a confidence level of 95% and a power level of 90%, with an SD in change score of 13, in a two-sided test, the sample size would be 8. In view of a higher expected failure rate at follow-up and to allow for exclusions and drop-outs, as well as obtaining more exact estimates, a target sample of 15 subjects was set.
Statistical analysis was performed using Stata version 13 (StataCorp. 2013, College Station, TX, USA). Quantitative data are reported as mean (min, max) in the text and median in the figures. Comparison of data between the baseline (without treatment) and with treatment was carried out using the paired t test in the case of normally distributed data and the Wilcoxon matched pairs sign-rank test in the case of skewed data. McNemar’s test was used to assess paired proportions. All statistical tests were two-tailed and conducted at 5% significance level.
Results
All 15 patients fulfilled the study protocol and slept on the MPP during 4 weeks. One patient was excluded from the present results due to failure in registration of oxygen saturation during the first PSG study. The characteristics of the 14 eligible participants are summarized in . According to the first PSG study, 9 of 14 patients (64%) had POSA.
Table I. The characteristics of the 14 eligible patients.
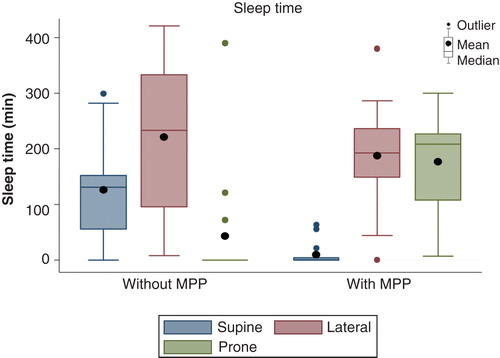
Sleep time
The mean total sleep times during the first PSG study night without treatment and the second night after 4 weeks of adaptation to the MPP were, respectively, 390 (min, 238; max, 537) and 370 min (min, 260; max, 502) (p = 0.7). The mean sleep efficiency was 79% during the first night and 74% during the second night (p = 0.4).
Without treatment the mean times spent in the supine and lateral positions were, respectively, 128 min (min, 0; max, 299) and 220 min (min, 8; max, 421). With the MPP, mean supine time decreased to 10 min (min, 0; max, 63) (p = 0.02), and the mean lateral time was 186 min (min, 0; max, 380) (p = 0.5). The mean prone time increased from 42 min (min, 0; max, 390) to 174 min (min, 7; max, 300) (p = 0.02) with the MPP. Eleven patients spent no time in the supine position with the treatment ().
AHI/ODI
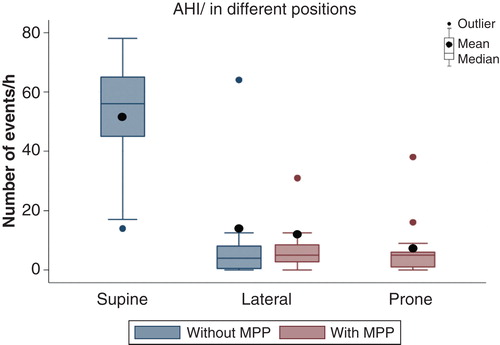
The mean AHI and ODI without treatment were 26 (min, 6; max, 53) and 21 (min, 6; max, 51) and decreased to 8 (min, 1; max, 26) and 7 (min, 1; max, 25), respectively, with the MPP (p < 0.001) (). Eleven patients (79%) achieved an AHI < 10 with the MPP and 10 patients (71%) reduced the AHI by at least 50% and reached a value < 10 during treatment. All patients had a reduction in AHI () and ODI, even if they did not meet these criteria.
Figure 4. Distribution of apnoea/hypopnoea index (AHI) and oxygen desaturation index (ODI) during the first polysomnographic (PSG) study night without treatment (blue) and the second study with the mattress and pillow for prone positioning (MPP) (red).
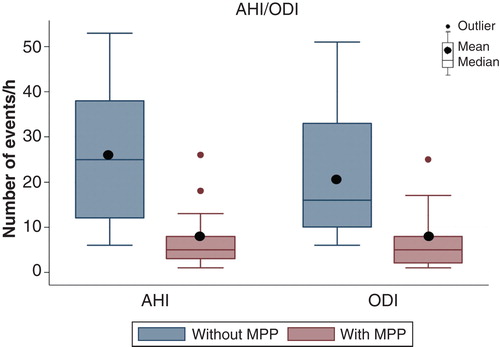
The AHI altered depending on the position (). Without MPP the mean supine AHI was 52 (min, 14; max, 78) and decreased to 7 (min, 0; max, 38) in the prone position during the second night with the MPP (p < 0.005) (). The mean AHI in the lateral positions did not alter significantly (from 14 to 12; p = 0.6) regardless of treatment.
Figure 5. Apnoea/hypopnoea index (AHI) distribution without and with the mattress and pillow for prone positioning (MPP). The prone AHI without treatment and the supine AHI with MPP are omitted due to short registration time.
With the MPP the mean SaO2-min increased from 80% (min, 54; max, 91) to 87% (min, 78; max, 93) (p < 0.05). Without treatment 13 patients (93%) had SaO2-min < 90%, 9 patients (64%) < 85% and 5 patients (36%) < 80%. With the MPP eight patients (57%) had SaO2-min < 90%, four patients (29%) < 85% and one patient (7%) < 80%.
Sleep architecture
The mean rapid eye movement (REM) sleep time remained at 19% without and with MPP, and non-significant alterations in mean N3 sleep time and mean sleep efficiency were observed.
Questionnaires
Ten of 14 patients returned the ESS questionnaires. The mean ESS score was reduced from 12 to 9 (p = 0.007). Without treatment seven patients had an ESS score > 10 and after 4 weeks with the MPP this number was reduced to three (p < 0.05).
Four patients complained about discomfort in the back during the first week with the MPP. However, compliance was satisfactory with all the patients using the MPP > 4 h per night during the 4-week follow-up.
Discussion
The present study shows a beneficial effect of the prone sleeping position on the severity of disease in patients with OSA. The mean total AHI and ODI decreased from 26 and 21 to 8 and 7, respectively, with the MPP. The mean supine time decreased from 128 to 10 min and the mean prone time increased from 42 to 174 min with treatment. AHI in the supine position was 52 without treatment and AHI in the prone position was 7 with the MPP.
Twelve patients (86%) reduced their baseline AHI by > 50%, 11 patients (79%) achieved an AHI < 10 and 8 patients (57%) an AHI ≤ 5 with the MPP (). This was achieved with no disruption of the sleep architecture judged by PSG.
Figure 6. Individual apnoea/hypopnoea index (AHI) during the first polysomnographic (PSG) study night without treatment and the second night with the mattress and pillow for prone positioning (MPP).
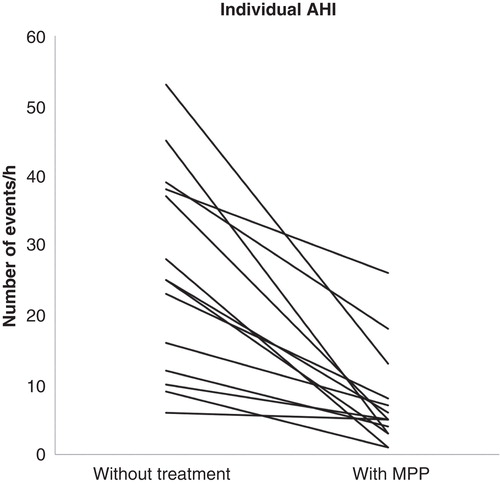
Compliance was satisfactory, with all the patients completing the study with sleep time of > 4 h per night with the MPP. At baseline, 6 of 15 patients were under treatment with either CPAP or an oral device. At the end of the study, 14 patients (93%) wished to continue with the MPP. One patient was excluded from the presented results due to failure in the recording of oxygen saturation during the first PSG study night. This patient had an AHI of 17 without the MPP during the PSG screening night. AHI was 1 with the MPP and the patient chose also to continue with the MPP. Five of six patients with a previously initiated OSA treatment preferred to continue with the MPP, while one patient chose to go back to the previous treatment with CPAP at the end of the study.
The patients were encouraged to supply us with feedback regarding possible alteration in the MPP to satisfy their personal preferences. Two patients desired a shorter mattress for partial body support and eight patients a longer and wider mattress for full body support. Five patients desired a softer mattress.
Previous trials regarding patients with respiratory distress syndrome and acute respiratory failure indicate improved oxygenation and reduced mortality when patients are nursed in the prone position compared with the supine position [Citation17–19]. Our observations have shown that prone positioning with the MPP reduced the mean ODI from 21 to 7 and increased the mean SaO2-min from 80% to 87%.
A limitation in the present study was the lack of monitoring of the position of the head. In an earlier study, van Kesteren et al. found that the occurrence of OSA depends not solely on the position of the trunk but also on the position of the head [Citation20]. According to our observations in a previous study, the head position is important for the effect on severity of disease [Citation14]. In the present study one patient had a prone sleep time of 390 min and an AHI of 23 without treatment. During the second PSG study with the MPP the AHI was improved to 8, probably due to prone positioning of the head.
Humans seems to be one of the few mammals preferring the supine sleep position and also one of the few vertebrates with observed sleep apnoea. Based on our observations, sleeping in the prone position reduces the tendency towards airway collapse and improves respiration in patients with OSA. Future studies should assess the long-term compliance and possible side effects of prone positioning.
Conclusions
Prone positioning with the MPP improved AHI and ODI in patients with OSA, with satisfactory compliance during the 4-week follow-up. Further studies are needed to assess the long-term compliance and efficiency of this novel method.
Acknowledgments
We would like to thank Raquel Praça Silva and Arash Bidarian-Moniri for their important contributions to the design and the development of the MPP, Christopher Oldmeadow for his feedback on the final draft, Carlos Praça for drawing the 3D models of the MPP, Fernando Molina for the production of the instruction video, Ann-Christin Mjörnheim and Henrik Söderström for their assistance in performance of the PSG registrations and the participating patients for their valuable feedback.
Declaration of interest: This study was partially financed by the Acta Otolaryngologica Foundation, Sweden. The sponsor had no role whatsoever in the study design, in the collection, analysis and interpretation of data, the writing of the manuscript or the decision to submit the manuscript for publication. Armin Bidarian-Moniri is the patent-holder for the ‘Pillow and Mattress for Reducing Snoring and Sleep Apnoea’.
References
- Cartwright RD. Effect of sleep position on sleep apnea severity. Sleep 1984;7:110–14.
- Richard W, Kox D, den Herder C, Laman M, van Tinteren H, de Vries N. The role of sleep position in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 2006;263:946–50.
- Sunnergren O, Brostrom A, Svanborg E. Positional sensitivity as a confounder in diagnosis of severity of obstructive sleep apnea. Sleep Breath 2013;17:173–9.
- Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis 1993;147:887–95.
- Richard W, Venker J, den Herder C, Kox D, van den Berg B, Laman M, et al. Acceptance and long-term compliance of nCPAP in obstructive sleep apnea. Eur Arch Otorhinolaryngol 2007;264:1081–6.
- Petit FX, Pepin JL, Bettega G, Sadek H, Raphael B, Levy P. Mandibular advancement devices: rate of contraindications in 100 consecutive obstructive sleep apnea patients. Am J Respir Crit Care Med 2002;166:274–8.
- van Maanen JP, Meester KA, Dun LN, Koutsourelakis I, Witte BI, Laman DM, et al. The sleep position trainer: a new treatment for positional obstructive sleep apnoea. Sleep Breath 2013;17:771–9.
- Oksenberg A, Gadoth N. Are we missing a simple treatment for most adult sleep apnea patients? The avoidance of the supine sleep position. J Sleep Res 2014;23:204–10.
- Skinner MA, Kingshott RN, Filsell S, Taylor DR. Efficacy of the ’tennis ball technique’ versus nCPAP in the management of position-dependent obstructive sleep apnoea syndrome. Respirology 2008;13:708–15.
- Permut I, Diaz-Abad M, Chatila W, Crocetti J, Gaughan JP, D’Alonzo GE, et al. Comparison of positional therapy to CPAP in patients with positional obstructive sleep apnea. J Clin Sleep Med 2010;6:238–43.
- Heinzer RC, Pellaton C, Rey V, Rossetti AO, Lecciso G, Haba-Rubio J, et al. Positional therapy for obstructive sleep apnea: an objective measurement of patients’ usage and efficacy at home. Sleep Med 2012;13:425–8.
- van Maanen JP, de Vries N. Long-term effectiveness and compliance of positional therapy with the sleep position trainer in the treatment of positional obstructive sleep apnea syndrome. Sleep 2014;37:1209–15.
- Menon A, Kumar M. Influence of body position on severity of obstructive sleep apnea: a systematic review. ISRN Otolaryngol 2013;2013:670381.
- Bidarian-Moniri A, Nilsson M, Rasmusson L, Attia J, Ejnell H. The effect of the prone sleeping position on obstructive sleep apnoea. Acta Oto-Laryngologica 2014:1–6. [ Epub ahead of print].
- Iber C, Ancoli-Israel S, Chesson A, Quan SF. The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specification. Westchester, IL: American Academy of Sleep Medicine. 2007.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540–5.
- Abroug F, Ouanes-Besbes L, Elatrous S, Brochard L. The effect of prone positioning in acute respiratory distress syndrome or acute lung injury: a meta-analysis. Areas of uncertainty and recommendations for research. Intensive Care Med 2008;34:1002–11.
- Sud S, Friedrich JO, Taccone P, Polli F, Adhikari NK, Latini R, et al. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta-analysis. Intensive Care Med 2010;36:585–99.
- Guerin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013;368:2159–68.
- van Kesteren ER, van Maanen JP, Hilgevoord AA, Laman DM, de Vries N. Quantitative effects of trunk and head position on the apnea hypopnea index in obstructive sleep apnea. Sleep 2011;34:1075–81.