Abstract
Conclusion: Additional treatment with clarithromycin (CAM) reduced persistent middle ear inflammation after acute otitis media (AOM) caused by Haemophilus influenzae in children. CAM is a treatment option for persistent inflammation following AOM and to prevent continuing otitis media with effusion. Objective: We conducted a clinical study to evaluate a new method of treatment for persistent inflammation after AOM in children. Methods: H. influenzae-infected children with AOM were treated acutely with antimicrobial agents, after which those still demonstrating effusion of the middle ear cavity received additional treatment with carbocysteine (S-CMC) alone or S-CMC combined with clarithromycin (CAM) for 1 week. The two regimens were compared in terms of clinical effects. Results: After the initial acute treatment, many patients still showed abnormal otoscopic findings. At the completion of additional treatment, there were no significant differences between the two treatment groups. However, 1 week after completion of additional treatment, the prevalence of a diminished light reflex was significantly lower in the CAM + S-CMC group than in the S-CMC group (p = 0.017). The prevalence of redness of the tympanic membrane also tended to be lower in the combined treatment group than in those receiving a single drug (p = 0.097).
Keywords:
Introduction
Acute otitis media (AOM) is one of the most common diseases in children. As prevalence of single viral AOM has been reported to account for less than 5% of cases, AOM is most frequently caused by bacterial infection or a combination of viral and bacterial agents [Citation1]. Therefore, it is necessary to choose appropriate antibiotics. Recently, clinical guidelines for AOM have been published in many countries including Japan. Following antibiotic treatment recommended by such guidelines, some children show little improvement regarding otoscopic findings, and they may suffer refractory or recurrent AOM. This is partly because of the drug resistance of common organisms causing AOM, i.e. penicillin-resistant Streptococcus pneumoniae (PRSP), β-lactamase-producing ampicillin-resistant (BLPAR) and β-lactamase-negative ampicillin-resistant (BLNAR) Haemophilus influenzae. In recent years in Japan, while the prevalence of PRSP isolation from AOM has declined, an increase in the occurrence of infection with BLNAR strains has occurred [Citation2].
Symptoms of AOM caused by H. influenzae are less severe than those due to S. pneumoniae, but can be prolonged or recur in many cases [Citation3]. This is partly explained by cell-invasive H. influenzae, which has recently been attracting attention. When H. influenzae organisms attach to and invade epithelial cells, these bacteria can escape both antimicrobial sterilization and the host immune response [Citation4]. Because β-lactams do not penetrate cells well, they fail to come into contact with the bacteria and thus cannot exert their clinical effects. In addition, mixed infections of S. pneumoniae and H. influenzae allow both organisms to adapt better for biofilm formation, leading to the persistence of inflammation in AOM [Citation5]. Indeed, biofilm formation was frequently detected in the middle ear mucosa of children with recurrent AOM and chronic otitis media with effusion [Citation6]. Furthermore, otitis media cannot totally be prevented by vaccination, because of the prevalence of nontypable noncapsulate strains of H. influenzae associated with otitis media.
As H. influenzae may be associated with persistent infection of the middle ear following acute treatment with antimicrobial agents, we evaluated the effects of an additional AOM treatment in children infected with H. influenzae following standard primary therapy. Clarithromycin (CAM), a macrolide, is a suitable candidate for secondary treatment because it is able to kill intracellular H. influenzae and to eradicate the biofilm [Citation7,8].
Material and methods
Patients
This study included children younger than 15 years of age with acute or recurrent otitis media, who visited the Department of Otorhinolaryngology of Jichi Medical University Saitama Medical Center, or associated clinics, between March 2009 and August 2012. The inclusion criterion was infection with H. influenzae (including mixed infections) at enrolment in the study. Exclusion criteria were as follows: children with a history of AOM or otitis media with effusion within 1 month before the onset of the current episode; children with tympanostomy tube placement; children with craniofacial abnormalities or immunodeficiency. Children with recurrent otitis media were also included in this study. Recurrent otitis media was defined as at least three episodes of AOM within the past 6 months, or at least four episodes within the last year. Among the patients meeting these criteria, we included children with persistent inflammation of the middle ear following amelioration of acute inflammation by use of antimicrobial agents for AOM.
Patients’ guardians provided informed consent for participation in the study, following a full explanation of the objective and methods of the study, expected effects and risks, and other relevant matters. This study was approved by the ethics committee of Jichi Medical University Saitama Medical Center.
Bacteriological examination
In the first instance, specimens were collected from the middle ear following myringotomy or otorrhea or from the nasopharynx, for bacteriological culture and examination. This constituted the first examination. The collected samples were sent to each hospital’s contract laboratory for isolation and identification of microorganisms. Patients who were culture positive for H. influenzae (including mixed infections) at the first examination and subsequently received additional treatment also underwent bacteriological screening by the same method upon completion of the additional treatment regimen – the second examination. The minimum inhibitory concentration (MIC) of several antimicrobial agents against H. influenzae detected at both the first and second examinations was determined by laboratory analysis.
Acute treatment
Children who were diagnosed as having AOM at the first visit received antimicrobial agents based on the severity of their otitis media infection. Severity was assessed according to the criteria specified by the Clinical Practice Guidelines for the Diagnosis and Management of Acute Otitis Media (AOM) in Children in Japan 2009 (subsequently referred to as the Japan Guidelines) [Citation2]. Briefly, the severity of AOM was defined by a scoring system using eight categories: age (<24 months), clinical manifestations of otalgia, crying and/or bad temper and fever, and otoscopic findings of hyperemia, protrusion of the eardrum, otorrhea, and diminishment of light reflex (). The duration of treatment was 5–14 days depending on otoscopic findings and the elimination of acute symptoms.
Table I. Scoring system for the severity of acute otitis media (AOM) [Citation2].
Additional treatment
Additional treatment was administered to patients demonstrating persistent inflammation of the middle ear after the acute phase had been ameliorated by appropriate primary treatments. Patients were asked about any history of disease of the nose or ears, complicating allergies, nutrition in infancy, attendance of day nursery, presence/absence of a smoker in the family, and disease symptoms using an interview sheet. Tympanometry was also performed before commencement of additional treatment.
Children with persistent inflammation were divided into two groups; group A, carbocysteine (S-carboxymethyl-L-cysteine, S-CMC) only; group B, CAM + S-CMC combination therapy. Patients with odd-numbered medical records were assigned to group A, and those with even-numbered records to group B. Both CAM and S-CMC were administered orally for 1 week at a daily dose of 15 mg/kg divided into two doses, or 30 mg/kg in two to three divided doses for CAM and S-CMC, respectively. In both groups, patients who still showed clinical manifestations and were not cured upon completion of the additional treatment regimen continued to receive S-CMC and were examined weekly until the middle ear inflammation had fully resolved.
End points
Clinical assessment. Severity of clinical manifestations and otoscopic findings was assessed based on the criteria in upon completion of additional treatment, and during the follow-up period.
Bacteriological effects. The eradication rates of H. influenzae and two further common bacterial species (S. pneumoniae and Moraxella catarrhalis) were assessed upon completion of additional treatment.
Results
Patient randomization and baseline characteristics
A total of 133 patients were enrolled in the study, with 60 patients in the S-CMC group and 73 in the CAM + S-CMC group. The patients’ baseline characteristics are presented in . Patients were between 8 and 137 months (mean, 51.2 months) of age in the S-CMC group and between 6 and 179 months (mean, 50.3 months) in the CAM + S-CMC group. In both groups, less than 10% of the patients underwent myringotomy when starting acute treatment. Upon initiation of additional treatment, a type B tympanogram, an indicator of middle ear fluid, was noted in 53.3% of the patients in the S-CMC group and 64.4% of those in the CAM + S-CMC group. No significant differences were found in any patient baseline characteristics between the two groups.
Table II. Patients’ baseline characteristics.
Questionnaires collected from 116 of the 133 patients were examined. Assessment of the history of nose or ear diseases revealed that 69.8% of the responders had a history of AOM, 5.2% had a history of otitis media with effusion, and 5.2% had a history of rhinosinusitis. Assessment of complicating allergies showed allergic rhinitis to be the most common (5.2%), with other allergies seen in 2% or less of the respondents. Assessment of nutrition in infancy indicated breast milk to be the most common method of feeding (67.8%), followed by a combination of breast milk and formula (17.4%) and formula alone (14.8%). Group nursing was experienced by 72.2% of the respondents and 38.3% had a smoker in the family. Assessment of symptoms revealed that 57.8% had nasal discharge/obstruction. There were no statistical differences between the two groups regarding clinical history and background.
Clinical outcome
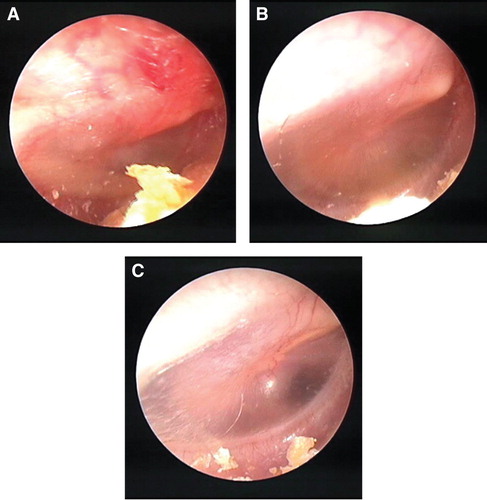
shows the otoscopic findings of a patient during the study. The patient was a 74-month-old girl, suffering from severe otitis media (score = 16) with severe redness and protrusion of the tympanic membrane and a markedly diminished light reflex in the right ear at initiation of acute treatment. After administration of amoxicillin (AMPC) for 7 days, only protrusion of the tympanic membrane showed slight improvement, reducing the score to 12. After 7 days of additional treatment with CAM combined with S-CMC, all of the findings resolved completely.
Figure 1. Changes in the otoscopic findings of a patient with acute otitis media. (A) At the initiation of acute treatment (amoxicillin, AMPC); score = 16. (B) At the initiation of additional treatment (S-CMC + CAM); score = 12 (after 7 days). (C) At the completion of additional treatment; score = 0 (after 14 days).
summarizes the prevalence of clinical manifestations and otoscopic findings in patients receiving additional treatment during the study. About one-third of the patients were under 24 months of age. At initiation of acute treatment, clinical manifestations were seen only in a relatively small percentage of patients, except for otalgia, which was common. However, the three otoscopic findings under observation were noted in most of the patients in both groups; after acute treatment, 86.7% and 87.7% of the patients had a diminished light reflex; 58.9% and 63.3% showed redness of the tympanic membrane; and protrusion of the tympanic membrane was seen in 38.3% and 38.4% of the patients, respectively. Thus, many patients still demonstrated disease-associated otoscopic findings.
Table III. Proportion of patients with clinical manifestations and otoscopic findings.
Upon completion of additional treatment, the prevalence of otoscopic findings was reduced. Diminished light reflex was detected in 43.3% of patients in the S-CMC group and 46.6% of patients in the CAM + S-CMC group. Redness of the tympanic membrane was observed in 41.7% of patients in the S-CMC group and 32.9% of patients in the CAM + S-CMC group, while protrusion of the tympanic membrane was noted in 23.3% of patients in both groups. No significant differences were found in the proportion of patients with any of these findings between the two groups. One week after completion of additional treatment, we evaluated the clinical manifestations and otoscopic findings in 27 patients in the S-CMC group and 38 patients in the CAM + S-CMC group. Among the patients, the prevalence of diminished light reflex in the CAM + S-CMC group was significantly lower than that in the S-CMC group (52.6% vs 81.5%, respectively; chi-squared test, p < 0.05). A similar trend was observed regarding redness of the tympanic membrane, with 42.1% in the CAM + S-CMC group and 63.0% in the S-CMC group still demonstrating this symptom (chi-squared test, p = 0.097).
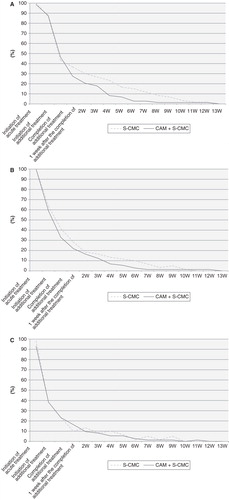
Changes in severity score of AOM are shown in . Upon completion of additional treatment, the median score (50th percentile) was three in both the CAM + S-CMC and S-CMC groups, and decreased to zero at 1 week following cessation of treatment. The 75th percentile achieved a severity score of zero in the CAM + S-CMC and S-CMC groups at 2 and 4 weeks, respectively, following completion of additional treatment, thus indicating an earlier resolution of disease in the CAM + S-CMC group.
Table IV. Changes in the otitis media severity score.
shows changes in the proportion of 60 patients in S-CMC group and 73 patients in CAM + S-CMC group with otoscopic findings. The patients still demonstrated diminished light reflex, redness of the tympanic membrane, or otorrhea, symptoms that were commonly observed following completion of acute treatment. The proportion of patients with a diminished light reflex was approximately 10% lower in the CAM + S-CMC than in the S-CMC group from 1 to 7 weeks after completion of additional treatment and resolved earlier in the CAM + S-CMC group (). The proportion of patients with redness of the tympanic membrane also tended to decrease earlier in the CAM + S-CMC group (). However, little difference was noted between the two groups in the proportion of patients with otorrhea symptoms ().
Bacteriological effects
At initiation of additional treatment, H. influenzae, including mixed infection, was detected in all patients. shows the eradication rate of H. influenzae and two further common bacterial species (S. pneumoniae and M. catarrhalis) upon completion of additional treatment. The eradication rates of H. influenzae were similar between the two groups, with 36.7% in the S-CMC group and 37.0% in the CAM + S-CMC group demonstrating clearance. Similarly, the eradication rates of both S. pneumoniae, and M. catarrhalis tended to be higher in the CAM + S-CMC group. Assessment of the antimicrobial activity of CAM against H. influenzae revealed that the MIC50 was 4–8 µg/ml in both groups at the initiation of acute treatment and upon completion of additional treatment. The MIC90 was 8 µg/ml in both groups at both time points (). No adverse effects were reported during the treatment period.
Table V. Eradication rate of bacterial species at the completion of additional treatment.
Table VI. Antimicrobial activity against H. influenzae.
Discussion
S. pneumoniae and H. influenzae are the most common microbial agents of AOM in children. The prevalence of S. pneumoniae and H. influenzae in AOM is 19–74% and 16–61%, respectively [Citation4]. A recent study demonstrated that H. influenzae infection may be responsible for persistent inflammation in the middle ear [Citation3], and effective antimicrobial agents against H. influenzae make treating AOM of this etiology challenging. In the Japan guidelines [Citation2], use of AMPC is recommended as the first-line treatment for mild and moderate grade AOM, as defined by severity score, when the administration of antimicrobial agents is needed. For severe grade AOM, use of AMPC, clavulanic acid (CVA)/AMPC, and cefditoren-pivoxil is recommended. Therefore, these three drugs, but mainly AMPC, were used for the acute phase of treatment in the present study. However, these drugs are not effective against organisms that have invaded host cells to cause persistent inflammation, and neither AMPC nor CVA/AMPC have strong antimicrobial activity against H. influenzae.
In the meta-analysis of seven articles by Rosenfeld and Kay [Citation9], persistent effusion was found in 41% of patients after 4 weeks, 54% after 8 weeks, and 26% after 12 weeks in children who did not receive treatment for AOM. Therefore, appropriate treatment is needed to cure acute inflammation as well as to prevent progression to otitis media with effusion. The present study was conducted to investigate whether CAM, a macrolide, could resolve persistent inflammation in AOM caused by H. influenzae, as CAM is known to kill intracellular H. influenzae and to eradicate biofilms. In addition to antimicrobial activity, CAM also demonstrates anti-inflammatory and immunomodulatory effects [Citation10,11]. We also used S-CMC as an additional treatment in both groups, because it is commonly used to regulate airway mucus and normalize mucosa. Oral administration of S-CMC accelerated clearance of middle ear effusion in experimental otitis media with effusion [Citation12]. Meta-analysis of seven articles showed that use of S-CMC resulted in a 35% improvement of otitis media with effusion compared with only 17% improvement in the control group [Citation13]. In the present study, we investigated the effect of add-on administration of CAM to S-CMC for persistent inflammation after acute middle ear infection subsided.
As the results indicate, CAM showed the greatest efficacy against otoscopic findings, especially regarding diminished light reflex. Normally, the light from the otoscope reflects off the eardrum in a characteristic fashion, and is called the cone of light or light reflex. Diminished or reduced light reflex of the eardrum usually indicates the presence of persistent inflammation of the middle ear with or without effusion. Hotomi et al. [Citation14] reported that the eardrum change including reduced light reflex was one of the very important indicators to predict the outcome of AOM. The proportion of patients with this finding was significantly lower in the CAM + S-CMC group than in the S-CMC group at 1 week following completion of additional treatment (p < 0.05). The proportion of patients with redness of the tympanic membrane also tended to be lower in the CAM + S-CMC group (p = 0.097). These findings suggest that CAM ameliorates otoscopic findings that are likely to persist after acute treatment and accelerates resolution of inflammation. This may be partly because of its action on intracellular H. influenzae. However, there was little difference in the eradication rate of H. influenzae between the two treatment groups at completion of additional treatment. The reason that CAM was more effective in elimination of persistent inflammation may be the reduction of the overall bacterial count, including intracellular H. influenzae, although we did not directly observe bacterial counts in this study. Further study is needed to clarify this aspect of disease resolution. It is also possible that the higher eradication rate of other common bacterial species in the CAM + S-CMC group was reflected in the better outcome observed in this group.
Recently, the effectiveness of CAM on subacute and chronic phases of otitis media with effusion has been reported [Citation15]. Macrolide therapy, using 14-membered ring macrolides such as erythromycin or CAM, has been reported to be effective for a wide range of diseases, including diffuse panbronchiolitis and chronic sinusitis [Citation10,11,16]. The mechanisms underlying the effectiveness of macrolides are reportedly associated with anti-secretory effects (water/mucus); anti-inflammatory effects including inhibition of neutrophil function, inhibition of cytokine production, and other effects; inhibition or destruction of biofilms, and enhancement of ciliary activity [Citation17,18]. Among these effects, the anti-secretory action, thus reducing middle ear fluid, and inhibition of interleukin (IL)-8 or neutrophil activity [Citation19], therefore reducing inflammation, is closely associated with otitis media. Takaki et al. [Citation20] reported that in adenoidal fibroblasts, CAM inhibited production of IL-8 through NF-κB activation in response to endotoxin. The authors’ suggestion that the inhibitory effects of CAM are mediated through NF-κB activation and IL-8 inhibition in adenoidal fibroblasts might explain, in part, the mechanism of this drug in improving otitis media with effusion.
The results of the present study suggest that CAM may be a suitable candidate drug for preventing persistent or recurrent otitis media in children following acute treatment for AOM.
Acknowledgement
Taisho Toyama Pharmaceutical Company was the funding source for bacteriological examination of middle ear effusions and nasopharyngeal smears, and was involved in the study conduct and analysis.
Declaration of interest: The corresponding author declares having grants from Taisho Toyama Pharmaceutical Company for conducting the study. The authors alone are responsible for the content and writing of the paper.
References
- Heikkinen T, Chonmaitree T. Importance of respiratory viruses in acute otitis media. Clin Microbiol Rev 2003;16:230–41.
- Japan Otological Society, Japan Society for Pediatric Otorhinolaryngology, Japan Society for Infection and Aerosol in Otorhinolaryngology. 2013. Clinical practice guidelines for the diagnosis and management of acute otitis media (AOM) in children in Japan 2013. Tokyo: Kanehara & Co.
- Barkai G, Leibovitz E, Givon-Lavi N, Dagan R. Potential contribution by nontypeable Haemophilus influenzae in protracted and recurrent acute otitis media. Pediatr Infect Dis J 2009;28:466–71.
- Clementi CF, Murphy TF. Non-typeable Haemophilus influenzae invasion and persistence in the human respiratory tract. Front Cell Infect Microbial 2011;1:1–9.
- Dagan R, Leibovitz E, Greenberg D, Bakaletz L, Givon-Lavi N. Mixed Pneumococcal-nontypeable Haemophilus influenza otitis media is a distinct clinical entity with unique epidemiologic characteristics and pneumococcal serotype distribution. J Infect Dis 2013;208:1152–60.
- Hall-Stoodley L, Hu FZ, Gieseke A, Nistico L, Nguyen D, Hayes J, et al. Direct detection of bacterial biofilms on the middle-ear mucosa of children with chronic otitis media. JAMA 2006;296:202–11.
- Nakamura S, Yanagihara K, Araki N, Yamada K, Norinaga Y, Izumikawa K, et al. Efficacy of clarithromycin against experimentally induced pneumonia caused by clarithromycin-resistant Haemophilus influenzae in mice. Antimicrob Agents Chemother 2010;5:757–62.
- Uemura Y, Qin Y, Gotoh K, Ohta K, Nakamura K, Watanabe H. Comparison study of single and concurrent administrations of carbapenem, new quinolone, and macrolide against in vitro nontypeable Haemophilus influenzae mature biofilm. J Infect Chemother 2013;19:902–8.
- Rosenfeld RM, Kay D. Natural history of otitis media. Laryngoscope 2003;113:1645–57.
- Kudoh S, Uetake T, Hagiwara K, Hirayama M, Hus LH, Kimura H, et al. [Clinical effects of low-dose long-term erythromycin chemotherapy on diffuse panbronchiolitis.]. Nihon Kyobu Shikkan Gakkai Zasshi 1987;25:632–42; in Japanese.
- Cervin A, Wallwork B. Macrolide therapy of chronic rhinosinusitis. Rhinology 2007;45:259–67.
- Hori F, Kawauchi H, Mogi G. Effect of S-carboxymethylcysteine on the clearance of middle ear effusion. An experimental study. Ann Otol Rhinol Laryngol 1994;103:567–75.
- Moore RA, Commins D, Bates G. S-carboxymethylcysteine in the treatment of glue ear: quantitative systematic review. BMC Fam Pract 2001;2:3.
- Hotomi M, Yamanaka N, Shimada J, Ikeda Y, Faden H. Factors associated with clinical outcome in acute otitis media. Ann Otol Rhinol Laryngol 2004;113:846–52.
- Chen K, Wu X, Jiang G, Du J, Jiang H. Low dose macrolide administration for long term is effective for otitis media with effusion in children. Auris Nasus Larynx 2013;40:46–50.
- Statham MM, Seiden A. Potential new avenues of treatment for chronic rhinosinusitis: an anti-inflammatory approach. Otolaryngol Clin North Am 2005;38:1351–65.
- Shinkai M, Henke MO, Rubin BK. Macrolide antibiotics as immunomodulatory medications; proposed mechanisms of action. Pharmacol Ther 2008;117:393–405.
- Kitano M, Ishinaga H, Shimizu T, Takeuchi K, Majima Y. Effect of clarithromycin and dexamethasone on mucus production in isografted rat trachea. Pharmacology 2011;87:56–62.
- Fujita K, Shimizu T, Majima Y, Sakakura Y. Effects of macrolides on interleukin-8 secretion from human nasal epithelial cells. Eur Arch Otorhinolaryngol 2000;257:199–204.
- Takaki M, Ushikai M, Deguchi K, Nishimoto K, Matsune H, Kurono Y. The role of nuclear factor-kappa B in interleukin-8 expression by human adenoidal fibroblasts. Laryngoscope 2003;113:1378–85.