Abstract
Objective: To explore the effect of ever having tried to conceive for more than 12 months on levels of anxiety and depressive symptoms and to investigate if symptom levels of anxiety and depression in infertile women who remain childless, or go on to have children, respectively, differ from symptom levels in mothers without reports of infertility.
Methods: Analyses were based on information from 12 584 Norwegian women aged 19–45 years who participated in the North-Trøndelag Health Study from 1995 to 1997 and data from the Medical Birth Registry of Norway. Anxiety and depressive symptoms were measured by the Hospital Anxiety and Depression Scale.
Results: Having tried to conceive for more than 12 months (ever) was weakly associated with higher levels of depressive symptoms. In the categorical analyses, women with resolved infertility had higher levels of anxiety symptoms (B = 0.25 (95% confidence interval (CI) = 0.04–0.47)) and voluntarily childfree had lower levels of depressive symptoms (B = –0.05 (95% CI = –0.50 to –0.21)) than mothers without infertility. However, women with current primary or current secondary infertility had levels of anxiety and depression not significantly different from mothers without infertility.
Conclusion: At the population level, and from a longitudinal perspective, unresolved infertility is less burdensome than findings from studies on women seeking help for infertility would suggest.
Introduction
Cross-sectional surveys on women who seek medical care for infertility (i.e. clinical samples) have found that levels of mental distress and symptoms of anxiety and depression are higher [Citation1–7] and quality of life lower [Citation6,Citation8–11] in infertile women compared with control samples without fertility problems or population norms [Citation5,Citation6]. Reports suggest that up to one-third of women seeking help for infertility score above cut-off values for a mental condition [Citation1,Citation11,Citation12], which is similar to the prevalence of mental disorders seen in patients with somatic conditions [Citation13]. However, the association between infertility and symptoms of common mental conditions may be less pronounced in the general female population than in infertility clinic attendees [Citation14], as the less than half of couples [Citation15,Citation16] with infertility who seek medical help are more likely to have a longer duration of infertility, higher levels of distress and higher prevalence of co-morbid somatic conditions than non-help-seeking couples [Citation7,Citation17]. In addition, fertility treatment is associated with levels of distress over and above those associated with the state of being infertile in and of itself [Citation18].
The very few population-based studies that have assessed the association between infertility and mental health have yielded inconclusive results: a study using a random US sample of 580 women found that infertility, defined as ever having tried to conceive or having had regular unprotected intercourse for more than 12 months without conceiving, was associated with higher depressive symptom levels than when no fertility problems were reported [Citation19]. In the same sample, the prevalence of case-level mental distress was 27% in infertile women with intent of getting pregnant [Citation20]. However, a large Finnish study using stratified cluster sampling and a structured psychiatric diagnostic interview did not find increased risk for mental disorders overall, but did report an increased risk for dysthymia or anxiety disorder in childless women who had tried to conceive for more than 12 months without success compared with women without fertility problems [Citation16]. However, levels of depressive symptoms and general distress in women who had made unsuccessful attempts to conceive a child over a period of 12 months or longer at any time of their life were comparable with the fertile reference population. These conflicting results make it difficult to come to firm conclusions regarding whether infertility is associated with increased levels of anxiety and depressive symptoms at the population level. We therefore carried out this study, first to test the associations between ever having tried to conceive for more than 12 months without achieving pregnancy and levels of anxiety or depressive symptoms; and second, to investigate if symptom levels of anxiety and depression in infertile women who remain childless, or who have gone on to have children, respectively, differ from symptom levels in mothers without reports of infertility in the general population.
Methods
All adult inhabitants in the county of North-Trøndelag (total population 127 000) were invited to participate in the second wave of the North-Trøndelag Health Study (HUNT 2) from 1995 to 1997. Of the 94 194 individuals aged 19 years or older who were invited, 92 936 were eligible for participation. Of them, 66 140 (71%) women and men provided written informed consent and completed “Questionnaire 1”, which was mailed to participants along with the invitation to participate approximately two weeks prior to the physical examinations. “Questionnaire 1” included the 14-item Hospital Anxiety and Depression Scale (HADS) [Citation21,Citation22] and questions about demographic characteristics, somatic conditions, use of medication and lifestyle. “Questionnaire 2”, which was given to female participants at the study sites to be completed at home and then returned via mail, included questions about fertility-related problems, menstrual history and history of gynecological surgery. This article is based on a linkage file with data from the HUNT 2 and the Medical Birth Registry of Norway (MBRN). The MBRN file used includes information about all pregnancies in Norway registered for antenatal care from 1967 to 2008. Data from the MBRN were used for retrospective detailing of number of pregnancies and births. This project was approved by the Regional Committee for Medical Research Ethics (ref. no. 4.2007.275) and the Norwegian Data Inspectorate (ref. no. 08/01940-2/CGN).
Data sampling
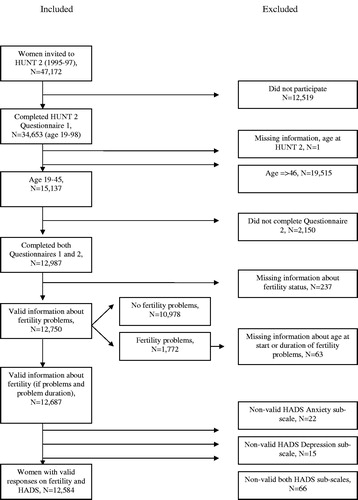
The flow chart in displays the procedure of sampling. Of the 34 653 women aged 19–98 years (74%) who completed “Questionnaire 1”, 15 137 were between 19 and 45 years of age (i.e. in the reproductive age span). Of the 12 750 who provided a valid answer to the question “Have you ever tried to get pregnant for more than one year?”, 1772 (14%) answered “Yes”. Of them, 1709 provided a valid answer to the question “If yes, how old were you the first time you experienced problems becoming pregnant?”. Women with missing or inconsistent information about fertility problems or non-valid scores on one or both subscales of the HADS were excluded, leaving 12 584 in the final analysis file (1696 (14%) of these with reports of fertility problems). The valid sample represented 56% of the 22 296 women in the age span 19–45 years invited to HUNT 2.
Fertility status
Fertility status was operationalized using the following mutually exclusive categories: “current primary infertility” (i.e. women who reported having tried to get pregnant for > 12 months and had no live-born children registered in the MBRN at the time of HUNT 2) (n = 350 (3%)), “current secondary infertility” (i.e. women who reported having tried to get pregnant for > 12 months, but with registration of live-born children in the MBRN prior to the date of infertility) (n = 265 (2%)) and “resolved infertility” (women with live-born children after previous primary or secondary infertility) (n = 1081 (9%)). We further defined 2318 women (18%) as being “voluntarily childfree” because they reported no pregnancies in HUNT, were not registered with pregnancy in MBRN and they answered “No” to the question about whether they had ever tried to get pregnant without success. The category of mothers without infertility (n = 8570) was chosen as reference category in the inferential analyzes below as this was large and probably most normative with regard to marital and parenting status in the age span studied.
Measurement of mental distress
Levels of anxiety and depressive symptoms were assessed by the Norwegian version of the HADS [Citation21,Citation22]. HADS assesses anxiety (HADS-A) and depression (HADS-D) on two separate subscales, each of which has seven items. Examples of items are “Worrying thoughts go through my mind” or “I get a sort of frightened feeling as if something awful is about to happen”. Items were scored from 0 to 3, and positively worded items were reverse-scaled before item scores were added up to produce the subscales [Citation21]. The psychometric properties of HADS are regarded as good in terms of internal reliability (intra-scale Cronbach’s alphas of 0.80 and 0.76, respectively) [Citation21], and sensitivity and specificity for the subscale cutoff value ≥ 8 used to indicate case-level distress [Citation23,Citation24].
Statistical analysis
Linear regression models were used to test the associations between infertility and HADS-A or -D subscales. A model with subgroups according to infertility type (current primary, current secondary or resolved infertility) or parenting status (voluntarily childfree or mothers without infertility) as independent variable and HADS subscales as dependent variables was used to assess the associations between fertility status and HADS-A or -D, respectively.
Separate adjustments were performed for variables that could confound the association between infertility and mental health: age (years), education (≤ 9, 10–12, 13–15 or ≥ 16 years), marital status (married/registered partner, unmarried, divorced/separated or widow), hypothyroidism, body mass index (BMI) (< 18.49, 18.50–24.99, 25.00–29.99 or ≥ 30.00), cigarette smoking (current daily smoking or not) and alcohol consumption (no alcohol consumption, 1–9, 10–13 or ≥ 14 units/week). As parenting status could confound the association between infertility and anxiety and depression, the analyses with infertility (ever) as independent variable and HADS subscales as dependent variables were adjusted for parity (i.e. number of live-born children as registered in the MBRN) and the interaction term of infertility with parity. In the final step, all covariates were entered simultaneously (fully adjusted model). With the exceptions of age and parity (which were continuously scaled), adjustment variables were encoded as categorical, with missing data as separate categories.
All analyses were repeated with log-transformed HADS-A and -D subscales as these were not normally distributed and significance was reported from the analyzes performed on the transformed data. Effect sizes and 95% confidence intervals (CIs) were reported from analyses performed on the non-transformed variables. All significance tests were two-tailed with an ά-level of 0.05, except in the categorical analysis with subgroup according to infertility or parity status; in these, the ά-level was set to 0.01 to avoid type I error, which can occur when multiple comparisons are being conducted. Data analyses were performed using STATA 12.0 (StataCorp, College Station, TX, US).
Results
Mean HADS-A and HADS-D scores in the women who reported that they had at some point tried to get pregnant for more than 12 months (irrespective of whether pregnancy was finally achieved, n = 1696 (14%)) were 4.5 (SD = 3.37, range 0–21) and 2.6 (SD = 2.71, range 0–19), respectively. Descriptive statistics of the subgroups and total sample are listed in . HADS-A and -D subscales were intercorrelated (Pearson’s correlation coefficient r = 0.62, p < 0.001). Mean times since start of the first unsuccessful attempt of getting pregnant were 10 years (SD = 6.6, range 1–26), 9 years (SD = 6.2, range 1–26) and 13 years (SD = 5.7, range 3–29) in the subgroups with primary, secondary or resolved infertility, respectively.
Table 1. Descriptive statistics of the total n = 12 584 sample and by subgroup according to fertility status.
Infertility and symptom levels of anxiety and depression
Weak positive associations of infertility, defined as having tried to get pregnant for > 12 months irrespective of whether pregnancy was finally achieved, were found with HADS-A (unadjusted B = 0.25 (95% CI = 0.07–0.42)); and -D (unadjusted B = 0.26 (95% CI = 0.12–0.40); ). After adjustment for relevant confounding factors, only the association between infertility and HADS-D remained statistically significant (B = 0.32 (95% CI = 0.08–0.57)).
Table 2. Linear regression model with infertility (ever) as independent variable and HADS-A or -D subscales as dependent variables; n = 12 584.
In the fully adjusted models, the following covariates made significant independent contributions to levels of anxiety or depressive symptoms: higher number of live-born children, higher age, lower level of education, being divorced and smoking (all p < 0.05). In addition, hypothyroidism and drinking ≥ 10 units of alcohol/week were associated with higher levels of anxiety symptoms; and being unmarried, higher BMI, never drinking alcohol and the interaction term of infertility with parity were inversely associated with more depressive symptoms (all p < 0.05).
Infertility type or parity status versus symptom levels of anxiety and depression
Women with current primary infertility had symptom levels not significantly different from the reference group of mothers without infertility (adjusted B = 0.06 (95% CI = –0.30 to 0.42); and B = –0.10 (95% CI = –0.39 to 0.18) for HADS-A and -D, respectively; ). Furthermore, the subgroup with current secondary infertility had symptom levels comparable with the reference group (adjusted B = –0.12 (95% CI = –0.53 to 0.29); and B = –0.16 (95% CI = –0.48 to 0.17), for HADS-A and -D, respectively).
Table 3. Linear regression model with subgroups of women categorized according to infertility or number of live-born children as independent variable and HADS-A and -D subscales as dependent variables; n = 12 584.
The subgroup of mothers with resolved infertility had the highest symptom levels of all groups with adjusted B = 0.25 (95% CI = 0.04–0.47) for HADS-A and B = 0.12 (95% CI = –0.05 to 0.28) for HADS-D, as compared with the reference category.
Finally, the subgroup of women who were voluntarily childfree had lower levels of depressive symptoms than the reference category (adjusted B = –0.36 (95% CI = –0.50 to –0.21)).
Discussion
This large population study found weak associations between reports of infertility, defined as ever having tried for more than 12 months to conceive (regardless of whether a child was finally conceived or not), and higher levels of anxiety and depressive symptoms; however, after adjusting for relevant confounding factors, only the association between infertility and depressive symptoms remained statistically significant. Mean time since start of the first unsuccessful attempt of getting pregnant was long, and the findings indicate that at the population level, and from a longitudinal perspective, the association between infertility and symptoms of depression is less pronounced than studies on women seeking help for infertility would suggest [Citation1–3,Citation7].
This study design was cross-sectional, with retrospective reports of infertility; therefore, firm conclusions about direction of causality, i.e. whether infertility caused the mental symptoms observed or vice versa, cannot be made. Mental distress has been suggested to be an etiological factor in infertility [Citation3] and has been linked to increased risk of diminished ovarian reserve [Citation25]. However, the existing literature lends more support to the hypothesis of infertility causing mental distress than the opposite [Citation3,Citation7].
In this study, the currently infertile subgroups had levels of anxiety or depressive symptoms comparable to the reference population. This finding is in line with one previous population study that assessed symptom levels of depression and general psychological distress in women with infertility [Citation16], and it is consistent with the finding from the US study in which the weak association between infertility and levels of depressive symptoms became non-significant once adjusted for biological motherhood and other factors [Citation19]. Furthermore, our finding is also in line with long-term follow-up investigations of samples of help-seeking women showing that women with unresolved infertility have levels of mental distress comparable with population norms [Citation26,Citation27] and with a recent Danish cohort study [Citation28]. This study included n = 98 320 women not previously hospitalized for mental disorders. It showed that women who had had infertility evaluation at public or private specialist centers had no increased risk of hospitalization for affective- or anxiety disorders if they did not give birth afterwards compared with women who succeeded in giving birth. However, this study did not clarify whether the women included had undergone ART or not, and it did actually detect an increased risk of hospitalization for some other specific types of mental disorders in women who did not give birth after infertility evaluation.
The lack of difference in anxiety and depressive symptom levels between currently infertile women and the reference category in our study contrasts with a number of earlier studies on women who undergo ART-treatment, which have found elevated levels of symptoms of mental distress or higher prevalence of mental conditions in infertile women [Citation1–3,Citation5–7,Citation28]. This discrepancy in findings between this population study and earlier clinical studies may reflect the previously mentioned selection biases in the clinical [Citation1–3,Citation5–7] or self-selected [Citation4] samples, and possibly also a publication bias (i.e. studies with statistically significant differences between help-seeking women and controls may have been more likely to be published than studies that did not find such group differences). Furthermore, mean time since start of infertility was long in this study. Research on the natural course of psychological reactions to infertility has shown that although infertility initially leads to grief and personal and social distress, it is later associated with coping, acceptance and re-orientation [Citation29–31]. Therefore, it may be that levels of depressive or anxiety symptoms in the infertile women in this study had already returned to levels comparable with mothers without infertility at the time of measurement (after an initial rise in the first phase of infertility).
However, distress related to the parenting role in the reference category of mothers without infertility may represent an alternative explanation for the lack of difference in levels of anxiety and depressive symptoms between currently infertile women and the reference category in this study: it may be that the lack of difference between the infertile subgroups and the reference category was not so much due to low levels in the infertile subgroups, but rather due to higher levels of symptoms and mental distress in the reference category with children. Given that infertility and number of children are both factors associated with higher levels of anxiety [Citation19], the higher level of anxiety symptoms found in women with resolved infertility may be a result of the combined effects of distress related to their current parenting role and to infertility in the past. Previous studies have shown that women with resolved infertility may suffer from persistent psychological, partnership and social distress resulting from their past infertility or infertility treatment, and they may have different mother–child interactions, family functioning and show more anxious over-concern for their existing children [Citation32] than women with naturally conceived children. These are all factors that may explain the present finding of higher levels of anxiety symptoms in women with resolved infertility than in the reference category.
The effect sizes for the difference in HADS scores between the reference population and the other subgroups were small in this study. For instance, the mean difference in HADS-A between the subgroup with resolved infertility and the reference population was only 0.3 point, and the difference in HADS-D between the voluntarily childfree subgroup and the reference population was only 0.9 point. Although the “minimal important difference” of the HADS for infertility samples is not known, earlier research suggests that the difference in HADS scores in this study are not likely to be of clinical significance [Citation33]. However, although the small differences in HADS scores are not likely to be of clinical significance, the differences may be important when taking a population perspective.
In this study, women who were defined as voluntarily childfree had significantly lower levels of depressive symptoms than the reference population. Only 4% of the women in the voluntarily childfree subgroup scored above cut-off for case-level depression on HADS-D, as compared with 7% of mothers without infertility. It should be noted that the differences with regard to depression between this group of childfree women and the reference group may be due to differences in demographic profile and not due to fertility status per se: The women categorized as “voluntarily childfree” were younger and more frequently unmarried than the reference population of mothers without infertility. It may be that the women included in the “voluntarily childfree” subgroup had not yet considered pregnancy, and therefore these findings cannot be used to make firm conclusions about women who have deliberately chosen to stay childfree in the long run.
Strengths and limitations
The main strengths of this study were that it used a large population sample and that the valid subsample included 56% of the women aged 19–45 years available in the population. Consequently, the findings have a relatively high degree of generalizability, and the impact of potential response biases is reduced. Although the participation rate in the HUNT 2 study was high compared with many other epidemiological studies and the population of North-Trøndelag is stable and homogeneous with regard to sociodemographic factors, selection bias cannot be excluded. For instance, participants may have higher levels of education, better social support and lower frequency of co-morbid somatic or psychiatric conditions than non-participants. These are all factors that may confound the association between fertility problems and mental health [Citation20]. However, to minimize the potential effects of relevant confounding factors in this study, all analyses were adjusted for the effects of age, education, marital status, hypothyroidism, BMI and use of stimulants.
Fertility problems were self-reported, and this use of retrospective self-reports may reduce the internal validity of the study. Furthermore, neither items measuring fertility-specific distress [Citation18,Citation20] nor information about whether the respondent was actively trying to get pregnant, whether she self-identified as infertile, had undergone ART treatment or had adopted a child was included. Finally, levels of anxiety and depressive symptoms were assessed by means of a self-report instrument. However, this is regarded as a valid tool for measuring mental distress [Citation22,Citation23].
In conclusion, the contribution of infertility to symptoms of anxiety and depression is less pronounced in the general female population than among infertile women who are currently seeking medical help for it. Mean duration of infertility was long in this study, and the findings suggest that, from a longitudinal perspective and at the population level, unresolved infertility is not as burdensome as findings from clinical studies would suggest.
Many studies have shown that women seeking help for infertility have higher levels of anxiety and depression than women without infertility.
However, such clinical studies are subject to a wide range of biases that may affect the association between infertility and levels of mental distress.
The very few population-based studies that have assessed the association between infertility and mental health have yielded inconclusive results.
Current knowledge on the subject
Women with current primary or current secondary infertility have levels of anxiety and depression not significantly different from mothers without infertility.
At the population level, and from a longitudinal perspective, the mental burden of unresolved infertility is smaller than findings from studies on women seeking help for infertility would suggest.
What this study adds
Acknowledgements
The authors wish to thank the Nord-Trøndelag Health Study, which is a collaboration between the HUNT Research Centre (Faculty of Medicine, Norwegian University of Science and Technology, NTNU), Nord-Trøndelag County Council, Central Norway Health Authority and the Norwegian Institute of Public Health. The authors also acknowledge the services of the Medical Birth Registry of Norway (MBRN), and they thank Jörg Aβmus at the Centre for Clinical Research, Helse Bergen Local Health Authority for the categorization of variables from the MBRN.
Declaration of interest
The authors report no conflicts of interest.
R. S. is partly funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London.
References
- Drosdzol A, Skrzypulec V. Depression and anxiety among Polish infertile couples – an evaluative study. J Psychosom Obstet Gynecol 2009;30:11–120
- Galhardo A, Cunha M, Pinto-Gouveia J. Psychological aspects in couples with infertility. Sexologies 2011;20:224–8
- Greil A. Infertility and psychological distress: a critical review of the literature. Soc Sci Med 1997;45:1679–704
- Lechner L, Bolman C, van Dalen A. Definite involuntary childlessness: associations between coping, social support and psychological distress. Hum Reprod 2007;22:288–294
- Lykeridou K, Gourounti K, Deltsidou A, et al. The impact of infertility diagnosis on psychological status undergoing fertility treatment. J Reprod Infant Psychol 2009;27:223–37
- Souter V, Hopton J, Penney G, Templeton A. Survey of psychological health in women with infertility. J Psychosom Obstet Gynecol 2002;23:41–9
- Williams K, Marsh H, Rasgon N. Mood disorders and fertility in women: a critical review of the literature and implications for future research. Hum Reprod Update 2007;13:607–16
- Chachamovich J, Chachamovich E, Ezer H, et al. Investigating quality of life and health-related quality of life in infertility: a systematic review. J Psychosom Obstet Gynecol 2010;31:101–10
- Chachamovich J, Chachamovich E, Zachia S, et al. What variables predict generic and health-related quality of life in a sample of Brazilian women experiencing infertility? Hum Reprod 2007;22:1946–52
- Cousineau T, Domar A. Psychological impact of infertility. Best Practice Res Clin Obstet Gynaecol 2007;21:293–308
- Nelson C, Shindel A, Naughton C, et al. Prevalence and predictors of sexual problems, relationship stress, and depression in female partners of infertile couples. J Sex Med 2008;5:1907–14
- Volgsten H, Skoog Svanberg A, Ekselius L, Lundkvist Ö. Prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Hum Reprod 2008;23:2056–63
- Domar A, Zuttermeister P, Friedman R. The psychological impact of infertility: a comparison with patients with other medical conditions. J Psychosom Obstet Gynecol 1993;14:45–52
- Greil A, Slauson-Blevins K, McQuillan J. The experience of infertility: a review of recent literature Sociol Health Illness. 2010;32:140–62
- Boivin J, Bunting L, Collins J, Nygren K. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod 2007;22:1506–12
- Klemetti R, Raitanen J, Sihvo S, et al. Infertility, mental disorders and well-being – a nationwide survey. Acta Obstet Gynecol 2010;89:677–82
- Schmidt L. Social and psychological consequences of infertility and assisted reproduction – what are the research priorities. Hum Fertil 2009;12:14–20
- Greil A, McQuillan J, Lowry M, Shreffler K. Infertility treatment and fertility-specific distress: a longitudinal analysis of a population-based sample of U.S. women. Soc Sci Med 2011;73:87–94
- McQuillan J, Greil AL, White L, Jacob MC. Frustrated fertility: infertility and psychological distress among women. J Marriage Fam 2003;65:1007–18
- Jacob M, McQuillan J, Greil A. Psychological distress by type of fertility barrier. Hum Reprod 2007;22:885–94
- Mykletun A, Stordal E, Dahl A. Hospital Anxiety and Depression (HAD) scale: factor structure, item analyses and internal consistency in a large population. Br J Psychiatry 2001;179:140–4
- Zigmond A, Snaith R. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361–70
- Bjelland I, Dahl A, Haug T, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69–77
- Olssøn I, Mykletun A, Dahl A. The Hospital Anxiety and Depression Rating Scale: a cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry 2005;5:46
- Pal L, Bevilacqua K, Santoro NF. Chronic psychosocial stressors are detrimental to ovarian reserve: a study of infertile women. J Psychosom Obstet Gynecol 2010;31:130–9
- Sundby J, Schei B. Infertility and subfertility in Norwegian women aged 40–42. Prevalence and risk factors. Acta Obstet Gynecol Scand 1996;75:832–7
- Verhaak C, Smeenk J, Nahuis M, et al. Long-term psychological adjustment to IVF/ICSI treatment in women. Hum Reprod 2007;22:305–8
- Baldur-Felskov B, Kjaer SK, Albieri V, et al. Psychiatric disorders in women with fertility problems: results from a large Danish register-based cohort study. Hum Reprod 2013;28:683–90
- Peterson B, Pirritiano M, Christensen U, et al. The longitudinal impact of partner coping in couples following 5 years of unsuccesful fertility treatments. Hum Reprod 2009;24:1–9
- Verhaak C, Smeenk J, Evers A, et al. Women's emotional adjustment to IVF: a systematic review of 25 years of research. Hum Reprod Update 2007;13:27–36
- Wirtberg I, Möller A, Hogström L, et al. Life 20 years after unsuccessful infertility treatment. Hum Reprod 2007;22:598–604
- Hammarberg K, Fisher JRW, Wynter KH. Psychological and social aspects of pregnancy, childbirth and early parenting after assisted conception: a systematic review. Hum Reprod Update 2008;14:395–414
- Puhan M, Frey M, Buchi S, Schünemann HJ. The minimal important difference of the hospital anxiety and depression scale in patients with chronic obstructive pulmonary disease. Health Qual Life Outcomes 2008;6:46