Abstract
Objective: This paper investigates the effectiveness of high-intensity focused ultrasound (HIFU) for treating non-neoplastic epithelial disorders of the vulva (NNEDV) and to analyse the factors that affect the effectiveness of HIFU and recurrence. Methods: This study included a total of 950 patients with pathologically confirmed NNEDV, who underwent HIFU treatment in our hospital between August 2008 and June 2013 and had completed follow-up data. Treatment efficacy and recurrence were evaluated retrospectively by analysing the patients’ clinical pathological data and by following up their symptomatic changes. We also explored factors including age, status of menopause, HPV infection, lesion size, pathological type, and symptom severity for their correlation with treatment effectiveness and recurrence. Results: HIFU was effective in alleviating symptoms and improving vulva signs, with a cure rate of 42.2%, an effective rate of 56.1%, and a low recurrence rate of 9.4%. No severe complications were recorded during or after the treatment. The treatment was statistically more effective in younger patients with squamous hyperplasia and smaller lesions than in older patients with lichen sclerosus and larger lesions (P < 0.05). Patients with a longer disease course or with lichen sclerosus had significantly higher recurrence rates than those with a shorter disease course or with squamous hyperplasia (P < 0.05). Conclusions: HIFU is safe and effective in treating NNEDV. Its effectiveness is correlated with age, size of lesion and pathological type, whereas post-treatment recurrence rates may be related to the duration of the disease and the pathological sub-types.
Introduction
Non-neoplastic epithelial disorders of the vulva (NNEDV) are grouped under the common term vulva skin disease. In 1987 the International Society for the Study of Vulva Disease (ISSVD) classified the disease into two major pathological types: squamous hyperplasia (SH) and lichen sclerosus (LS), both with high incidence rates [Citation1]. NNEDV have been regarded as ‘refractory diseases’ featuring prolonged course, severe symptoms, refractoriness to treatments and high recurrence rates. Since high intensity focused ultrasound (HIFU) was first applied to treat NNEDV in 1999, it has been increasingly used for treating this condition [Citation2]. While a number of studies have demonstrated the safety and effectiveness of HIFU for the treatment and management of NNEDV [Citation3–5], few of them have focused on factors that correlate with the effectiveness of HIFU and recurrence of the disease.
We have treated more than 2000 NNEDV patients since 2006. In this retrospective study we included 950 patients who were diagnosed with SH or LS and treated with HIFU between August 2008 and June 2012. A retrospective analysis of their clinico-pathological and post-HIFU treatment follow-up data was conducted to identify factors that significantly correlate with treatment effectiveness or disease recurrence.
Materials and methods
Baseline information of patients
Between August 2008 and June 2012, 950 patients were diagnosed with squamous hyperplasia (SH) or lichen sclerosus (LS) and were treated with HIFU in our hospital with complete follow-up data. The mean age of these patients was 42.5 ± 13.0 years and the median course of the disease was 5.4 ± 5.6 years. Inclusion criteria for patients were (1) colposcopy examinations and multi-site biopsies meeting the ISSVD 1987 diagnostic standard and ruling out vulva carcinoma or precancerous lesions, (2) having no serious heart, liver or kidney diseases nor uncontrolled diabetes, (3) having no hormone medication or physiotherapies 3 months before HIFU treatment, (4) not having acute genital inflammation, menstruation, gestation or lactation, and (5) having no other on-going therapies during HIFU treatment.
Treatment protocol
Before HIFU treatment all patients were asked about their medical history, and gynaecological examination, vulva colposcopy, and biopsy were conducted to make the final diagnoses of NNEDV. The treatment was performed at 3–7 days after the completion of menstruation and when the biopsy wound had healed. The bladder was emptied and the skin prepared preoperatively. Patients were placed in bladder lithotomy position during the operation, and 0.5% povidone iodine solution was used for routine vulva skin disinfection before draping. Then 0.5% lidocaine was used for local infiltration anaesthesia. Thereafter, all the patients were treated with a model CZF-focused ultrasound therapeutic device developed by Chongqing Haifu Medical Technology, Chongqing, China. The treatment parameters were: power 3.5–4 W, frequency 9.4 MHz, pulse 1000 Hz. The probe was in close contact with the skin above the lesion via an ultrasound couplant. A consecutive scanning at a speed of 3–5 mm/s was performed on the lesion area and healthy tissues 5 mm around that area. The scanning lasted for a period of 8–40 min until the treatment area showed mild congestion, swelling, and hyperthermia, while the wrinkled or depressed area became flat and smooth. For post-treatment management, the patient’s vulva was sterilised again with Iodophor, and moist burn ointment was applied locally for a week. During the 24 h after treatment, ice packs were intermittently applied on affected skin (5 min ice application, 5 min break).
Follow-ups and evaluation of effectiveness of HIFU treatment
Patients were followed up on a regular basis after treatment to observe the effectiveness, side effects of the treatment, and recurrence of the lesion. One week after treatment, outpatient follow-ups were made to monitor relief of symptoms and local complications. Outpatient check-ups were done in 1 month, 3 months and 6 months after the treatment. In the first 3 years after treatment, patients were examined every 6 months. After 3 years, patients were examined once a year. Follow-ups included inquiry about symptom relief and gynaecological examinations to identify changes in lesion areas, skin colour and elasticity. Some patients had colposcopy examinations and biopsies again 3 months after treatment.
Based on changes in the degrees of symptoms severity and local skin signs (lesion size, skin colour and elasticity) before and after treatment, treatment effectiveness on each patient was assessed using the following criteria [Citation6]. (1) Curative: symptoms such as vulva pruritus disappeared, skin colour and elasticity of the diseased area became normal, (2) effective: symptoms such as vulva pruritus and causalgia decreased, vulva skin colour and elasticity partially recovered, (3) ineffective: symptoms such as vulva pruritus continued and signs of local skin did not change, or such signs and symptoms recurred within 6 months after treatment, (4) recurrent: symptoms such as vulva pruritus and pain recurred, vulva skin depigmented and elasticity decreased 6 months after treatment.
Statistical analysis
Statistical analysis was performed with SAS version 9.2. The patients were grouped by median age and the course of disease. Measurement data and quantitative data are described by mean value (standard deviation) and frequency, respectively. Single factor analysis of effectiveness was performed with non-parametric rank sum test, while single factor analysis of recurrence was performed with chi-squared test or Fisher’s exact test. Variables of statistical significance in single factor analysis were then incorporated into a logistic regression model for multiple factor analysis, where multiple factor analysis of effectiveness was performed with the ordinal logistic regression model while multiple factor analysis of recurrence was performed with the dichotomy regression model. P < 0.05 was defined as a statistically significant difference for two-sided test.
Results
Effectiveness of HIFU treatment for NNEVD
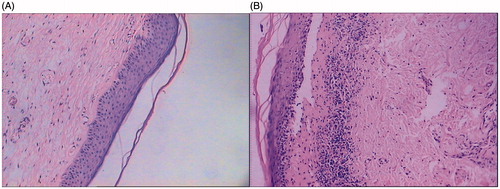
Out of 950 patients, curative response, judged by the complete disappearance of symptoms and signs, was observed in 401 (42.4%) patients. Post-operative skin biopsies, performed on a subset of patients, suggested recovery of ultrastructures (). Effective response, judged by improvement of symptoms and signs, was observed in 533 (56.1%) patients, some of whom underwent vulvar biopsies which demonstrated repair of the dermal structure, decreased inflammatory cell infiltration, and increased vascularisation. Only 16 patients (1.7%) showed no improvement, thus were non-responsive. HIFU was ineffective for a small fraction of NNEVD in our cohorts.
Figure 1. Pathological features of SH before and after HIFU treatment. (A) SH before treatment, squamous epithelial cell proliferation, extended epithelial ridges, excessive cornification in epidermis, thickened prickle cell layers, and various degrees of lymphocytes infiltration. (B) SH after treatment, the cornification of epithelial cells and the structure of the prickle cell layer are normalised. HE (hematoxylin-eosin staining) 100 × diseased tissues.
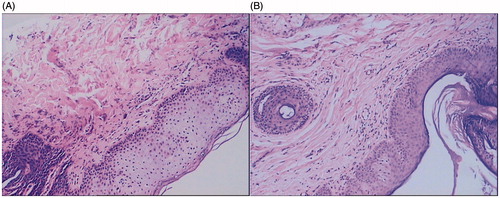
Figure 2. Pathological features of LS before and after HIFU treatment. (A) LS before treatment, squamous epithelium is thin, epithelial ridge becomes blunt or disappeared; cornification appears in epidermis, the superficial layer of dermis develops oedema, and fibrous tissue shows hyperplasia and glassy degeneration. (B) LS after treatment, the epithelium is thickened, epithelial ridges become obvious, and number of inflammatory infiltrated cells has decreased. HE (hematoxylin-eosin staining) 100 × diseased tissues.
Of all the effective cases, 89 cases (9.5%) recurred, among which 18 patients developed recurrence within the first year after treatment, 29 developed recurrence in the second year, 27 in the third year, 10 in the fourth year, and 4 developed recurrence more than 4 years later after the treatment.
Immediately after treatment, the treated areas of nearly all patients showed varied degrees of swelling and congestion. Blisters developed in 97 (10.2%) patients, scleroma developed in three patients. Examinations taken 1 week after treatment found 29 (3.1%) patients with ulceration, among whom one had cellulitis because of serious infection and another had post-operative bleeding. All cases improved after symptomatic treatment.
Single factor analysis of the effectiveness of HIFU treatment for NNEVD and recurrence
In order to look into the prognostic factors, the patients were analysed based on (1) age: ≤42 years and >42 years, (2) disease course: ≤3 years and >3 years, (3) menopause status: with and without, (4) HPV infection status: with and without, (5) lesion size: three groups with pre-treatment percentages of vulva lesion size of <30%, 30–50%, and >50%, respectively, (6) pathological sub-types: SH and LS, (7) severity of symptoms: mild, moderate and severe symptoms.
As shown in , whereas the response to HIFU in 231 (46.9%) cases in the group ≤42 years were curative and 255 (51.7%) were effective; 170 (37.2%) cases in the group >42 years were curative and 278 (60.8%) were effective. The treatment effective rate in patients ≤42 years was significantly higher than that in patients >42 years (P = 0.003). The effective rate was found to be higher in pre-menopausal patients than in post-menopausal patients (P = 0.011), higher in the SH group than in the LS group (P = 0.012), and also higher in patients with smaller lesions. Disease course, HPV infection, and severity of pre-treatment symptoms were not independent prognostic factors for the effectiveness of HIFU.
Table 1. Single factor analysis of the effectiveness of HIFU treatment for NNEVD.
The recurrence rate was 11.4% in patients with a course of >3 years, significantly higher than in those with a course of ≤3 years (P = 0.029). The recurrence rate was higher for LS cases than for SH cases (P = 0.015). Thus, the disease course and the pathological subtypes appear to be independent prognostic factors for predicting recurrence. In contrast, other factors including age, status of menopause, concurrent HPV infection, the size of the lesion and severity of pre-treatment symptoms were not independent prognostic for predicting recurrence ().
Table 2. Single-factor analysis of the recurrence of HIFU treatment for NNEVD.
Multiple factor analysis of treatment effectiveness and recurrence
Logistic regression multi-variant analysis was conducted using the individual prognostic factors (age, status of menopause, pathological sub-types, lesion size) identified in the single factor analysis for treatment effectiveness. The analysis showed that age, lesion size, and pathological type were all prognostic factors for effectiveness. Older patients with larger lesions and LH pathological type showed less satisfactory treatment effectiveness (P < 0.05) ().
Table 3. Multi-variant analysis of the effectiveness of HIFU treatment for NNEVD.
Similarly, multi-variant analysis was performed on individual prognostic factors identified in the single factor analysis for recurrence. The analysis revealed that the disease course and pathological type are both prognostic risk factors for recurrence. Patients with longer course and LH type had higher recurrent risks (P < 0.05) ().
Table 4. Multiple variant analysis of recurrence after HIFU treatment for NNEDV.
Discussion
Management of NNEDV
NNEDV belong to a group of common chronic vulvar skin diseases, with a reported morbidity of 1/300∼1/1000 [Citation7]. Characteristic symptoms include vulvar pruritus, pain, causalgia, or even dyspareunia during sex. Typical gynaecological examination findings demonstrate varying degrees of vulvar skin depigmentation that is often accompanied by coarsening skin, vulvar dystrophies, and rhagades [Citation8,Citation9]. Pathological changes in SH subtype of NNEDV include squamous epithelial cell proliferation, extended epithelial ridges, excessive cornification in the epidermis, thickened prickle cell layers, and various degrees of lymphocytes infiltration. In the LS subtype of NNEDV, however, squamous epithelial cells become thin, the epithelial ridge becomes blunt or disappeared, cornification appears in the epidermis, the superficial layer of the dermis develops oedema, and fibrous tissue shows hyperplasia and glassy degeneration [Citation10]. Studies have shown that NNEDV patients with long disease course and severe symptoms are more likely to suffer from depression or anxiety [Citation11]. NNEDV are detrimental to women’s physical and mental health. Up till now, the underlying mechanism for the pathogenesis of NNEDV is thought to be related to immunity, infection, hormone, or genetic factors [Citation12–14], yet the exact cause remains to be identified. Consequently, effective treatment of NNEDV has been a clinical challenge. Conventional medications such as local application of hormone medication, traditional Chinese medicine bathing therapy, or physical therapies such as laser therapy, cryotherapy, and bomu light treatment, have been found to be effective to a certain degree, but are associated with high recurrence rates [Citation15].
Ultrasound beam therapy can generate cavitation, thermal, mechanical and other biological effects. With the characteristics of precise positioning, non-invasiveness, and non-irradiation damage, focused ultrasound energy can be directed onto a targeted area inside the body [Citation16]. As a new non-invasive modality, HIFU has been used for, but not limited to the treatment of benign and malignant tumours. In recent years it has been increasingly used in the field of gynaecology and obstetrics, including HIFU ablation for hysteromyoma and adenomyoma, chronic cervicitis, and NNEDV [Citation17].
We reported here through a retrospective analysis that of the 950 cases treated with HIFU, the curative rate and effective rate were 42.4% and 56.1%, respectively, while the recurrence rate was as low as 9%. Incidence of major post-operative complications was rare. These observations collectively demonstrate that HIFU treatment is a new, safe, and effective treatment for NNEDV. The result is attributable to the features of NNEDV and the way HIFU works. Recent studies have discovered that microvessels in the local dermis are reduced or obstructed in NNEVD, causing local microcirculation disturbance and epithelial disorders at different levels [Citation18]. The lesions, seeming to be epidermis depigmentation, are actually disorders in the dermis, primarily vascular disorders in the dermal layer. Conventional medications or other physical therapies cannot reach the dermal layer or go deep enough without damaging the epidermal layer. Ultrasound beam therapy, on the other hand, can be accurately directed and targeted at lesions in the dermis without causing damage to the surrounding epidermal tissues. Additionally, HIFU may facilitate local vascularisation, increase permeability of capillaries, and improve nutrition in capillaries and nerve endings [Citation3].
Single factor analysis and multi-variant analysis have shown that the effectiveness of HIFU treatment for NNEDV was related to age and the size of lesions. The efficacy was significantly higher in younger patients with smaller lesions than in older patients with larger lesions. The younger patients had stronger local immunity and better vulva regenerative capability, which might contribute to the more rapid alleviation of symptoms and signs after treatment [Citation19]. For patients with larger lesions, reduced treatment effectiveness could be attributed to two reasons. First, because the treatment time was limited, lesion areas received relatively small doses of ultrasound per unit. Second, patients with large lesions often had lesions growing in the wrinkled parts such as the clitoris and crissum, where even distribution of a therapeutic dose of HIFU would be difficult.
We also found that the course of disease was not significantly related to treatment effectiveness but was a prognostic factor for recurrence. Patients with longer courses of disease had significantly higher recurrence rate than those with shorter courses. The statistical results showed that although the course of the disease is not prognostic for treatment efficacy, it is perplexing that the trend was that the effective rate was higher while the curative rate was lower in patients with longer courses than those in patients with shorter courses. This is probably because patients with longer courses had more severe symptoms and local signs, which were relatively easier to relieve but harder to cure, thus more likely to recur.
Our study also found that LS patients had a lower effective rate but higher recurrence rate than SH patients. This could be attributed to the fact that in LS cases, the epithelium became atrophied and thin, and blisters and scleromas tended to develop. Therefore the treatment power had to be lowered and treatment duration had to be shortened, leading to undesirable ‘under-treatment’. Since LS and SH patients differ in clinical signs and pathological features, and their pathogeneses remain unknown, whether such factors are relevant to effectiveness and recurrence warrants further study.
Conclusions
In conclusion, HIFU is a safe and effective therapy that has curative potential and causes low recurrence rate for NNEDV. In our analyses we have identified that age, size of lesion, and pathological type are prognostic factors for predicting the effectiveness or recurrence of HIFU treatment for NNEDV. These findings prompt us to improve HIFU clinical protocols and to search for new complementary approaches to achieve higher efficacy and to reduce disease recurrence. Future clinical studies are warranted.
Acknowledgements
We thank Wenyi (Wendy) Zhang at Marshall College of University of California, San Diego for providing language help and writing assistance.
Declaration of interest
The authors have no potential conflicts of interest to disclose. The authors alone are responsible for the content and writing of the paper.
References
- Ridley CM, Frankman O, Jones IS, Pincus SH, Wilkinson EJ, Fox H, et al. New nomenclature for vulvar disease: International Society for the Study of Vulvar Disease. Hum Pathol 1989;20:495–6
- Wang ZB. High-intensity focused ultrasound in obstetrics and gynecology. Chinese J Gynaecol Obstet 2003;38:510–12
- Li C, Bian D, Chen W, Zhao C, Yin N, Wang Z. Focused ultrasound therapy of vulvar dystrophies: A feasibility study. Obstet Gynecol 2004;104:915–21
- Ruan L, Xie Z, Wang H, Jiang J, Shi H, Xu J. High-intensity focused ultrasound treatment for non-neoplastic epithelial disorders of the vulva. Int J Gynaecol Obstet 2010;109:167–70
- Jiao LX, Hu LN, Xiong ZA, Feng LH, Zhang Y, Tian GB. High intensity focused ultrasound for the treatment of 900 cases of non-neoplastic epithelial disorders of vulva. Chinese J Gynaecol Obstet 2007;42:6–8
- Cattaneo A, Bracco GL, Maestrini G, Carli P, Taddei GL, Colafranceschi M, et al. Lichen sclerosus and squamous hyperplasia of the vulva. A clinical study of medical treatment. J Reprod Med 1991;36:301–5
- Shirer JA Jr, Ray MC. Familial occurrence of lichen sclerosus et atrophicus: Case reports of a mother and daughter. Arch Dermato 1987;123:485–8
- O’Donnell TX, Nathan LS, Satmary WA, Goldstein AT. Non-neoplastic epithelial disorders of the vulva. Am Fam Physician 2008;77:321–6
- Mac Bride MB, Rhodes DJ, Shuster LT. Vulvovaginal atrophy. Mayo Clinic Proc 2010;85:87–94
- Sander CS, Ali I, Dean D, Thiele JJ, Wojnarowska F. Oxidative stress is implicated in the pathogenesis of lichen sclerosus. Br J Dermatol 2004;151:627–35
- Van de Nieuwenhof HP, Meeuwis KA, Nieboer TE, Vergeer MC, Massuger LF, De Hullu JA. The effect of vulvar lichen sclerosus on quality of life and sexual functioning. J Psychosom Obstet Gynaecol 2010;31:279–84
- Tchórzewski H, Rotsztejn H, Banasik M, Lewkowicz P, Głowacka E. The involvement of immunoregulatory T cells in the pathogenesis of lichen sclerosus. Med Sci Monit 2005;11:CR39–43
- Ueda Y, Enomoto T, Miyatake T, Shroyer KR, Yoshizaki T, Kanao H, et al. Analysis of clonality and HPV infection in benign, hyperplastic, premalignant, and malignant lesions of the vulvar mucosa. Am J Clin Pathol 2004;122:266–74
- Gao XH, Barnardo MC, Winsey S, Ahmad T, Cook J, Agudelo JD, et al. The association between HLA DR, DQ antigens, and vulval lichen sclerosus in the UK: HLA DRB112 and its associated DRB112/DQB10301/04/09/010 haplotype confers susceptibility to vulval lichen sclerosus, and HLA DRB10301/04 and its associated DRB10301/04/DQB10201/02/03 haplotype protects from vulval lichen sclerosus. J Invest Dermatol 2005;125:895–9
- Cattaneo A, Bracco GL, Maestrini G, Carli P, Taddei GL, Colafranceschi M, et al. Lichen sclerosus and squamous hyperplasia of the vulva. A clinical study of medical treatment. J Reprod Med 1991;36:301–5
- Poissonnier L, Chapelon JY, Rouvière O, Curiel L, Bouvier R, Martin X, et al. Control of prostate cancer by transrectal HIFU in 227 patients. Eur Urol 2007;51:381–7
- Zhang L, Zhang W, Orsi F, Chen WZ, Wang ZB. Ultrasound-guided high intensity focused ultrasound for the treatment of gynaecological diseases: A review of safety and efficacy. Int J Hyperthermia 2015;31:280–4
- Kim YS, Rhim H, Choi MJ, Lim HK, Choi D. High-intensity focused ultrasound therapy: An overview for radiologists. Korean J Radiol 2008;9:291–302
- Powell J, Wojnarowska F. Childhood vulvar lichen sclerosus: An increasingly common problem. J Am Acad Dermatol 2001;44:803–6
