Abstract
Purpose: The aim of this study was to explore whether doxorubicin hydrochloric (DOX) combined with microwave ablation (MWA) is more effective at increasing tumour coagulation and prolonging end-point survival in a VX2 rabbit breast cancer model than each intervention individually.
Methods: New Zealand white rabbits with VX2 tumours were placed into treatment groups as follows: MWA (20 W for 5 min and 40 W for 5 min), intravenous injection of 4 mg/kg DOX, and combined therapy. Tumours were analysed at 4 h and 24 h after treatment to determine the temporal quantities of cleaved caspase-3 and Hsp70 using immunohistochemical staining and Western blots. Tumour coagulation areas were compared at 24 h after treatment.
Results: No significant difference in tumour coagulation was found between DOX-MWA and 40W-MWA (mean 4.52 cm2 ± 0.48 (SD), 4.08 cm2 ± 0.36, respectively; P > 0.05). A significant difference between tumour coagulation was found for DOX-MWA and 20W-MWA (mean 4.52 cm2 ± 0.48 (SD), 1.69 cm2 ± 0.34 cm2, respectively; p < 0.01). Cleaved caspase-3 and Hsp70 demonstrated low level expression at 4 h and 24 h in the DOX group. Cleaved caspase-3 showed low expression at the coagulation margin in the 20W-MWA group, was highly expressed in DOX-MWA group, and continued to increase with time. Hsp70 in the 20W-MWA group increased significantly at the coagulation margin but demonstrated low expression in the DOX-MWA group at 4 h and 24 h. The animals in the combined treatment group had a longer survival time (mean 78.33 days ± 8.07 SD) than the 20W-MWA group (mean 57.17 days ± 8.77, p < 0.01) or the DOX group (mean 35.17 days ± 7.63, p < 0.01).
Conclusion: A combination of DOX and MWA could increase tumour coagulation and end-point survival better than single therapy, which had some connection with the elevated expression of cleaved caspase-3 and low Hsp70 expression at the coagulation margin.
Introduction
The incidence of breast cancer tops the list of female malignant tumours, which exerts a significant negative impact on the overall health of women [Citation1]. Due to the special nature of breast tissues, the heterogeneity in breast cancer leads to a high degree of diversity among cancer patients, bringing great challenges to breast cancer research and therapy.
Microwave ablation (MWA), a hyperthermia treatment, has demonstrated unique advantages in experimental studies and clinical application of tumours. MWA has proven safe and efficient in breast cancer (≤3 cm) [Citation2]. However, when the tumour size is larger than 3 cm, or the tumour’s distance from the skin and (or) chest wall is smaller than 1 cm, damage to the surrounding soft tissues will limit the microwave effect. In addition, neoadjuvant chemotherapy, as an effective method for breast cancer, also poses some issues in clinical application, such as incomplete regression and a longer chemotherapy cycle. Therefore, there is more controversy than consensus regarding neoadjuvant chemotherapy [Citation3]. Tumour death can be enhanced when combining radiofrequency ablation (RFA) with adjuvant chemotherapy or radiosensitisers over non-thermal therapy alone [Citation4–6].
However, RFA results in coagulant necrosis only within a few millimetres of the probe. Deposition of heat into the surrounding tissue is not only limited by the inherent thermal conductivity of the tissue but also the development of carbonisation providing further resistance to heat transfer. MWA is different from RFA as it does not require a current loop. Consequently, the limitations of thermal conduction are not as severe compared with RFA. This results in better heating, a larger heated volume, and less damage to the adjacent vessels from heatsink [Citation7,Citation8].
This experiment aims to explore the efficacy of MWA combined with doxorubicin hydrochloric (DOX) versus the single use of each in increasing tumour necrosis and prolonging animal survival time. In addition, the study aims to identify a new path for neoadjuvant chemotherapy by making full use of the minimally invasive advantages of MWA.
Adriamycin has been the first-line medication for solid tumours and also has good efficacy in treating breast cancer. This study investigated the combination of DOX and MWA in treating a rabbit VX2 transplantation cancer model and analysed whether MWA combined with DOX could increase tumour coagulation and end-point survival of these animals.
Materials and methods
Animal model
The protocol was approved by the Institutional Animal Care and Use Committee of Nanjing Medical University. Female New Zealand white rabbits (age range 12–14 weeks), weighing between 2.0 and 2.5 kg, were used in this study. The VX2 cell line used for tumour implantation, provided by W.Z., was obtained from the Surgery Department of the First Affiliated Hospital of Nanjing Medical University. For all experiments and procedures, anaesthesia was induced by using an intravenous injection of pentobarbital (30 mg/mL, 0.8 to 1.2 mL/kg, pentobarbital sodium; Sigma, St Louis, MO, USA). All animal studies were performed by trained researchers using US-guided MWA techniques (ECO-100A, NanjingYigao, China). The required tumour tissue, taken from a tumour carrier rabbit, was cut into small strips (1.5 × 1.5 × 6 mm). Under direct visualisation, 0.2–0.3 mL of the tumour suspension was injected slowly with a 16-gauge needle subcutaneously into the mammary fat pad underneath the right second nipple [Citation9]. Animals were monitored, and the tumour diameter was measured every 3–4 days. Tumours grew for 3-4 weeks until the desired treatment size was achieved. Solid non-necrotic tumours (as determined with ultrasonography) measuring 3.0–3.5 cm in diameter were used in this study. Animals that refused solid and fluid intake for more than four days with concomitant apathy and weight loss of more than 20% were sacrificed for ethical reasons [Citation10,Citation11,Citation12].
MWA application
In a manner similar to prior experiments [Citation2,Citation9], a 2450-MHz MWA generator (ECO-100A) was used to apply monopolar MWA. Output powers of 20 W and 40 W were chosen for this study. After testing the cold water (4 °C) cycling system, the percutaneous microwave coagulation (PMC) procedure continued for 5 min to eradicate the majority of tumours according to the pilot study.
After MWA treatment the antenna was removed and the incision closed. All rabbits were monitored for 2–3 months after surgery to avoid any complications caused by the intervention. The degree and extent of skin burning were evaluated. Weight and food intake were monitored, and behaviour after treatment was observed.
Experimental groups
The longest and shortest tumour diameters were measured using calipers. When the longest tumour diameter reached approximately 30 mm (18 to 30 days), 74 rabbits were chosen and randomly divided into five groups as follows: (1) control group, eight rabbits served as un-treated controls (two for immunohistochemical (IHC) staining), (2) DOX group (n = 18): doxorubicin hydrochloric (4 mg/kg) was injected through the ear vein [Citation13], (3) 20W-MWA group (n = 18), guided by ultrasound, an output power of 20 W was used along the tumour’s long axis for 5 min, (4) 40W-MWA group (n = 12), an output power of 40 W was used for 5 min, (5) DOX-MWA group (n = 18), combination treatment group with doxorubicin hydrochloric (4 mg/Kg) injected 24 h after 20W-MWA treatment, (6) in groups except the 40W-MWA group, under aseptic conditions, tumours of six rabbits were taken out at 4 h and 24 h to detect immunohistochemistry (IHC) staining of cleaved caspase-3 and Hsp70. End-point survival for the remaining six rabbits in each group was observed using the Kaplan-Meier test.
Measuring and calculating necrosis range
Tumour specimens taken at 24 h after treatment were dissected along the long axis of the probe to create thin tissue sections, which were incubated in 2% 2,3,5-triphenyltetrazolium chloride for 30 min [Citation14]. The extent of tissue necrosis was evaluated by assessing mitochondria enzyme activity. It is the viable tissue with intact mitochondrial enzyme activity, not the ablated tissue that turns red after staining [Citation15]. The extent of visible coagulation was measured in two separate and perpendicular dimensions with calipers. The coagulation diameter (i.e. longest measurement perpendicular to the inserted electrode) in all tissue samples was determined in a blinded fashion. Two pathologists with no knowledge of this trial performed the measurements. The necrosis range was calculated using the formula S = л¼ab.
IHC staining
All specimens were fixed in a 10% formalin solution, embedded in paraffin and stained with haematoxylin and eosin (H&E) and IHC. Ten visual fields with clear background and staining under light microscope with 100× magnification were randomly selected and examined. The protein immune activity was evaluated by both the extent and intensity of staining. The staining extent was scored as follows: 0 = no positively stained cells, 1 = < 25% of the cells were stained, 2 = 25–50% of the cells were stained, 3 = 50–75% cells were stained, and 4 = > 75% cells were stained. The staining intensity was scored as follows: 0 = no positive staining, 1 = weak positive staining, 2 = moderate positive staining, and 3 = strong positive staining. The comprehensive score was achieved by multiplying the staining extent and staining intensity scores. We define IHC scores as follows: 0 = negative staining, 1–3 = weak positive staining, 4–5 = positive staining, and > 6 = strong positive staining. The IHC staining procedure was strictly controlled according to the reagent kit instructions. All IHC staining specimens were analysed, observed and evaluated by two pathologists.
Western blots
Western blotting was performed as described previously [Citation16]. Briefly, equal amounts of protein isolated from the coagulation margin of tumour tissues were loaded onto a 10% SDS-PAGE gel and transferred to PVDF membranes (Amersham Pharmacia Biotech, Piscataway, NJ, USA). The membranes were incubated with antibodies against cleaved caspase-3 and Hsp70 (1:1000 dilution;Cell Signaling Technology, Danvers, MA, USA). Beta-actin (1:10000 dilution; Sigma-Aldrich, St. Louis, MO, USA) antibody was used to confirm that the protein loading among samples was equal. The signals were detected with the Enhanced Chemiluminescence (ECL) system (West Pico kit; Pierce, Loughborough, UK), and band density was analysed using Image J software (National Institutes of Health, Bethesda, MD).
Survival observation
Local changes in tumours and the severity of scalds on the skin were observed. The changes in tumour diameters were monitored weekly and animal survival time was recorded. The humane endpoint was defined by a >50% decrease in food intake and >20% loss in body weight. The animals were then humanely euthanised by an overdose injection of 3% pentobarbital solution (>3 mL/kg) via the ear vein [Citation10,Citation11,Citation12].
Statistical analysis
Software (SPSS 16.0, Chicago, IL) was used for statistical analysis in the current study. All statistics are shown as the means ± standard deviation. Student’s t-test was used to compare the tumour necrosis ranges and the long diameters after 3 weeks of treatment. The Kaplan-Meier method was used for the end-point survival analysis. Results with P values less than 0.05 were considered significant.
Results
The necrosis range in the combination group was larger than the other groups
Our results demonstrated that there was no significant difference in tumour coagulation between the DOX-MWA and 40W-MWA groups (mean 4.52 cm2 ± 0.48 (SD), 4.08 cm2 ± 0.36, respectively; p > 0.05). DOX-MWA increased tumour coagulation over 20W-MWA (mean 4.52 cm2 ± 0.48 (SD), 1.69 cm2 ± 0.34, respectively; p < 0.01). The control group specimens were brittle and fish-meat-like, with no necrotic foci. In the DOX group one of the specimens had a necrotic range of 1.00 cm × 0.60 cm, and multiple spotty necrosis areas appeared in all the other specimens.
Expression of apoptosis and Hsp70 production
Our results demonstrated low expression of cleaved caspase-3 and Hsp70 at 4 h and 24 h in the DOX group. Cleaved caspase-3, which demonstrated low expression at the coagulation margin in the 20W-MWA group, was highly expressed in the DOX-MWA group with a continuous increase at 24 h. Hsp70 increased significantly in the 20W-MWA group, and always exhibited low expression in the DOX-MWA group at 4 h and 24 h (, , ).
Figure 1. IHC staining of Caspase-3 ×100 ACEG took place at the 4 h time point after treatment, and BDFH staining at the 24 h time point. (A, B) Negative expression of cleaved caspase-3 in the control group. (C, D) Weak positive cleaved caspase-3 expression in the necrotic region of the DOX group. (E, F) Weak positive cleaved caspase-3 expression at the coagulation margin of the 20W-MWA group. (G, H) Positive cleaved caspase-3 expression at 4 h and a strong positive expression at 24 h at the coagulation margin in the DOX-MWA group.
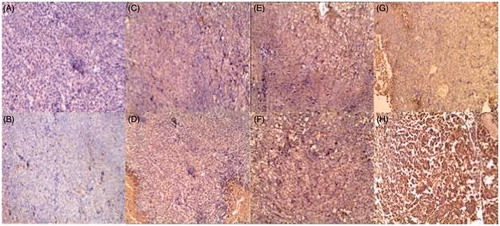
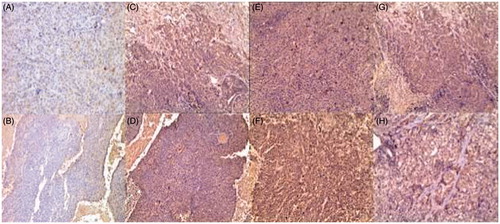
Figure 2. IHC staining of Hsp70 × 100 ACEG took place at the 4 h time point after treatment, and BDFH staining at the 24 h time point. (A, B) Negative Hsp70 expression in the control group. (C, D) Weak positive Hsp70 expression at the necrotic region of the DOX group. (E, F) Positive Hsp70 expression at 4 h and a strong positive expression at 24 h at the coagulation margins of the 20W-MWA group. (G, H (Weak Hsp70 expression in the DOX-MWA group.
Survival observation
Mean and median survival time for rabbits that received both DOX and MWA were longer (mean and median, 78.33 days ± 8.07 and 18 days, respectively) than those that received 20W-MWA alone (mean and median, 57.17 days ± 8.77 and 57 days, respectively), those that received DOX alone (mean and median, 35.17 days ± 7.63 and 33 days, respectively), or those in the control group (mean and median, 30.50 days ± 4.76 and 31 days, respectively; p < 0.01, all comparisons) (). The Kaplan-Meier survival curve showed that the survival time of rabbits in the DOX-MWA group was significantly longer than those in all other groups (
Figure 3. Expressions of Hsp70 and cleaved caspase-3 at 4 h and 24 h after treatment. Western blot results of (A) Hsp70, and (B) cleaved caspase-3 at the coagulation or necrosis margins of the tumour tissues. Significant differences in the relative intensity of Hsp70 and cleaved caspase-3 were detected between the DOX group and 20W-MWA and DOX-MWA groups. The results are displayed as the mean, and the error bars denote SD; n = 6 for each group; p < 0.05. Significant differences in Hsp70 and cleaved caspase-3 were detected between the 20W-MWA and DOX-MWA groups at 24 h after treatment. The DOX-MWA level of Hsp70 was lower than 20W-MWA at 24 h after treatment; however, the DOX-MWA levels of cleaved caspase-3 were significantly higher. *p > 0.05; **p < 0.05; ***p < 0.01.
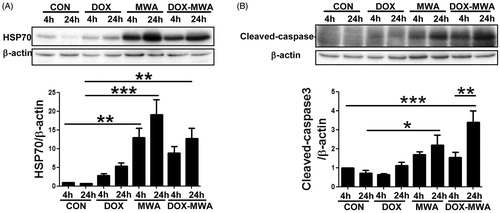
Figure 4. Kaplan–Meier analysis of end-point survival following treatment with MWA and/or IV DOX. Survival end-point signifies the time when the animal refused solid and fluid intake for more than 4 days with a weight loss of more than 20%. The greatest end-point survival was observed with combined therapy, using DOX and MWA. In addition, improved survival was noted in the 20W-MWA group, compared to the DOX group or control group.
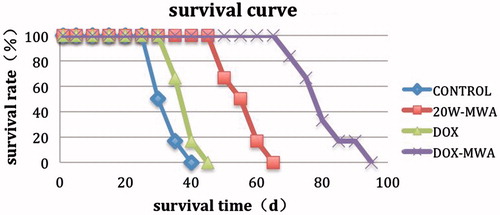
Table 1. Survival time of rabbits in the four groups.
The rank sum test was used to analyse the survival time of rabbits in all groups. The DOX-MWA group had the longest survival time. Compared with the other three groups, the DOX-MWA group demonstrated significant differences (**p < 0.01). There was also a significant difference between the 20W-MWA group and the DOX-MWA group (ap < 0.01). The survival time in the DOX-MWA group was longer than in the 20W-MWA group. In contrast, the survival times between the control group and the DOX group were not significantly different (p > 0.05). In the 40W-MWA group, serious injuries and infection occurred. Within 2 weeks of the treatment, animals were sacrificed with excessive anaesthetic.
Hyperthermia vice injury
In this study, two rabbits in the 20W-MWA group experienced skin swelling. In one rabbit, swelling gradually faded over 3 days, and the other rabbit developed ulcers on day 3, with a maximum diameter of 0.8 cm. With disinfection and treatment with Kangfuxin solution (Pan western pharmaceutcal co. Ltd,sichuan, China), the ulcers shrank and healed at day 54. Six rabbits in the 40W-MWA group experienced skin swelling. In one rabbit, swelling faded after 3 days and the other five developed ulcers with diameters between 1.5 and 3.7 cm. After disinfection and treatment with Kangfuxin solution, four developed infection and started to fast and lose weight. These four animals were euthanised with overdoses of anaesthetics according to the ethical norms of animal experimentation. In the DOX-MWA group, three rabbits experienced skin swelling. Two of these animals developed 0.3 cm and 0.5 cm ulcers, which healed at day 40 and 46, respectively, after disinfection and treatment with Kangfuxin solution ().
Table 2. Vice injury aroused by MWA.
Tumour regression
In the DOX group, tumour growth was not well controlled. In the 20W-MWA group no obvious changes were observed after the first 2 weeks of treatment. In the third week tumours softened and the long diameter average shrank to 2.63 ± 0.26 cm. In the DOX-MWA group the tumours softened after 2 weeks and the long diameters averaged 1.77 ± 0.21 cm in the third week. After the 3 weeks of treatment the long diameters between the DOX-MWA group and 20W-MWA group demonstrated statistically significant differences (t = 6.303, p < 0.01).
Discussion
At present the commonly used methods in breast cancer treatment and research have distinct advantages and quite a few disadvantages.
With a total effective rate of 60–90%, neoadjuvant chemotherapy (NCT) in clinical application is considered effective in down-staging breast cancer. Approximately 3–30% of patients experience complete pathological remission (pCR). A clinical study has shown that pCR patients have distinctly longer survival [Citation17]. pCR is generally accepted as a predictor of breast cancer survival. However, even after six to eight courses of NCT, only 10% to 25% of patients can achieve pCR with survival improvement. Tumour regression after NCT is not only concentric but also branch and nest-like [Citation18]. For patients with progressive breast cancer, NCT increases the chances of keeping their breasts. The presence of tumour residues does not significantly impact the survival team compared to patients who have chemotherapy after mastectomy. Furthermore, at least 5% of patients have progression during NCT. Thus, it has become a challenge for doctors to help patients receiving NCT to achieve pCR in a relatively shorter time.
Moreover, as a commonly used thermotherapy, MWA has its own advantages in both research trials and clinical application [Citation19–22]. In MWA, microwaves move the molecules bidirectionally to generate heat. This process is free from the influences of thermal subsidence, tissue carbonisation and tissue resistance. As a result there will be larger coagulation areas in a shorter time [Citation23–26]. MWA is relatively safe and effective in treating smaller breast tumours (< 3 cm) [Citation2]. However, for larger tumours or those within 1 cm of the skin and/or the thoracic wall, it is difficult to achieve optimal curative effects, either due to incomplete coagulation that causes a smaller ablation range, or injury to soft tissues caused by a larger range.
Several investigators have reported the use of pharmacological agents as adjuvants to RF ablation in an attempt to increase coagulation and improve clinical outcomes. Yang [Citation27] reported that paclitaxel can increase tumour coagulation and end-point survival in percutaneous RFA of tumours in a rat tumour model. Paclitaxel increased apoptosis and decreased Hsp70 expression at the coagulation margin. Ahmed et al. [Citation28] have described the co-administration of intravenous liposomal DOX with RF ablation in multiple tumour types, animal models, and a pilot clinical series. Benefits of this combination therapy over either RFA or liposomal DOX alone include increased intratumoural drug delivery predominantly in the peripheral ablation zone, where sublethal tissue heating occurs, and increased animal end-point survival [Citation29,Citation30]. Our study was intended to combine MWA and DOX to determine whether the combination could increase tumour coagulation and end-point survival in rabbit VX2 breast cancer.
Our study demonstrates that adjuvant DOX increases MWA-induced tumour coagulation more effectively than MWA or DOX alone, with gains similar to those observed in the combined RFA and liposomal DOX treatment [Citation31]. In the 20W-MWA (2450 MHz) group, the VX2 tumours of the modelled rabbits had an ablation area averaging 1.69 ± 0.34 cm2. In the DOX group one of the specimens had a necrotic range of 1.0 c× 0.6 cm, and the others had multiple spotty necrosis. In the DOX-MWA group the average ablation area was 4.52 ± 0.48 cm2 on average after administering DOX followed by 20W-MWA 24 h later. Our findings confirm that the necrosis range in the DOX-MWA group was clearly larger than the 20W-MWA group (p < 0.01) and DOX group, confirming that the combination of DOX and MWA can produce larger necrotic ranges and chemotherapy can intensify the effects of MWA. The result also proves that MWA can help with incomplete regression of tumours in NCT.
Significant differences in animal end-point survival were identified for MWA combined with DOX over MWA alone. The measurement of tumours after 3 weeks’ treatment showed that tumour growth in the control group and DOX group was not controllable. By contrast, decreases in tumour diameter were detected in both the 20W-MWA group and DOX-MWA group. Moreover, statistical analysis showed that tumour diameter in the DOX-MWA group was significantly smaller than in the 20W-MWA group (p < 0.01). Taking the end-point survival time into account, the prolonged survival time was relevant to the inhibition of tumour growth, which indicated that the combination of the two therapies could kill tumours more extensively than single therapy.
Cleaved caspase-3 acts as the most important final shear enzyme in cell apoptosis, or a significant part of the cytotoxic lymphocyte killing mechanism. Cleaved caspase-3, a significant marker, plays an irreplaceable role in cell apoptosis. The increase of cleaved caspase-3 expression indicates that cell apoptosis is ongoing [Citation6]. In this study, results of IHC and Western blotting analysis in coagulation margins showed that with the passage of time, the expression of cleaved caspase-3 in the DOX-MWA group was on the rise. In the 20W-MWA group, there was moderate expression of cleaved caspase-3, and the expression at 4 h and 24 h were almost the same. In the DOX group, weak positive expressions occurred at 4 h and 24 h. These results showed that in the DOX-MWA group continuously high expression of cleaved caspase-3 was one of the major causes of a larger ablation area in degenerative tissues.
HSP, a highly conserved protein, is synthesised by heat-induced living organisms. When under stress, HSP can boost cell resistance to offer protection. Hsp70, a heat shock protein, can offer protection against injury and its expression is up-regulated at the coagulation margins [Citation27]. In this study, Hsp70 in the DOX group expressed weak and positive. In the 20W-MWA group it had an increased expression in specimens taken at 4 h, which became more obvious in specimens taken at 24 h. Small amounts of Hsp70 deposition could be found in specimens at 4 h from the DOX-MWA group and no obvious increase was noticed in specimens at 24 h. As a stress-protective protein, Hsp70 demonstrated high expression in the 20W-MWA group, protecting the tissues from stress and mitigating the effects of heat shock. In tissues of the coagulation margin from the DOX-MWA group, Hsp70 was lowly expressed all along, indicating that the expression of Hsp70 was inhibited and could not offer protection. Therefore, the larger coagulation areas were correlated to the low expression of Hsp70 in the DOX-MWA group.
Based on the analysis of the two proteins, larger coagulation areas in the DOX-MWA group were positively correlated to cleaved caspase-3 expression. The low expression of Hsp70 deprived the tissues of stress protection. Compared with the 20W-MWA group, the distinctive increase in coagulation areas in this group could be attributed to the cumulative effects of both chemotherapy and thermal ablation. Rai and Richardson’s study revealed that the combination of RFA and heat shock protein medication, such as quercetin, could increase the tumour coagulation range and prolong animal survival time, which demonstrates that heat shock proteins can inhibit cell apoptosis.
Scalds occurred in two rabbits in the 20W-MWA group and three in the DOX-MWA group which, after conservative treatment, subsided and healed with no severe consequences. Compared with the 20W-MWA group, there were obviously larger coagulation ranges in the 40W-MWA group and more severe scalds in surrounding tissues. With the same microwave power and time, the DOX-MWA group had an obviously larger coagulation area with no more serious scalds than the 20W-MWA group. Therefore, it is concluded that compared with higher microwave intensity, weaker MWA combined with chemotherapy medication can result in a larger necrotic range and can avoid injury to the surrounding tissues to a largest extent. Guo et al. [Citation31] demonstrated that subcutaneous perfusion with D5W was effective in protecting the skin against burns during RF ablation without compromising the effect of ablation. If this technology were applied, the larger power could generate a larger area. Hyperthermia combined with radiotherapy and chemotherapy would ensure a complete ablation with fewer side effects.
Results of this study revealed that the combination of DOX and MWA could significantly increase the tumour necrotic range and prolong animal survival time, which to a certain extent verified the synergistic effects of DOX and MWA combination.
At present, the clinical treatment of breast cancer has entered a stagnant period. Problems, such as how to avoid treatment failure caused by incomplete tumour regression to achieve complete pathological remission, and how to reduce side injury and incomplete coagulation in tumour margins after thermotherapy to decrease the incidence of relapse, have to be settled urgently in both experimental and clinical treatment of breast cancer. The heterogeneity in breast cancer and the high degree of diversity among cancer-bearing patients make it difficult to research, develop and choose medications, requiring deeper research in breast cancer. Early stage tumours can be treated by thermal therapy together with short-cycle chemotherapy. This combination is effective and can reduce injury to surrounding tissues caused by thermal therapy alone and tumour residues caused by chemotherapy alone. For patients with progressive breast cancer, MWA combined with full cycle chemotherapy will not only keep primary tumour lesions under control but also offer treatment for metastases and leave as little tumour residues as possible. For patients with advanced stage cancer, combination therapy will also reduce tumour loading and delay tumour progress. If combined with other therapies such as endocrine or targeted therapies, better effects will be achieved. Further study should be focused on how to maximise the advantages of MWA to achieve even better results in breast cancer treatment.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Torre LA, Bray F, Siegel RL, Ferlay J. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87–108
- Zhou WB, Zha XM, Liu XA, Ding Q, Chen L, Ni Y. US-guided percutaneous microwave coagulation of small breast cancers: A clinical study. Radiology 2012;263:364–73
- Shimizu C, Ando M, Kouno T, Katsumata N, Fujiwara Y. Current trends and controversies over pre-operative chemotherapy for women with operable breast cancer. Jpn J Clin Oncol 2007;37:1–8
- Kim HR, Cheon SH, Lee KH, Ahn JR, Jeung HC, Lee SS. Efficacy and feasibility of radiofrequency ablation for liver metastases from gastric adenocarcinoma. Int J Hyperthermia 2010;26:305–15
- Thaker AA, Razjouyan F, Woods DL, Haemmerich D, Sekhar K, Wood BJ. Combination therapy of radiofrequency ablation and bevacizumab monitored with power Doppler ultrasound in a murine model of hepatocellular carcinoma. Int J Hyperthermia 2012;28:766–75
- Ahmed M, Moussa M, Goldberg SN. Synergy in cancer treatment between liposomal chemotherapeutics and thermal ablation. Chem Phys Lipids 2012;165:424–37
- Zhou WB, Ding Q, Liu XA, Jiang Y, Chen L, Zhang Y. Percutaneous microwave coagulation for eradication of VX2 tumors subcutaneously in rabbits. World J Surg Oncol 2012;30: 90–7
- Baisi A, De Simone M, Raveglia F, Cioffi U. Thermal ablation in the treatment of lung cancer: Present and future. Eur J Cardiothorac Surg 2013;43:683–6
- Brace CL. Radiofrequency and microwave ablation of the liver, lung, kidney, and bone: What are the differences? Curr Probl Diagn Radiol 2009;38:135–43
- Wissniowski TT, Hansler J, Neureiter D, Frieser M, Schaber S, Esslinger B. Activation of tumor-specific T lymphocytes by radio-frequency ablation of the VX2 hepatoma in rabbits. Cancer Res 2003;63:6496–500
- Lai R, Long Y, Li Q, Zhang X, Rong T. Oxidative stress markers may not be early markers of doxorubicin-induced cardiotoxicity in rabbits. Exp Ther Med 2011;2:947–50
- Choi SS, Sicklick JK, Ma Q, Yang L, Huang J, Qi Y. Sustained activation of Rac1 in hepatic stellate cells promotes liver injury and fibrosis in mice. Hepatology 2006;44:1267–77
- Shu GZ, Hui XX, Le HG, Lin NL, Feng L. The safety and treatment response of combination therapy of radioimmunotherapy and radiofrequency ablation for solid tumor: A study in vivo. PLoS One 2014;9:e96539
- Goldlberg SN, Kruskal JB, Oliver BS, Clouse ME, Gazelle GS. Percutaneous tumor ablation: Increased coagulation by combining radio-frequency ablation and ethanol instillation in a rat breast tumor model. Radiology 2000;217:823–9
- Goldberg SN, Gazelle GS, Compton CC, Mueller PR, Tanabe KK. Treatment of intrahepatic malignancy with radiofrequency ablation: Radiologic-pathologic correlation. Cancer 2000;88:2452–63
- Bear HD, Anderson S, Smith RE, Geyer CE, Mamounas EP, Fisher BR. Sequential preoperative or postoperative docetaxel added to preoperative doxorubicin plus cyclophosphamide for operable breast cancer: National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol 2006;24:2019–27
- Zhou W, Ding Q, Liu X, Jiang Y, Chen L, Zhang Y. Percutaneous microwave coagulation for eradication of VX2 tumors subcutane- ously in rabbits World J Surg Oncol 2012;10:97. doi: 10.1186/1477-7819-10-97
- Sun B, Song ST, Jiang ZF, Wang T, Zhang SH, Meng XY. Analysis of the factors affecting pathologic complete response to neoadjuvant chemotherapy in breast cancer patients. Chin J Oncol 2013;35:38–42
- Kanaoka Y, Yoshida C, Fukuda T, Kajitani K, Ishiko O. Transcervical microwave myolysis for uterine myomas assisted by transvaginal ultrasonic guidance. J Obstet Gynaecol Res 2009;35:145–51
- Simon CJ, Dupuy DE, Mayo-Smith WW. Microwave ablation: principles and applications. Radiographics 2005;25:S69–S83
- Yu J, Liang P, Yu X, Liu F, Chen L, Wang Y. A comparison of microwave ablation and bipolar radiofrequency ablation both with an internally cooled probe: Results in ex vivo and in vivo porcine livers. Eur J Radiol 2011;79:124–30
- Zhou WB, Jiang YN, Chen L, Ling L, Liang MD, Pan H. Image and pathological changes after microwave ablation of breast cancer: A pilot study. Eur J Radiol 2014;83:1771–7
- Kastler A, Alnassan H, Pereira PL, Alemann G, Barbé DA, Aubry S. Analgesic effects of microwave ablation of bone and soft tissue tumors under local anesthesia. Pain Med 2013;14:1873–81
- Brace CL, Hinshaw JL, Laeseke PF, Sampson LA, Lee FT. Pulmonary thermal ablation: Comparison of radiofrequency and microwave devices by using gross pathologic and CT findings in a swine model. Radiology 2009;251:705–11
- Zhang XG, Zhang ZL, Hu SY, Wang YL. Ultrasound-guided ablative therapy for hepatic malignancies: A comparison of the therapeutic effects of microwave and radiofrequency ablation. Acta Chir Belg 2014;114:40–5
- Yang W, Ahmed M, Elian M, Hady el- SA, Levchenko TS, Sawant RR. Do liposomal apoptotic enhancers increase tumor coagulation and end-point survival in percutaneous radiofrequency ablation of tumors in a rat tumor model? Radiology 2010;257:685–96
- Ahmed M, Liu Z, Lukyanov AN, Signoretti S, Horkan C, Monsky WL. Combination radiofrequency ablation with intratumoral liposomal doxorubicin: Effect on drug accumulation and coagulation in multiple tissues and tumor types in animals. Radiology 2005;235:469–77
- D’Ippolito G, Ahmed M, Girnun GD, Stuart KE, Kruskal JB, Halpern EF, Goldberg SN. Percutaneous tumor ablation: Reduced tumor growth with combined radio-frequency ablation and liposomal doxorubicin in a rat breast tumor model. Radiology 2003;228:112–18
- Ahmed M, Monsky WE, Girnun G, Lukyanov A, D'Ippolito G, Kruskal JB. Radiofrequency thermal ablation sharply increases intratumoral liposomal doxorubicin accumulation and tumor coagulation. Cancer Res 2003;63:6327–33
- Goldberg SN, Kamel IR, Kruskal JB, Reynolds K, Monsky WL, Stuart KE. Radiofrequency ablation of hepatic tumors: Increased tumor destruction with adjuvant liposomal doxorubicin therapy. Am J Roentgenol 2002;179:93–101
- Guo H, Liu XL, Wang YL, Li JY, Lu WZ, Xian JZ. Protection of skin with subcutaneous administration of 5% dextrose in water during superficial radiofrequency ablation in a rabbit model. Int J Hyperthermia 2014;30:258–65
