Abstract
Purpose The aim of this study was to evaluate the decrease of benign thyroid nodules after bipolar radiofrequency ablation (RFA) in a 3-month follow-up using a multiple overlapping shot technique (‘MOST’).
Methods A total of 18 patients with 20 symptomatic benign thyroid nodules (17 cold nodules, 3 hyperfunctioning nodules) were treated in one single session by bipolar RFA. Bipolar ablation was performed using MOST. The nodule volumes were measured prior to ablation and 3 months after the procedure using ultrasound. The population consisted of either solid (>80% solid tissue within the volume of interest), complex, or cystic nodules (<20% solid tissue within the volume of interest).
Results Bipolar RFA resulted in a highly significant (p < 0.0001) decrease of nodule volume (ΔV), median 5.3 mL (range 0.13–43.1 mL), corresponding to a relative reduction in mean of 56 ± 17.9%. Median initial volume was 8 mL (range 0.48–62 mL); 3 months after ablation a median volume of 2.3 mL (range 0.3–32 mL) was measured. Nodule growth ≥50% occurred in 70% (14 nodules). At the follow-up no complications such as infections, persisting pain, nerve injuries or immunogen stimulation occurred. Patients with cold nodules (15) remained euthyroid, with hyperfunctioning nodules either euthyroid (2) or latent hypofunctional (1).
Conclusion The use of bipolar RFA is an effective, safe and suitable thermoablative technique to treat benign thyroid nodules. Combined with the multiple overlapping shot technique it allows sufficient ablation.
Introduction
Different techniques of thermal ablation will be increasingly recognised as feasible treatments of benign thyroid nodules. While thermal ablation is already successfully used and established in organ tissues such as kidney [Citation1] and liver [Citation2,Citation3], the ablation of benign thyroid nodules is rather innovative and only performed in a small percentage of patients. Next to slightly novel systems such as microwave ablation (MWA) [Citation4–6] and high intensity focused ultrasound (HIFU) [Citation7–9] or more approved techniques such as laser ablation [Citation10], radiofrequency ablation (RFA) is the most investigated and commonly used technique of thermal ablation. For RFA, mainly monopolar systems are available, leading to several disadvantages caused by the required additional grounding pads. In monopolar systems the electrical current flows through the body and may therefore induce skin burns as well as interfering with electrical implantations such as pacemakers [Citation11,Citation12]. Bipolar systems are able to avoid these complications by integrating the anode and cathode within the same probe [Citation13]. Current studies performed in human thyroid diseases deal with monopolar systems [Citation14,Citation15], whereas bipolar systems are promising alternatives [Citation16].
Despite a first initial study declaring bipolar RFA as a safe treatment of symptomatic benign thyroid nodules, literature research is still missing data about nodule decline [Citation17].
The aim of this study was to evaluate the volume of benign thyroid nodules treated by bipolar RFA in a 3-month follow-up.
Material and methods
The study was retrospective. Written informed consents were obtained from all patients prior to the procedure and the study protocol was approved by the local ethics committee.
This study consisted of 18 patients (4 male, 14 female; mean age 50 years, age range 15–72) with 20 nodules, who were treated between November 2014 and July 2015. Patients included in this study did not receive any further thyroid treatment during the 3 months observation period to avoid falsifying influences. Nodule composition was divided into cystic (2), complex (10) or solid (8). The amount of solid tissue within the volume of interest was set at less than 20% in cystic nodules, and more than 80% in solid nodules.
Treatment condition
Inclusion criteria (≥1)
Mainly non-symptomatic thyroid nodules only causing cosmetic problems.
Symptomatic patients complaining about difficulty in swallowing, hoarseness, breathlessness or pain.
Proven non-malignancy.
Refusal of surgery.
Hyperfunctioning nodules and refusal of radioiodine therapy.
Exclusion criteria
Excessive thyroid volume with retrosternal growth including contiguous position to vessels, oesophagus, trachea or nerves.
Histological or scintigraphic sign of follicular dysplastic proliferation.
Absence of symptoms.
Procedure
In order to reduce local pain during the skin incision (2 mm) and electrode insertion, the patient received an analgesic medication. A short infusion of 0.9% NaCl with 2 mg metamizole (Novaminsulfon, Ratiopharm, Ulm, Germany) was attached prior to the procedure, followed by ultrasound-guided subcutaneous injection of local anaesthesia (mepivacaine hydrochloride 1% (AstraZeneca, Wedel, Germany). In order to optimally visualise the electrode along its entire active length and to maximize the safety margin for vulnerable structures such as jugular vein, carotid arteries, vagus nerve and recurrent laryngeal nerve, a transisthmic approach was chosen. If a transisthmic approach was not possible, a cranio-caudal approach was selected. The entire procedure was monitored by the use of ultrasound to identify upcoming hyperechogenic ‘microbubbles’ as an indicator of vaporisation during ablation as well as a subsequent oedema shown by echogenic decrease. Treatment was performed by using a so-called multiple overlapping shot technique (‘MOST’). Once one section of the nodule had been treated, the probe was repositioned next to the prior ablation area creating overlapping ablation zones (), which was repeated until the whole nodule was treated or the safety margin was reached. Afterwards, the transmitted energy was documented. All patients underwent an additional ultrasound examination within 24 h after RFA to address possible side effects and to verify a completed treatment. In order to quantify reduction of the nodule, all patients were scheduled for a further ultrasound diagnostic after 3 months.
Ablation procedure
The probe was chosen according to its active tip length, where the active tip length should not exceed the largest diameter of the imaged region of interest. The active tip was completely placed within the region of interest. Afterwards, the ablation was started with 10 W and gradually adjusted in 5–10 W steps. The duration was stopped according to patient tolerance, the local impedance measurement, and the forming ultrasound (US) changes, which should not exceed a predefined safety margin. Once one section was completely treated or the ablation was stopped, the probe was repositioned next to the prior ablation area. This procedure was repeated, until the whole nodule was treated.
Functional state
The laboratory parameters such as basal thyroid-stimulating hormone TSH, T3 and T4 were re-evaluated at the 3 months follow-up.
Equipment and calculation
Radiofrequency system
For bipolar RFA a generator (POWER System, Olympus, Hamburg, Germany), working in a frequency range of 470 ± 10 kHz leading to a maximum power output of 250 W, was used. The transmitted energy could be automatically adjusted based on a local impedance feedback and was applied by either internally cooled 15-gauge electrodes with an active tip length of 20–40 mm or by uncooled 18-gauge probes with an active tip length of 9–15 mm (CelonProSurge, Olympus, Hamburg, Germany). The internal cooling system was implemented within the electrode and reached fluid rates up to 30 mL/min.
Ultrasound system
Preablative assessment and follow-up evaluation were performed using an ultrasound based system (SonixTOUCH, Ultrasonix Medical, Richmond, BC, Canada).
Formula
The volume before and 3 months after treatment was calculated using the following equation for ellipsoid bodies:
where V is the volume, a is the largest diameter, and b andc are perpendicular diameters.
Statistical analysis
Statistical analysis was performed using the designated statistic software BiAS (Version 10.04; EPSiLON, 1989–2013). Initial volume, volume after 3 months, and volume reduction (ΔV) did not show normal distribution and were reported as median (range minimum–maximum). Relative volume reduction is given as mean ± standard deviation as it shows positive normal distribution. Wilcoxon matched-pairs test was performed to compare the initial volume to the volume after 3 months. Statistical level of significance was set at p < 0.05.
Results
Volume reduction
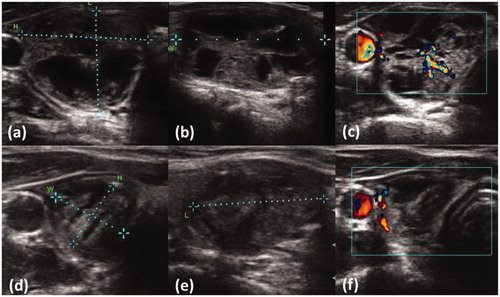
Bipolar ablation was performed in 18 patients with 20 nodules, where two patients had two nodules. None of the nodules was treated a second time within the follow-up duration. The ablation of thyroid nodules with bipolar RFA resulted in a significant (p < 0.0001) decrease of nodule volume after 3 months compared to the initial volume. While the median initial volume was 8 mL (range 0.48–62 mL), 3 months after ablation a median volume of 2.3 mL (range 0.3–32 mL) was measured (p < 0.001). The volume reduction ΔV (median 5.3 mL; range 0.13–43.1 mL) corresponds to a mean relative reduction of 56 ± 17.9% (). A nodule decrease ≥50% as a sign of satisfying treatment response occurred in 70% (14 nodules) (e.g. ). No nodule growth greater than the initial volume occurred after 3 months in any of the patients. On ultrasound guidance, the echogenicity of the nodules increased and appeared more solid. The reduction of central blood perfusion in the ablated area could still be visualized using Doppler sonography (e.g. ).
Table 1. Difference in volume 3 months after ablation.
Thyroid function and complications
Patients with hyperfunctioning nodules (3) occurred either as latent hypothyroid (1) or euthyroid (2) in laboratory blood tests at the follow-up. All patients with cold nodules (15) remained euthyroid after 3 months.
No severe complications such as nerve injuries, skin burns or damage of the vital surrounding tissue occurred. During re-examination no delayed complications such as infections, persistent pain, nerve injuries or immunogen stimulation were found. At the follow-up the symptoms of all patients had decreased.
Discussion
This study identifies bipolar RFA to be an effective treatment of benign thyroid nodules. Up to this point, few empirical data were available. Therefore, the data presented are the first clinical results dealing with the decline of thyroid nodules treated by bipolar RFA. Despite bipolar RFA being a novel system in human thyroid tissue, the decrease of nodule volume was close to the decrease reached by monopolar systems, which have already been used for years in thyroid tissue. With an average reduction of 56 ± 17.9% after 3 months (), the results are comparable to studies dealing with monopolar systems. While Jeong et al. reported a mean volume reduction of 74.4% after 3 months [Citation18], Baek et al. described a mean volume reduction of 67%±18% [Citation19]. In contrast to this study, in which patients underwent only one session within the follow-up, 30% of the patient population were treated multiple times with a maximum of six sessions [Citation18]. Nodules which were only treated twice are reported to show no statistical significance in nodule decline [Citation20], but if the treatment is extended by further ablations, an increasing influence on nodule decrease may not be excluded.
Next to cold nodules, the ablation of hyperfunctioning nodules (3) showed satisfying volume reduction (e.g. ) and had reached a euthyroid (2) or latent hypothyroid (1) functional state at the follow-up. These results are in accordance with comparable studies stating RFA as an effective treatment of hyperfunctioning thyroid nodules [Citation21,Citation22]. Most studies also include follow-ups after 6 months [Citation18,Citation19]. In this study a follow-up after 3 months was targeted. Basically, there is no consistent observation protocol after which time the nodules have to be evaluated again. The rates of reduction continuously decrease over a few months, but the greatest volume reduction is reported to be achieved during the first month [Citation18,Citation19,Citation23]. In some cases, progressing nodule reduction was still measurable after 4 years, and although further volume reduction after 3 months is probable, the major volume decrease had already occurred [Citation24]. Therefore, a follow-up after 3 months should show valid results. Additionally, the follow-up duration was aligned with the guideline of common procedures in benign human thyroid tissue such as radioiodine therapy, in which a follow-up after 3 months is targeted as well [Citation25]. To date, there are no official guidelines for bipolar ablation in thyroid tissue. For that reason different ablation protocols are used, where the moving shot technique is the most frequently practised. In contrast, the multiple overlapping shots technique (‘MOST’) was used instead of moving shots in this study. A recent study compared the fixed shot technique (FST), which is the technical basis of the MOST, with the more common moving shot technique [Citation26]. The authors assumed that the moving shot technique was superior against the FST because the probe was moved before local impedance could rise, which would have inhibited further electrical current. Consequently, more energy was transmitted and larger volumes could be ablated in less time [Citation26]. But the induced current in monopolar systems flows mainly between the grounding pads and the probe peak, thus a certain amount of energy is lost to the penetrated tissue. The effective heat induction is limited to a distinct area around the tip necessitating continuous movement during ablation [Citation15]. In contrast, bipolar systems mainly induce current flow between two separated electrodes within the probe, thus less electric current is lost to the surrounding tissue ( and Citation2) [Citation13]. Due to the electric field composition, the ablation zone of monopolar systems mainly grows along the probe axis, creating more elliptical lesions, while bipolar ablation zones grow perpendicularly around the probe as the electric field and induced heat are trapped between the inserted electrodes [Citation16]. Consequently, the ablation zone expands more spherically and allows large ablation volumes even if the probe is not moved, where probes between 20–30 mm especially are reported to exceed monopolar ablation size [Citation16]. While monopolar systems combined with moving shots may be able to hollow out the nodule more precisely, the use of MOST instead of the moving shot technique requires less technical skill, which can minimise performance loss due to the lack of physician treatment experience. The use of a simpler method is especially recommended where a new system such as bipolar RFA is used in highly vulnerable areas such as the neck and thyroid. These aspects may lead to the conclusion that MOST is the preferred technique in bipolar systems because a sufficient ablation is facilitated. Nevertheless, even though the use of MOST shows a significant and sufficient reduction of nodules, this method has been used less than the traditional moving shot technique so far, and therefore is not technically mature in its use yet. Organs such as the thyroid, which are adjacent to vulnerable structures such as nerves, vessels and parts of the respiratory tract, are at high risk of thermal damage [Citation27]. The temperature spread is not completely predictable, and potential damage is minimised by utilising either ‘heat sink’-effects through adjacent vessels [Citation28] such as the carotid artery, or choosing a transisthmic approach by creating a safety margin next to the so-called danger triangle, which contains the recurrent laryngeal nerve [Citation29]. Nonetheless, thermal damage to adjacent structures may not be excluded, thus a gentler and less aggressive treatment is reasonable. Thermal ablation with bipolar probes are reported to be well tolerated, where the most common symptom during ablation was moderate pain, stated at 3 out of 10 (Numeric Pain Rating Scale). The pain disappeared after the ablation stopped. After ablation, a small haematoma has been reported in 17% [Citation17]. During follow up the patients did not show delayed complications such as persisting pain, nerve injuries, infections or immunogen stimulation. The functional state remained euthyroid in patients with cold nodules (15), or became either latent hypothyroid (1) or euthyroid (2) in patients with hyperfunctioning nodules (3). These results emphasize bipolar ablation as safe and comfortable.
Figure 1. Expansion of the ablation zone by continuous movement (a). Effective heat induction within a distinct area around the active tip. A, carotid artery; V, jugular vein; N, vagus nerve.
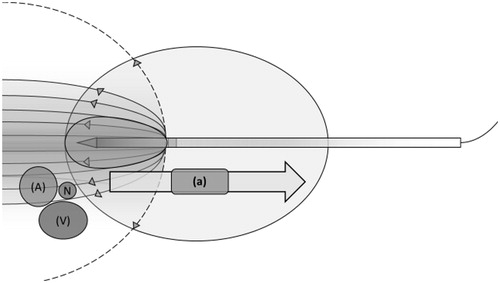
Figure 2. Multiple ablations (b) creating overlapping ablation zones (c). The ablation zone is more spherical as the heat rises more homogeneously between the two electrodes. A, carotid artery; V, jugular vein; N, vagus nerve.
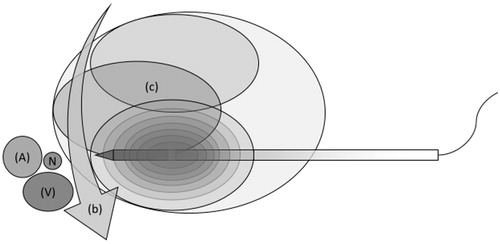
Figure 3: Patient with dextral nodule showing unifocal thyroid autonomy before RFA (a) and 3 months after (b). Ultrasound measurements revealed a relative reduction of 77.5%. (a) length = 19 mm; height = 24 mm; width = 36 mm; volume = 8.0 cm³. (b) length = 23 mm; height = 12 mm; width = 13 mm; volume = 1.8 cm³. After ablation the patient developed a euthyroid state of function. Sufficient ablation was verified by using Doppler blood flow before ablation (c) and 3 months after the procedure (d), showing a loss of central perfusing vessels as a sign of efficient treatment.
In contrast to bipolar RFA systems, neural pain is more probable in monopolar RFA, as the electrical current flows outside the thyroid, possibly stimulating adjacent nerves (). Monopolar systems require a higher power level, as more loss of energy has to be compensated, which possibly increases pain and the risk of complications. Consequently, the functional principle of bipolar systems seems recommendable, especially if the thyroid nodule is bordering vulnerable structures. The handling of bipolar RFA has to be taken into account as well. While monopolar probes require additional grounding pads, these are not necessary in bipolar ablation. The attachment of grounding pads is associated with further loss of time, because the skin has to be exposed and shaved before the pad is stuck. Also interference with implemented pacemakers as well as skin burns is more likely if monopolar probes are used as the current flows through the major part of the chest [Citation11,Citation12].
Summarised, bipolar systems reach sufficient, safe and promising nodule reduction. Nevertheless, this study should be supplemented through additional long-term follow-ups including larger patient populations to quantify clinical significance of bipolar RFA.
Limitations
There are a few limitations to this study, mainly the small number of patients. Despite initial results being shown after 3 months, complementary studies with longer follow-ups are imperative. Furthermore, different ablation protocols are used, which limits comparability to other studies. The respective influence is still uncertain and should be evaluated in further studies including both protocols.
Conclusion
Bipolar RFA represents an effective treatment of benign thyroid nodules. With an average volume reduction of 56 ± 17.9% at a 3-months follow-up, a significant decline of volume was reached. Bipolar RFA in combination with a multiple overlapping shot technique allows sufficient ablation. The favourable profile of side effects and handling are promising and should be taken into account.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Sung HH, Park BK, Kim CK, Choi HY, Lee HM. Comparison of percutaneous radiofrequency ablation and open partial nephrectomy for the treatment of size- and location-matched renal masses. Int J Hyperthermia 2012;28:227–34.
- Hocquelet A, Balageas P, Laurent C, Blanc J-F, Frulio N, Salut C, et al. Radiofrequency ablation versus surgical resection for hepatocellular carcinoma within the Milan criteria: A study of 281 Western patients. Int J Hyperthermia 2015;31:749–57.
- Zhang F, Wu G, Sun H, Ding J, Xia F, Li X, et al. Radiofrequency ablation of hepatocellular carcinoma in elderly patients fitting the Milan criteria: a single centre with 13 years experience. Int J Hyperthermia 2014;30:471–9.
- Korkusuz H, Happel C, Heck K, Ackermann H, Grünwald F. Percutaneous thermal microwave ablation of thyroid nodules. Nuklearmedizin 2014;53:123–30.
- Feng B, Liang P, Cheng Z, Yu X, Yu J, Han Z, et al. Ultrasound-guided percutaneous microwave ablation of benign thyroid nodules: Experimental and clinical studies. Eur J Endocrinol 2012;166:1031–7.
- Heck K, Happel C, Grünwald F, Korkusuz H. Percutaneous microwave ablation of thyroid nodules: Effects on thyroid function and antibodies. Int J Hyperthermia 2015;31:560–7.
- Korkusuz H, Sennert M, Fehre N, Happel C, Grünwald F. Local thyroid tissue ablation by high-intensity focused ultrasound: Effects on thyroid function and first human feasibility study with hot and cold thyroid nodules. Int J Hyperthermia 2014;30:480–5.
- Korkusuz H, Sennert M, Fehre N, Happel C, Grünwald F. Localized thyroid tissue ablation by high intensity focused ultrasound: Volume reduction, effects on thyroid function and immune response. RöFo 2015;187:1011–15.
- Korkusuz H, Fehre N, Sennert M, Happel C, Grünwald F. Volume reduction of benign thyroid nodules 3 months after a single treatment with high-intensity focused ultrasound (HIFU). J Ther Ultrasound 2015;3:4.
- Pacella CM, Mauri G, Achille G, Barbaro D, Bizzarri G, De Feo P, et al. Outcomes and risk factors for complications of laser ablation for thyroid nodules: A multicenter study on 1531 patients. J Clin Endocrinol Metab 2015;100:3903–10.
- Huffman SD, Huffman NP, Lewandowski RJ, Brown DB. Radiofrequency ablation complicated by skin burn. Semin. Intervent. Radiol. 2011;28:179–82.
- Tong NY, Ru HJ, Ling HY, Cheung YC, Meng LW, Chung PCH. Extracardiac radiofrequency ablation interferes with pacemaker function but does not damage the device. Anesthesiology 2004;100:1041.
- Ahmed M, Brace CL, Lee FT, Goldberg SN. Principles of and advances in percutaneous ablation. Radiology 2011;258:351–69.
- Bernardi S, Dobrinja C, Fabris B, Bazzocchi G, Sabato N, Ulcigrai V, et al. Radiofrequency ablation compared to surgery for the treatment of benign thyroid nodules. Int J Endocrinol 2014;2014:934595.
- Lee MT, Wang CY. Radiofrequency ablation in nodular thyroid diseases. J Med Ultrasound 2013;21:62–70.
- Bruners P, Lipka J, Günther RW, Schmitz-Rode T, Mahnken AH. Bipolar radiofrequency ablation: is the shape of the coagulation volume different in comparison to monopolar RF-ablation using variable active tip lengths? Minim Invasive Ther Allied Technol 2008;17:267–74.
- Korkusuz Y, Erbelding C, Kohlhase K, Luboldt W, Happel C, Grünwald F. Bipolar radiofrequency ablation of benign symptomatic thyroid nodules: Initial experience with bipolar radiofrequency. Rofo 2015. PMID 26713416. DOI: 10.1055/s-0041-110137.
- Jeong WK, Baek JH, Rhim H, Kim YS, Kwak MS, Jeong HJ, et al. Radiofrequency ablation of benign thyroid nodules: Safety and imaging follow-up in 236 patients. Eur Radiol 2008;18:1244–50.
- Baek JH, Kim YS, Lee D, Huh JY, Lee JH. Benign predominantly solid thyroid nodules: Prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. Am J Roentgenol 2010;194:1137–42.
- Huh JY, Baek JH, Choi H, Kim JK, Lee JH. symptomatic benign thyroid nodules: efficacy of additional radiofrequency ablation treatment session – prospective randomized study. Radiology 2012;263:909–16.
- Sung JY, Baek JH, Jung SL, Kim J, Kim KS, Lee D, et al. Radiofrequency ablation for autonomously functioning thyroid nodules: A multicenter study. Thyroid 2015;25:112–17.
- Baek JH, Moon W-J, Kim YS, Lee JH, Lee D. Radiofrequency ablation for the treatment of autonomously functioning thyroid nodules. World J Surg 2009;33:1971–7.
- Shin JH, Baek JH, Ha EJ, Lee JH. Radiofrequency ablation of thyroid nodules: Basic principles and clinical application. Int J Endocrinol 2012;2012:7. Article ID 919650.
- Lim HK, Lee JH, Ha EJ, Sung JY, Kim JK, Baek JH. Radiofrequency ablation of benign non-functioning thyroid nodules: 4-year follow-up results for 111 patients. Eur Radiol 2013;23:1044–9.
- Nuklearmedizin.de. Deutsche Gesellschaft für Nuklearmedizin e.V. 2016 Available from: http://www.nuklearmedizin.de/leistungen/leitlinien/html/rit_ben_schild_v4.php (accessed 21 January 2016).
- Ha EJ, Baek JH, Lee JH. Moving-shot versus fixed electrode techniques for radiofrequency ablation: Comparison in an ex-vivo bovine liver tissue model. Korean J Radiol 2014;15:836–43.
- Ha EJ, Baek JH, Lee JH. Ultrasonography-based thyroidal and perithyroidal anatomy and its clinical significance. Korean J Radiol 2015;16:749–66.
- Zorbas G, Samaras T. A study of the sink effect by blood vessels in radiofrequency ablation. Comput Biol Med 2015;57:182–6.
- Baek JH, Lee JH, Valcavi R, Pacella CM, Rhim H, Na DG. Thermal ablation for benign thyroid nodules: Radiofrequency and laser. Korean J Radiol 2011;12:525–40.
