Abstract
Objectives: The aim of this study was to characterize the current practice of asthma among general practitioners (GPs) in Lebanon. Methods: Out of 2450 Lebanese registered GPs, a representative sample of 330 were stratified by region to fill out the questionnaire constructed on the basis of surveys developed mainly by the Chicago Asthma Surveillance Initiative Report Team in newly moderate persistent asthma patients aged 5 years and above. The questionnaire included information about ascertaining diagnostic techniques, pharmacotherapeutic approaches, formal patient education program; asthma related continuing medical education and asthma practice guidelines. Results: Totally, 302 completed the questionnaire achieving a response rate of 91.5%. Chest radiography was the most commonly used diagnostic test (98%), while stain for eosinophilia was the less commonly used (7.9%). For clinical monitoring, cough and wheezing (98.7%) were mostly assessed. Short acting inhaled β2-agonists were often the most prescribed (94.3%) followed by inhaled corticosteroids (87.4%) then by long acting β-agonist (LABA) and theophylline (27.5% and 20.9%, respectively). Moreover, 10% of GPs provided formal asthma education program, 72.2% attended professional education and 65% adopted guidelines. Conclusion: Based on current international guidelines, the overall Lebanese GPs practice of asthma management is not at an acceptable standard. Therefore, it is recommended to improve monitoring parameters, implement the asthma guidelines nationally and improve patient education.
Introduction
Asthma is one of the most common chronic illnesses worldwide [Citation1]. As of 2011, the World Health Organization (WHO) estimated that globally, around 235 million people suffer from asthma [Citation1]. Many strategies have been employed to decrease asthma related mortality and morbidity [Citation2–5]. The National Asthma Education and Prevention Program (NAEPP), which was founded by the National Heart, Lung, and Blood Institute (NHLBI), has established guidelines for the proper diagnosis and treatment of asthma [Citation6]. Despite these guidelines, increases in the prevalence, morbidity, mortality and economic burden of asthma have been reported throughout the world [Citation7–9]. This impacts the physical, emotional and social well-being of sufferers [Citation1,Citation10].
Asthma needs to be recognized as a health priority in the developing world. Increasing urbanization further increases asthma incidence rates with consequent rises in asthma-related morbidity and mortality [Citation11].
Successful management of asthma requires that the physician be cognizant of the national recommendations, including pharmacotherapy and measures to prevent and control exacerbations [Citation12].
Significant differences in the management of asthma are also apparent between specialists and general practitioners (GPs) [Citation13]. GPs play a key role in both identifying poorly controlled asthma and improving disease management outcomes since many asthmatic patients in rural communities are initially seen by them [Citation5,Citation14]. In a recent European study, GPs were experts at excluding those who did not have asthma (specificity 99%), but poorly diagnosed those who had current asthma (sensitivity 59%) [Citation15].
There is a little published information in developing countries describing primary-care physicians’ willingness to embrace the guidelines and assess their practice in managing asthma [Citation16,Citation17].
Compositional differences in educational experience among Lebanese GPs may contribute to heterogeneity in treatment strategies [Citation18]. The physician's practice in managing asthma must be region-specific to ensure that they are tailored to the needs of a given region [Citation19]. Thus, the aim of this cross-sectional study is to evaluate the current practice of Lebanese GPs in managing asthma.
Materials and methods
Ethical approval
Approval from the Institutional Review Board at Makassed General Hospital, Beirut, Lebanon was sought prior to commencement of this cross-sectional survey.
Data sources
Primary data sources utilized in this study were the Lebanese Order of Physicians and the Order of Physicians in North Lebanon. Physicians are unequally distributed between the two professional associations that supervise their practice. One caters for the physicians of North Lebanon, while the four regions are under the Lebanese Order of Physicians. The database of the two orders contained contact information, in addition to the demographic and educational characteristics.
Indeed, to be able to practice in Lebanon, physicians have to be registered with one of these two orders, after passing the same licensure test. There are mechanisms in place to avoid dual registration and to remove physician who no longer practice from the databases. Physicians who are not Lebanese citizens cannot register and therefore cannot practice in Lebanon.
The national census has not been conducted since 1932; this makes recent demographic analysis of Lebanese society a difficult task. Currently, the ratio of physicians to population in Lebanon ranks among the highest in the Eastern Mediterranean region (248 physicians per 100 000 population) [Citation20]. This ratio is characterized by an uneven geographic distribution where the bulk resides in Beirut [Citation20].
Out of 7726 physicians (which included general medicine, internal medicine, pediatrics and obstetrics and gynecology), 2450 were exclusively categorized as GPs. Sampling proportionate to population size of GPs for each district was randomly drawn (
Table 1. Distribution of GPs among regions in Lebanon.a
The questionnaire was constructed on the basis of surveys developed by the NHLBI [Citation14], and the Chicago Asthma Surveillance Initiative Report Team [Citation21,Citation22] to assess the current practice among Lebanese GPs in managing asthma.
Diagnosis of asthma basically depends on clinical assessment (frequency of cough, wheezing, β2-agonist use, sleep disturbance and activity level) in addition to laboratory, radiological investigations and pulmonary function testing.
The questionnaire included information ascertaining asthma diagnostic techniques (chest radiography, spirometry, skin testing or radioallergosorbent testing (RAST), daily peak expiratory flow (PEF) monitoring, sinus radiography and sputum exam for eosinophil) used for new asthma patients aged 5 years and above, the clinical monitoring by physicians during regular office visits and the availability or access to spirometry, pharmacotherapeutic approaches to treat asthma, availability of formal patient education program in their clinics, involvement in continuing medical education activities related to asthma, use of asthma practice guideline and demographic characteristics (age, gender, country of medical degree and specialty, year of medical degree graduation and number of asthma patients seen per week).
The validity of the questionnaire was ensured through a pilot sample of 15 GPs who stated that the clarity of the questionnaire was satisfactory with no ambiguity.
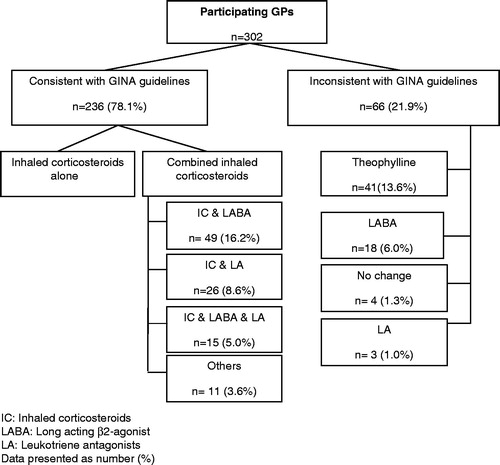
Evaluation of asthma treatment was made through two questions: the first was about the medication/s to be used for patients aged 5 years and above with moderate persistent asthma. The second question was in a form of hypothetical clinical scenario: “what are the other medications needed for a patient aged 5 years and above with an uncontrolled asthma maintained on short acting β2-agonists inhaler?”. Options that included inhaled steroids as mono-therapy or combination were considered as consistent with Global Initiative for Asthma (GINA) guidelines, otherwise were considered inconsistent [Citation5].
Statistical analyses
Region (Beirut, Bekaa, Mount Lebanon, North, South)-stratified random sampling was drawn to ensure that the sample was nationally representative. Data analysis was conducted using SAS software (SAS Institute; Cary, NC) to calculate frequency distributions. Means were reported with their corresponding standard deviations (SDs) and frequencies with percentages.
Results
A total of 330 questionnaires were distributed among GPs, of whom 302 completed the questionnaire achieving a response rate of 91.5%.
The characteristics of 302 Lebanese GPs are presented in
Table 2. Sociodemographic characteristics of GPs participating in the study (n = 302).a
Evaluation and clinical monitoring of asthma patients
For the initial evaluation, chest radiography was the most commonly used diagnostic test by 296 (98.0%) GPs, while sputum exam for eosinophils was the less commonly used diagnostic test (7.9%). Spirometry performed by 142 (47.0%) GPs 3 (0.7%) were performed on site, 139 (46.3%) were performed in specialized centers). In addition, only one GP (0.3%) referred a patient to a specialist for spirometry. In addition, daily peak flow was performed by 63 (20.9%) GPs and 68 (22.5%) GPs referred their patients to allergologist for skin testing or RAST (
Table 3. Asthma diagnostic techniques and clinical monitoring used by participating GPs for asthmatic patients.a
For clinical monitoring, the presence of cough and wheezing (98.7%) were mostly assessed. Whereas, PEF diary review (3.0%) was rarely monitored ().
Asthma treatment
Asthma pharmacotherapy approaches are presented in
Table 4. Pharmacotherapeutic approaches reported by participating GPs for patients ≥5 years old with moderate persistent symptoms.a
presented the pharmacotherapeutic approaches reported by GPs where short acting inhaled β2-agonists were often the most prescribed (94.3%) followed by inhaled corticosteroids (87.4%) then by long acting β-agonist (LABA) and theophylline (27.5% and 20.9%, respectively).
Treatment approach comparison of uncontrolled asthmatics on inhaled short acting β2-agonists treatment with GINA recommendations are presented in
. Of all, 78.1% prescribed inhaled corticosteroids, of which 44.7% were prescribed alone and the remaining 33.4% were prescribed in combination with one of the followings: LABA, LA, LABA & LA and others.Patient education and continuous medical education
Almost 90% of GPs did not provide a formal asthma education program for their patients.
Awareness of the GINA Guidelines was high, with 85% of GPs reporting that they have heard of the guidelines and 72.5% reporting of having read them. Moreover, 65% of GPs reported GINA Guidelines as the most adopted guidelines.
Most of the GPs (72.2%) attended a variety of professional education related to the management of asthma.
Discussion
To understand the current asthma management practice in Lebanon, a nationwide sample of GPs were surveyed to determine their actual asthma practices.
Lebanese GPs practice was consistent with international guidelines for patients ≥5 years old with moderate persistent asthma as inhaled short acting β2-agonist was often prescribed (94.4%). However, for uncontrolled asthmatics aged 5 years and above on inhaled short acting β2-agonist, our GPs showed lower compatibility with GINA Guidelines as 78.1% prescribed inhaled corticosteroids compared to (95.7%) in Chicago asthma surveillance [Citation21]. Corticosteroids remains the most potent primary controller medication for asthma [Citation22]. Those who were not well controlled on inhaled steroids (33.4%), the addition of LABA or leukotriene antagonists might improve their asthma control [Citation23–25]. GPs who are inconsistent with GINA Guidelines, still prescribe theophylline (13.6%) over LABA (6%) or leukotriene receptor antagonists (1%). This could be due to the lack of awareness on asthma treatment, or more likely, because theophylline preparations were cheaper than inhalers.
The compliance of GPs with the guidelines showed variability between Asian and European countries [Citation16,Citation26–28]. In Karachi, Pakistan, a cross-sectional survey conducted by Bhulani et al. found inadequate knowledge of asthma medications among GPs in comparison with the GINA Guidelines and only 10.4% of GPs had adequate practice in asthma management [Citation16]. Similarly, a study by Hussain et al. demonstrated serious deficiencies in the knowledge and attitude of GPs in the management of asthma patients in Pakistan [Citation26]. Moreover, in Genoa, Italy Kryj-Radziszewska et al. found that only 20% of the GPs were able to answer correctly the questions regarding asthma control [Citation27]. However, in Poland, a study by Braido showed a higher GPs compatibility with the guidelines; 42% in the part “General principles of treatment” and 65% in “Pharmacotherapy” [Citation28]. The polish figures are more comparable to our findings.
The present survey showed that PEF monitoring was not commonly used by GPs. This is recommended by GINA Guidelines. Possible limited availability or access to PEF meters may be a factor [Citation29]. When this data was compared to data from Grant et al. [Citation21], the utilization of PEF was much less among our GPs (20.9% versus 47.5%).
Our ratios of ordering spirometry (47%) and RAST (22%) were comparable to Chicago asthma surveillance (54.6% and 14.1%, respectively) [Citation21]. Similarly, the sputum examination and stain for eosinophilia rates were comparable between Lebanon and Chicago (7.9% versus 5%, respectively). The RAST has a sensitivity of 70–75% for the detection of allergen-specific IgE [Citation30]. Increase in sputum eosinophils as a predictor of airway inflammation is often seen in patients with asthma [Citation31]. In some cases, patients with uncontrolled asthma and airway hyper-responsiveness (PC20 <4 mg/ml) demonstrated an increase in sputum eosinophils to a median of 4.5% [Citation32], but this observation has not been consistently demonstrated [Citation33].
The perception of strict asthma control has evolved over the past years. While the goals set by GINA [Citation5] and NAEPP [Citation34] Guidelines seem unrealistic and unachievable for some clinicians, but meticulous monitoring, treatment and education can make it possible [Citation35]. We were able to identify important aspects of asthma monitoring in Lebanon that were divergent to the international guidelines. Activity levels and loss of work or school days due to asthma were not routinely asked by GPs (24.2% and 10.3%, respectively). GPs are not expected to comply with the use of spirometry as it is not included in their routine practice which was clearly reflected in our findings.
Patient education is an essential component of asthma care. Our survey showed that patients warrant better education about asthma as only 10% had previous asthma education program. This could be related to limited availability or awareness of this program.
Conclusion
Based on current international guidelines, the overall Lebanese GPs practice of asthma management is not at an acceptable standard. Therefore, it is recommended to improve monitoring parameters, implement the asthma guidelines nationally and improve patient education.
Declaration of interest
The authors declare no conflicts of interest. No funding was sought or received for this study.
Supplementary Material
Download PDF (197.5 KB)Acknowledgements
We acknowledge Ms. Linda Kennedy for her editing assistance.
References
- World Health Organization (WHO). Asthma fact sheet No. 207; 2011. Available from: http://www.who.int/chp/knowledge/publications/adherence [last accessed 2 Apr 2013]
- NHLBI/WHO Workshop Report: global strategy for asthma management and prevention; 2002. NIH. 02-3659
- Evans R, Mullally DI, Wilson RW, Gergen PJ, Rosenberg HM, Grauman JS, Chevarley FM, Feinleib M. National trends in the morbidity and mortality of asthma in the US. Prevalence, hospitalization and death from asthma over two decades. Chest 1987;91:65–74
- Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, Gibson P, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J 2008;31:143–178
- Global Initiative for Asthma. Global strategy for asthma management and prevention; 2013. Available from: http://www.gina.com [last accessed 13 Apr 2013]
- National Asthma Education and Prevention Program. Expert panel report 2: guidelines for the diagnosis and management of asthma. Bethesda, MD: US Dept of Health and Human Services; 1991, NIH: 97-4051
- Campbell JD. Managed care opportunities for improving asthma care. Am J Manag Care 2011;17:90–96
- Taylor DM, Auble TE, Calhoun WJ, Mosesso VN, Jr. Current outpatient management of asthma shows poor compliance with International Consensus Guidelines. Chest 1999;116:1638–1645
- Haby MM, Powell CV, Oberklaid F, Waters EB, Robertson CF. Asthma in children: gaps between current management and best practice. J Paediatr Child Health 2002;38:284–289
- The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Worldwide variations in the prevalence of asthma symptoms: the International Study of Asthma and Allergies in Childhood (ISAAC). Eur Respir J 1998;12:315–335
- Braman SS. The Global Burden of Asthma. Chest 2006;130:4S–12S
- Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma (EPR—2 1997). NIH Publication No. 97-4051. Bethesda, MD, U.S. Department of Health and Human Services; National Institutes of Health; National Heart, Lung, and Blood Institute; National Asthma Education and Prevention Program; 1997
- Laforest L, Van Ganse E, Devouassoux G, Chretin S, Osman L, Bauguil G, Pacheco Y, Chamba G. Management of asthma in patients supervised by primary care physicians or by specialists. Eur Respir J 2006;27:42–50
- Wolle JM, Cwi J. Physicians’ prevention-related practice behaviors in treating adult patients with asthma: results of a national survey. J Asthma 1995;32:131–140
- Montnémery P, Hansson L, Lanke J, Lindholm LH, Nyberg P, Löfdahl CG, Adelroth E. Accuracy of a first diagnosis of asthma in primary health care. Fam Pract 2002;19:365–368
- Bhulani N, Lalani S, Ahmed A, Jan Y, Faheem U, Khan A, Samani Z, et al. Knowledge of asthma management by general practitioners in Karachi, Pakistan: comparison with international guidelines. Prim Care Respir J 2011;20:448–451
- Salama AA, Mohammed AA, El Okda el SE, Said RM. Quality of care of Egyptian asthmatic children: clinicians adherence to asthma guidelines. Ital J Pediatr 2010;36:33
- Akl EA, El-Asmar K, Maroun N, Adib SM, Khater-Menassa B. Did the post war repatriation of Lebanese physicians drive recent Lebanese medical graduates to emigrate? An observational study. BMC Health Serv Res 2008;8:195
- National Institutes of Health. Making a difference in the management of asthma: a guide for respiratory therapists 2003, 02-1964. Available from: http://www.nhlbi.nih.gov/health/prof/lung/asthma/asth_respir.pdf [last accessed 5 May 2013]
- Kassak KM, Ghomrawi HM, Osseiran AM, Kobeissi H. The providers of health services in Lebanon: a survey of physicians. Hum Resour Health 2006;4:4
- Grant EN, Moy JN, Turner-Roan K, Daugherty SR, Weiss KB. Asthma care practices, perceptions, and beliefs of Chicago-area primary care physicians. Chest 1999;116:145S–154S
- Jason C, Gislason T, Boman G, Hetta J, Roos BE. Sleep disturbances in patients with asthma. Respir Med 1990;84:37–42
- Price DB, Hernandez D, Magyar P, Fiterman J, Beeh KM, James IG, Konstantopoulos S, et al. Clinical outcomes with montelukast as a partner agent to corticosteroid therapy (COMPACT) International Study Group. Randomized controlled trial of montelukast plus inhaled budesonide versus double dose inhaled budesonide in adult patients with asthma. Thorax 2003;58:211–216
- Vaquerizo MJ, Casan P, Castillo J, Perpiña M, Sanchis J, Sobradillo V, Valencia A, et al; CASIOPEA (Capacidad de Singulair Oral en la Prevencion de ExacerbacionesAsmaticas) Study Group. Effect of montelukast added to inhaled budesonide on control of mild to moderate asthma. Thorax 2003;58:204–210
- Virchow JC, Prasse A, Naya I, Summerton L, Harris A. Zafirlukast improves asthma control in patients receiving high-dose inhaled corticosteroids. Am J Respir Crit Care Med 2000;162:578–585
- Hussain SF, Zahid S, Khan JA, Haqqee R. Asthma management by general practitioners in Pakistan. Int J Tuberc Lung Dis 2004;8:414–417
- Kryj-Radziszewska E, Windak A, Margas G, Wizner B, Grodzicki T. The influence of guidelines of asthma management in adults in reference to family physician’s knowledge in the field of treatment. Przegl Leg 2008;6:166–171
- Braido F, Baiardini I, Stagi E, Piroddi MG, Balestracci S, Canonica GW. Unsatisfactory asthma control: astonishing evidence from general practitioners and respiratory medicine specialists. J Investig Allergol Clin Immunol 2010;20:9–12
- Khadadah M, Mahboub B, Al-Busaidi NH, Sliman N, Soriano JB, Bahous J. Asthma insights and reality in the Gulf and the near East. Int J Tuberc Lung Dis 2009;13:1015–1022
- Williams PB, Dolen WK, Koepke JW, Selner JC. Comparison of skin testing and three in vitro assays for specific IgE in the clinical evaluation of immediate hypersensitivity. Ann Allergy 1992;68:35–45
- Green RH, Brightling CE, NcKenna S, Hargadon B, Parker D, Bradding P, Wardlaw AJ, Pavord ID. Asthma exacerbations and sputum eosinophil counts: a randomized controlled trial. Lancet 2002;360:1715–1721
- Pizzichini E, Pizzichini MM, Efthimiadis A, Evans S, Morris MM, Squillace D, Gleich GJ, et al. Indices of airway inflammation in induced sputum: reproducibility and validity of cell and fluid-phase measurements. Am J Respir Crit Care Med 1996;154:308–317
- Lemière C, Walker C, O'Shaughnessy D, Efthimiadis A, Hargreave FE, Sears MR. Differential cell counts in sputum in respiratory epidemiology: a pilot study. Chest 2001;120:1107–1113
- National Asthma Education and Prevention Program. Expert Panel Report 2: Guidelines for the diagnosis and management of asthma. Bethesda, MD: US Dept of Health and Human Services, National Institute of Health; 1997. NIH publication 97-4051
- Bateman ED, Boushey HA, Bousquet J, Busse WW, Clark TJ, Pauwels RA, Pedersen SE; GOAL Investigators Group. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma Control study. Am J Respir Crit Care Med 2004;170:836–844
Appendix 1
Serial #: _______
Dear Dr.,
We are conducting a cross sectional study to evaluate the current practice of Lebanese GPs in managing asthma. You are kindly asked to take few minutes to answer the following questionnaire.
1) Age: _______years 2) Sex: □ Male □ Female
3) Year of medical school graduation: __________
4) Where did you study medicine (country)? __________________
5) How many patients with asthma do you see weekly?
□ 1–4 □ 5–10 □ >10
6) What diagnostic technique(s) do you do for newly diagnosed patients with asthma?
(Check all applicable items)
□ Chest radiography □ Spirometry □ Skin testing or RAST
□ Sinus radiographs □ Trail of daily peak flow monitoring
□ Sputum examination and stain for eosinophilia
7) What do you monitor during office visits?
□ Frequency of cough and wheezing
□ Frequency of β2-agonist use
□ Frequency of disturbed sleep due to asthma
□ Loss of work/school days due to asthma
□ Spirometry
□ Peak flow
□ Direct observation of inhaler technique
□ Peak flow diary review
□ Patient activity level
8) Do you have access to spirometry?
□ No
□ Yes, where: □ In my office □ Hospital □ Specialized center
9) Do you use inhalers for patients with asthma?
□ Often □ Sometimes □ Rarely □ Never
10) Do you prescribe spacer devices with the metered dose inhalers (MDIs)?
□ Often □ Sometimes □ Rarely □ Never
11) Are you certain about the safety of inhaled corticosteroids.
□ Yes □ No
12) What are the medications you prescribe for patients ≥5 years old with moderate persistent asthma?
12.1 Oral β-agonist □ Often □ Sometimes □ Rarely □ Never
12.2 Inhaled β-agonist □ Often □ Sometimes □ Rarely □ Never
12.3 Theophylline □ Often □ Sometimes □ Rarely □ Never
12.4 Long acting β-agonist (LABA) □ Often □ Sometimes □ Rarely □ Never
12.5 Inhaled steroids □ Often □ Sometimes □ Rarely □ Never
12.6 Oral steroids □ Often □ Sometimes □ Rarely □ Never
12.7 Leukotriene antagonist □ Often □ Sometimes □ Rarely □ Never
12.8 Cromolyn or nedocromil □ Often □ Sometimes □ Rarely □ Never
12.9 Oral anti-histamines □ Often □ Sometimes □ Rarely □ Never
13) For a patient (>5 years of age) with daily symptoms that respond to three times daily short acting β-agonists as his or her only medication who is waking up more than twice a month with asthma symptoms, what would you do next? (Choose one item only)
□ No change □ Increase β-agonists □ Add theophylline
□ Add oral steroids □ Add inhaled steroids □ Add cromolyn
□ Add long acting β-agonists
□ Add oral anti-histamine
□ Add Montelukast or Zafirlukast
□ Add inhaled steroids and Montelukast/Zafirlukast
□ Add inhaled steroids and long acting β-agonist
□ Add inhaled steroids and Montelukast/Zafirlukast and long acting β-agonist
□ Other: _________________________________________________________
14) Do you use “practice guidelines” for the treatment of asthma?
□ No
□ Yes:
If yes, please specify
□ Other: _____________________________________________________________________________________
15) Have you attended a lecture on asthma in the past year?
□ Yes □ No
16) Have you educated your patients about asthma?
□ Yes □ No
Thank you for your cooperation.