Abstract
Objective. To investigate the course of mental health problems in children presenting to general practice with abdominal pain and to evaluate the extent to which abdominal pain characteristics during follow-up predict the presence of mental health problems at 12 months’ follow-up. Design. A prospective cohort study with one-year follow-up. Setting. 53 general practices in the Netherlands, between May 2004 and March 2006. Subjects. 281 children aged 4–17 years. Main outcome measures. The presence of a depressive problem, an anxiety problem, and multiple non-specific somatic symptoms at follow-up and odds ratios of duration, frequency, and severity of abdominal pain with these mental health problems at follow-up. Results. A depressive problem persisted in 24/74 children (32.9%; 95% CI 22.3–44.9%), an anxiety problem in 13/43 (30.2%; 95% CI 17.2–46.1%) and the presence of multiple non-specific somatic symptoms in 75/170 children (44.1%; 95% CI 36.7–51.6%). None of the abdominal pain characteristics predicted a depressive or an anxiety problem at 12 months’ follow-up. More moments of moderate to severe abdominal pain predicted the presence of multiple non-specific somatic symptoms at follow-up. Conclusions. In one-third of the children presenting to general practice for abdominal pain, anxiety and depressive problems persist during one year of follow-up. Characteristics of the abdominal pain during the follow-up period do not predict anxiety or depressive problems after one-year follow-up. We recommend following over time children seen in primary care with abdominal pain.
Children with abdominal pain often have mental health problems; however, the prognosis of these problems is unknown. This follow-up study showed that:
in one-third of the children depressive and anxiety problems persist over one year;
characteristics of the abdominal pain during follow-up do not predict the presence of depressive and anxiety problems at 12 months’ follow-up;
in children with persisting moderate to severe abdominal pain other non-specific somatic symptoms also persist.
Introduction
Abdominal pain is one of the most common complaints in childhood [Citation1,Citation2]. Childhood abdominal pain often can be characterized by the following aspects: (i) usually no organic abnormalities can be found explaining the pain [Citation3,Citation4], (ii) the abdominal pain tends to have a prolonged or recurrent course [Citation2,Citation5], (iii) children with abdominal pain often have mental health problems [Citation6,Citation7] and (iv) the abdominal pain affects the child's daily life and well-being [Citation8]. In the literature a variety of expressions are used describing this pain syndrome in children: recurrent abdominal pain [Citation3], chronic abdominal pain [Citation9,Citation10], functional abdominal pain [Citation11], non-specific abdominal pain [Citation12].
As follow-up studies on children with abdominal pain are scarce, the prognosis for mental health problems in these children is basically unknown. In addition, the direction of the relationship between abdominal pain and mental health problems is largely unknown as well, as it has primarily been established in cross-sectional studies. Disentanglement of the relation between abdominal pain and mental health problems will allow for more effective management of both the abdominal pain and the mental health problems.
The present study investigates the course of mental health problems in a cohort of children presenting with abdominal pain in general practice. We further evaluated the extent to which abdominal pain characteristics during the follow-up period predict mental health problems at 12 months’ follow-up.
Material and methods
Participants
Between May 2004 and March 2006, 53 general practitioners (GP) in the Netherlands invited all consecutive patients aged 4–17 years presenting with a new episode of abdominal pain to participate in a one-year follow-up study (the HONEUR abdominal pain cohort). A new episode of abdominal pain was defined as a consultation for abdominal pain not preceded by a consultation for this complaint in the previous three months. In total 305 children were included. Detailed methods of the study have been described previously [Citation13].
Measurements
All data were collected with structured questionnaires and were filled in at baseline and after three, six, nine, and 12 months’ follow-up.
Characteristics of the abdominal pain
We investigated the following abdominal pain characteristics: presence of chronic abdominal pain (yes/no), duration of chronic abdominal pain (0–15 months), severity (0–10), and frequency (0–5) [Citation14] of abdominal pain. Chronic abdominal pain was defined as abdominal pain that occurred at least once each month in three consecutive months [Citation3].
Diagnoses of the abdominal pain by the GP
We searched the electronic medical records (EMR) at three months’ follow-up of all included children to record the diagnosis as coded according to the International Classification of Primary Care (ICPC) [Citation15] by the GP. We categorized the child to have non-specific abdominal pain if GPs used one of the following ICPC codes: D01 (general abdominal pain), D02 (stomach pain), D06 (localized abdominal pain), and D12 (functional constipation). All other diagnoses were categorized as organic abdominal pain. If the GP did not code the diagnosis, two medical doctors coded the diagnosis with the information from the EMR.
Mental health problems
Mental health problems were assessed with the Child Behavior Checklist (CBCL) parent report. The CBCL provides a global measure of psychopathological symptoms [Citation16,Citation17]. We analysed the depressive, anxiety, and somatic problem scales orientated in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV, American Psychiatric Association 1994) [Citation18]. A score of ≥ 93rd percentile scores of norm children is considered deviant. Norm scores are derived from a general population of children with comparable cultural and economical background to our study population (norm children 6–17 years n = 1753, 4–6 years n = 700) [Citation19]. A child with a deviant score on the DSM orientated scales has symptoms suggesting a mental disorder conforming to the DSM-IV classification and is referred to as having a mental problem. According to the DSM-IV classification, children cannot be diagnosed as having a somatization disorder as they can never fulfil the described criteria of the DSM-IV due to both immaturity and the stipulated duration of symptoms. The CBCL classification of a somatic problem means that the children who fulfil this classification have multiple non-specific somatic symptoms.
Statistical analyses
The prevalence of mental health problems was calculated at baseline and at 12 months follow-up; the difference in prevalence was tested with McNemar's test. The cumulative incidence of mental health problems during follow-up was calculated among children who did not have mental health problems at baseline. Among children who had mental health problems at baseline we calculated the percentage of children who had persisting mental health problems at 12 months. In addition the prevalence of mental health problems at follow-up was compared with the prevalence in norm children (7% of n = 2453) and relative risks were presented. CIA version 1.0 (MJ Gardner & British Medical Journal, 1989, London) was used to calculate these indices with their corresponding 95% confidence intervals (CI).
To investigate the association between abdominal pain characteristics during follow-up and mental health status at 12 months we used logistic regression analysis. The presence of either a depressive, an anxiety, or a somatic problem was used as dependent variable. Chronic abdominal pain during follow-up (yes vs. no), duration (months), severity (0–5), frequency (0–5), and the GP's diagnosis (non-specific versus organic abdominal pain) were used as independent variables. We controlled for age, sex, referral to mental health care (yes/no), and baseline scores on the DSM-IV orientated scales of the CBCL. For the latter, we used the continuous baseline scores of the CBCL scales by converting raw scores into scores on a 0–100 scale. The follow-up moments with moderate to severe abdominal pain (pain score of ≥ 3, range 0–10) were summed and used as summary measure for the severity of abdominal pain during follow-up [Citation20]. For the frequency of abdominal pain we summed the number of follow-up moments with five days or more of abdominal pain in the past two weeks. We reported adjusted odds ratios (ORs) with 95% CI. Variables with a significant association (p < 0.02) with the dependent variable were entered into a multivariable logistic regression analysis. We reported these as adjusted multivariable ORs. SPSS for Windows version 15.0 (SPSS Inc.) was used for the analysis.
Results
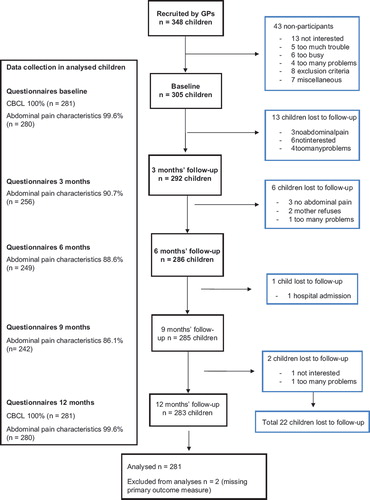
In total 281 children (92.1%) of the 305 children from the HONEUR abdominal pain cohort completed the CBCL at baseline and at 12 months and were included in the analyses (). There were no differences between the children lost to follow-up and those included in the analysis with respect to the prevalence of mental health problems at baseline and the abdominal pain characteristics.
In the baseline characteristics of the 281 children are presented. There were 175 girls (62.3%) and the median age was 7.8 years (interquartile range (IQR) 5.7–10.7). The median duration of abdominal pain in months was 10.5 (IQR 7.5–13.5). According to the GPs, 242 children (86.1%) had non-specific abdominal pain, 32 children (11.4%) organic abdominal pain. For seven children (2.5%) the diagnosis was not coded because of insufficient information in the EMR.
Table I. Characteristics of 281 children aged 4–17 years seen in primary care for a new episode of abdominal pain.
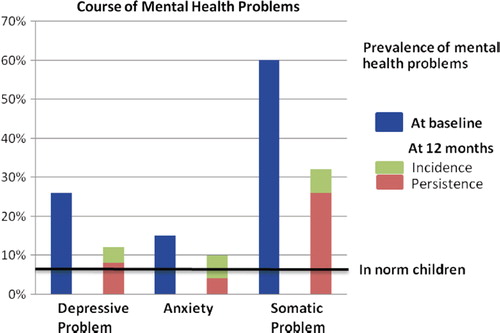
The course of mental health problems is shown in . The prevalence of depressive and somatic problems decreased statistically significant during the one-year follow-up period (p < 0.001). The decrease in anxiety problems was not statistically significant (p = 0.15). The one-year cumulative incidence for depressive problems was 6.3% (95% CI 3.4–10.5%), for anxiety problems was 8.0% (95% CI 5.0–12.2%), and for having multiple non-specific somatic symptoms was 16.2% (95% CI 9.4–23.1%). In total 32.9% (95% CI 22.3–44.9%) of children had persistent depressive problems, 30.2% (95% CI 17.2–46.1%) of children persistent anxiety problems, and 44.1% (95% CI 36.7–51.6%) of children had persistence of multiple non-specific somatic symptoms. Compared with the norm population (presented in with a horizontal line) after 12 months’ follow-up, more children in the study population had a depressive problem (RR 1.9 [95% CI 1.4–2.6]) an anxiety problem (RR 1.6 [95% CI 1.1–2.3]), and multiple non-specific somatic symptoms (RR 4.6 [95% CI 3.7–5.7]).
Details of the association between the abdominal pain characteristics and mental health problems after 12 months’ follow-up are given in . None of the abdominal pain characteristics was associated with a depressive or anxiety problem at 12 months. Only for the number of moments with moderate to severe abdominal was there a significant association (p < 0.02) with the presence of a somatic problem at 12 months.
Table II. Logistic regression analysis examining the effects of abdominal pain characteristics on the risk for a mental health problem at 12 months’ follow-up.
Discussion
In this prospective follow-up study performed in primary care we observed that mental health problems in children with abdominal pain decreased over the course of one year. However, the prevalence of children with a depressive problem, an anxiety problem, or multiple non-specific somatic symptoms after 12 months’ follow-up remained above the prevalence which is found in the general population. After follow-up, one-third of the children had multiple non-specific somatic symptoms. Abdominal pain characteristics did not predict depressive or anxiety problems at 12 months’ follow-up. More moments of moderate to severe abdominal pain predicted the presence of multiple non-specific somatic symptoms at follow-up.
The strength of our study is that we have followed children in general practice with abdominal pain measuring abdominal pain characteristics and mental health problems over time. Therefore, for the first time the association between abdominal pain characteristics and mental health problems of children with abdominal pain could be examined prospectively. To summarize the duration, severity, and frequency of abdominal pain during the follow-up period we used cut-off values based on the literature [Citation20] and expert opinion. We realize that any cut-off value is to a degree arbitrary. However, sensitivity analysis with other cut-off values did not alter the associations reported (data not shown). Earlier we examined whether our cohort adequately represents children consulting the GP with a new episode of abdominal pain [Citation13]. The included children were significantly younger than the identified non-participating children. There was a relative underrepresentation of gastroenteritis and overrepresentation of generalized abdominal pain. As GPs might feel that they have little to offer to children with persisting abdominal pain they might have proposed these children for participation in our cohort study more easily. We do not think, however, there was a selective inclusion of children with mental health problems. Participating GPs were not aware of our research questions and given the few referrals to mental health care in our cohort, we believe that GPs were not aware of the mental health problems of the children included.
To our knowledge, this is the first follow-up study examining the prognosis of depressive, anxiety, and somatic problems of children seen in general practice with abdominal pain. Secondary and tertiary care based studies, merely examining the prognosis of non-specific somatic symptoms, confirm that although mental health problems of children with abdominal pain decrease over time they remain higher than is seen in children from the general population [Citation21–26]. Prognostic factors for the prognosis of mental health problems in children with abdominal pain have hardly been studied.
In children with persisting moderate to severe abdominal pain other non-specific somatic symptoms also persist. It is striking that at 12 months’ follow-up one-third of our study population still had above-normal levels of non-specific somatic symptoms in comparison with 7% of the general population. The coexistence of abdominal pain and other non-specific somatic symptoms has frequently been found before [Citation27], and it raises the question of whether childhood NSAP is a separate functional syndrome and whether it is a precursor of a somatization disorder over time [Citation28].
Clinical implications
As children seen in primary care with abdominal pain are at increased risk for persisting mental health problems we recommend following up these children over time. We feel it is important to include in the anamnesis questions on medically unexplained, non-specific somatic symptoms in other bodily systems such as headaches, limb pains, or tiredness. We think that children with persisting non-specific somatic symptoms particularly need further special attention from GPs by means of further mental health assessment and by means of follow-up, as children with multiple somatic complaints have a short- and long-term psychosocial impairment [Citation29,Citation30]. As until now no studies have been performed on the effectiveness of any type of intervention in children with abdominal pain and mental health problems in primary care, there is no evidence to promote an early (psychological) intervention in these children.
Future research
The prognosis for mental health problems in children with abdominal pain should be further studied. Knowledge of factors that influence the prognosis is necessary as they might be targets for intervention and can help the clinician to recognize a child at risk of future mental health disorders. We think it is important to develop treatments for children seen in primary care with multiple non-specific somatic symptoms and to study the effects of early interventions.
Conclusions
Although mental health problems in children seen in primary care for abdominal pain decrease over time, children with abdominal pain still have more mental health problems after one year of follow-up than children in the general population. Duration, frequency, and severity of abdominal pain during the follow-up period did not predict the presence of depressive and anxiety problems after 12 months. Persisting moderate to severe abdominal pain predicted multiple non-specific somatic symptoms. We recommend following up over time the children seen in primary care with abdominal pain, especially those with multiple non-specific somatic symptoms.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Chitkara DK, Rawat DJ, Talley NJ. The epidemiology of childhood recurrent abdominal pain in Western countries: A systematic review. Am J Gastroenterol 2005;100:1868–75.
- Perquin CW, Hazebroek-Kampschreur AA, Hunfeld JA, Bohnen AM, van Suijlekom-Smit LW, Passchier J, . Pain in children and adolescents: A common experience. Pain 2000;87:51–8.
- Apley J, Naish N. Recurrent abdominal pains: A field survey of 1,000 school children. Arch Dis Child 1958;33:165–70.
- Stordal K, Nygaard EA, Bentsen BS. Organic abnormalities in recurrent abdominal pain in children. Acta Paediatr 2001;90:638–42.
- Gieteling MJ, Bierma-Zeinstra SMA, Passchier J, Berger MY. Prognosis of chronic or recurrent abdominal pain in children. J Pediatr Gastroenterol Nutr 2008;47:316–26.
- Campo JV, Bridge J, Ehmann M, . Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics 2004;113:817–24.
- Garber J, Zeman J, Walker LS. Recurrent abdominal pain in children: Psychiatric diagnoses and parental psychopathology. J Am Acad Child Adolesc Psychiatry 1990;29:648–56.
- Youssef NN, Murphy TG, Langseder AL, Rosh JR. Quality of life for children with functional abdominal pain: A comparison study of patients’ and parents’ perceptions. Pediatrics 2006;117:54–9.
- Di Lorenzo C, Colletti RB, Lehmann HP, Boyle JT, Gerson WT, Hyams JS, . Chronic abdominal pain in children: A technical report of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 2005;40:249–61.
- Hotopf M, Carr S, Mayou R, . Why do children have chronic abdominal pain, and what happens to them when they grow up? Population based cohort study. BMJ 1998;316:1196–1200.
- Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, . Childhood functional gastrointestinal disorders: Child/adolescent. Gastroenterology 2006;130:1527–37.
- Williams N, Jackson D, Lambert PC, Johnstone JM. Incidence of non-specific abdominal pain in children during school term: Population survey based on discharge diagnoses. BMJ 1999;318:1455.
- Spee LAA, van den Hurk APJM, van Leeuwen Y, Benninga MA, Bierma-Zeinstra SM, Passchier J, . Childhood abdominal pain in primary care: Design and patient selection of the HONEUR abdominal pain cohort. BMC Fam Pract;11:27.
- Walker LS, Smith CA, Garber J, Van Slyke D. Development and validation of the Pain Response Inventory for Children. Psychological Assessment 1997; 9:392–405.
- Lamberts H, Wood M, Hofmans-Okkes IM. ICPC. International classification of primary care. Oxford: Oxford University Press; 1987.
- Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms & Profiles. Burlington, VT: University Center for Children, Youth & Families; 2000.
- Achenbach TM, Rescorla LA. Manual of the ASEBA school age forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001.
- Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV). Washington, DC: American Psychiatric Association; 1994.
- Achenbach TM, Rescorla LA. Multicultural supplement of the manual for the ASEBA school age forms and profiles. Burlington VT: University of Vermont, Research Center for Children, Youth & Families; 2007.
- Von Baeyer CL, Walker LS. Children with recurrent abdominal pain: Issues in the selection and description of research participants. J Dev Behav Pediatr 1999;20:307–13.
- Walker LS, Garber J, Greene JW. Somatization symptoms in pediatric abdominal pain patients: Relation to chronicity of abdominal pain and parent somatization. J Abnorm Child Psychol 1991;19:379–94.
- Walker LS, Garber J, Greene JW. Somatic complaints in pediatric patients: A prospective study of the role of negative life events, child social and academic competence, and parental somatic symptoms. J Consult Clin Psychol 1994;62: 1213–21.
- Walker LS, Garber J, Van Slyke DA, Greene JW. Long-term health outcomes in patients with recurrent abdominal pain. J Pediatr Psychol 1995;20:233–45.
- Walker LS, Claar RL, Garber J. Social consequences of children's pain: When do they encourage symptom maintenance? J Pediatr Psychol 2002;27:689–98.
- Walker LS, Smith CA, Garber J, Claar RL. Testing a model of pain appraisal and coping in children with chronic abdominal pain. Health Psychol 2005;24:364–74.
- Mulvaney S, Lambert EW, Garber J, Walker LS. Trajectories of symptoms and impairment for pediatric patients with functional abdominal pain: A 5-year longitudinal study. J Am Acad Child Adolesc Psychiatry 2006;45:737–44.
- Hotopf M, Mayou R, Wadsworth M, Wessely S. Childhood risk factors for adults with medically unexplained symptoms: Results from a national birth cohort study. Am J Psychiatry 1999;156:1796–800.
- Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: One or many? Lancet 1999;354:936–9.
- Campo JV, Jansen-McWilliams L, Comer DM, Kelleher KJ. Somatization in pediatric primary care: Association with psychopathology, functional impairment, and use of services. J Am Acad Child Adolesc Psychiatry 1999;38:1093–101.
- Essau CA. Course and outcome of somatoform disorders in non-referred adolescents. Psychosomatics 2007;48:502–9.