The shortage of clinical research is a problem that has been addressed by clinicians, researchers, health authorities, and politicians alike [Citation1,Citation2]. Although hospital-based research is subject to this problem, it is even more pronounced in primary care. This is especially worrisome considering that the most common health problems are found in primary care – and stay there. Results from clinical research are often not generalizable to another context, which means that hospital-based clinical research may not apply to general practice.
What are the reasons for the lack of clinical research?
Inclusion of patients in studies is time-consuming and labour-intensive, and this is particularly true in primary care where the patient data are decentralized. The researcher has to go through a two-step process; first to recruit every single practitioner for the study, and second to support the clinician in recruiting patients to participate. And this has to be done over and over again for each patient and each study.
The clinicians face trouble, too. Invitations to partake in studies come unpredictably, which increases the risk of declining. Furthermore, the invitations come without advice from scientifically as well as clinically competent authorities. Each practice or even each single GP must decide whether the research project has the necessary scientific standard or clinical relevance. Lacking the competence to assess this may result in declining to participate due to uncertainty. In contrast, many clinicians may be interested in participating in research if a minimum framework is in place. Such a framework must include support for practical tasks, training, available time from other duties, reasonable funding, and motivation for the project in terms of relevance for one's own practice [Citation3].
In Norway, general practice is generally organized as private enterprises after the registered list system reform in 2001. This further creates some challenges for research: Who is to pay for the extra time it takes to consider participation in a study, to recruit patients including getting informed consent, and to obtain the necessary data and report back to the researcher? Professional research cannot be based on sheer goodwill from GPs who work in a fee-for-service healthcare system. This has to be addressed in efforts to strengthen clinical research in our field.
The current situation represents a waste of time for clinical researchers and a waste of resources for society. It provides no predictability for the clinicians and the practices, and it reduces our patients’ opportunity to participate in research and development that is in their own interests. Simply put, steps have to be taken to change the situation.
In 2010, Norwegian researchers in general practice and oral health found that we have common challenges in this regard. We have since worked together to establish research networks for general practice and oral health in Norway. Research networks in primary health and oral health care are infrastructures of clinical practices linked together by a research institution with employees who actively recruit clinicians to the network and help them stay “research ready”. Furthermore, when initiating research studies, the network supports recruitment of patients and obtainment of data in order to reduce the burden on the clinician as much as possible. Research networks already exist in Great Britain, the Netherlands, and a number of other countries [Citation4–6]. And they not only exist – some are really successful in terms of quality and relevant findings [Citation7,Citation8]. In addition to supporting acquirement of high-quality data with less effort for each research project, they also support international collaboration [Citation8].
In 2012, the Norwegian Directorate of Health requested a report on the topic and gave financial support to elaborate on the prerequisites to establish networks in Norway. Study trips to Great Britain and the Netherlands, as well as small-scale studies, were carried out. In May 2014, an international meeting on research networks was arranged in Bergen, Norway, with participants from Scotland, Canada, the Netherlands, and Denmark. Professor Frank Sullivan (Canada/Scotland) put it this way: “A research network may be viewed as the laboratory of primary care research. Who would ever dream of asking basic researchers to set up and tear down their laboratory for each single research project? So why should we carry on in such an old-fashioned way?”
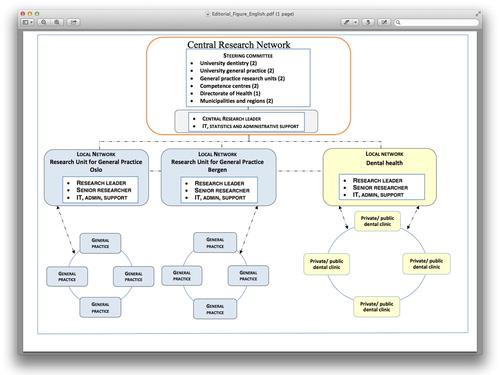
The report was published in 2013, outlining a possible organization () and funding of research networks [Citation2], and a short version in English has also been published [Citation9]. The costs of a first stage of the network were estimated at 25 million Norwegian kroner (just over 3 million euros) annually. It should be no surprise that clinical research costs money in primary care as well as in secondary care, where the spending is much higher. The idea of research networks is supported by the new strategy process for health research in Norway (HelseOmsorg 21) [Citation10] and by an external review of the strategy process [Citation11]. Considering the indefensibly low investment in general practice research, the time has come for some change to the benefit of our patients.
Figure 1. A possible model for a first step for research networks in Norwegian primary health and oral health care. A fully fledged model will include two additional local networks in general practice, linked to the research units in Trondheim and Tromsø. The model may be expanded to include other primary care services at a later stage.
Establishment of research networks in the oral health and primary health care services will be a response to current and future challenges in the services. The challenge is now in the hands of the health authorities and politicians.
References
- Nasjonal helse-og omsorgsplan (2011–2015) [National Health Care Plan (2011–2015)]. Oslo, Norway: Helse-og Omsorgsdepartementet; 2011.
- Rørtveit G, Espelid I, Straand J, Klock K. Forskningsnettverk i allmennmedisin og tannhelsetjenesten [Research networks in general practice and oral health services]. Bergen, Norway: Uni Research Health; 2013. Available online at: http://helse.uni.no/upload/Rapport_Hdir_Forskningsnettverk_2013_m_vedlegg.pdf
- Malterud K. Forskningsnettverk i allmennpraksis. Hva skal til for å få fastleger til å delta? [Research networks in general practice. What can be done to encourage GPs to participate?]. Bergen, Norway: Uni Research Health; 2013. Available online at: http://helse.uni.no/upload/Rapport_Hdir_Forskningsnettverk_2013_m_vedlegg.pdf
- Sullivan F, Butler C, Cupples M, Kinmonth AL. Primary care research networks in the United Kingdom. BMJ 2007;334:1093–4.
- Van Weel C, de Grauw W. Family practices registration networks contributed to primary care research. J Clin Epidemiol 2006;59:779–83.
- Peterson KA, Lipman PD, Lange CJ, Cohen RA, Durako S. Supporting better science in primary care: A description of practice-based research networks (PBRNs) in 2011. J Am Board Family Med 2012;25:565–71.
- Sullivan FM, Swan IR, Donnan PT, et al. Early treatment with prednisolone or acyclovir in Bell's palsy. N Engl J Med 2007;357:1598–607.
- Van Vugt SF, Broekhuizen BD, Lammens C, et al. Use of serum C reactive protein and procalcitonin concentrations in addition to symptoms and signs to predict pneumonia in patients presenting to primary care with acute cough: Diagnostic study. BMJ 2013;346:f2450.
- Rørtveit G, Espelid I, Straand J, Klock K. Research networks in general practice and oral health services. Bergen, Norway: Uni Research Health; 2013. Available online at: http://helse.uni.no/upload/Report_Hdir_ENGLISH.pdf
- HelseOmsorg21. En nasjonal strategiprosess [HealthCare21. A national strategy process]. Oslo, Norway: Research Council of Norway; 2014. Available online at: http://www.forskningsradet.no/prognett-helseomsorg21/Forside/1253985487298
- Grant J, Pollitt A, Castle-Clarke S, Cochrane G, Søndergaard S, Horvath V. Supporting the development of a new health R&D strategy. A rapid review of international theory and practice for Norway’s HelseOmsorg21. United Kingdom: RAND Europe; 2014. Available online at: http://www.forskningsradet.no/prognett-helseomsorg21/Forside/1253985487298
