Abstract
Objective. To find a salutogenic approach for prevention of metabolic syndrome in primary care practice. Design. An explanatory sequential mixed-methods procedure was used to find salutogenic approaches for lifestyle change by assessing individual need, potential, and personal motivation. Data from a population health survey and interviews that focused on a sense of coherence were analysed. Subjects. Altogether 480 Finnish subjects participated in a population health survey, and 43 of them were interviewed. The 43 interviewees’ data were included in the final analysis. Main outcome measures. With the health survey participants’ liability for MetS was assessed, and the objective need for lifestyle intervention was determined. Through the focused interviews potential and personal motivation for lifestyle modification were explored. Finally the data of the 43 interviewed subjects were merged. Results. Four possible lifestyle intervention approaches were identified for specific intervention. First, subjects with a strong sense of coherence only need encouragement to maintain a healthy lifestyle; second, professional support was found important for subjects with gaps in health awareness to improve health understanding; third, strengthening of social support for lifestyle change is necessary for subjects with various practical constraints in their everyday life; and fourth, strengthening of stress adaptation is important for subjects with redundant concerns about their health. Conclusions. Salutogenic client-centred lifestyle modification approaches should be part of primary care practice. Further, a cross-disciplinary approach is needed in primary care research and practice to combat the exploding lifestyle illnesses.
Evidence is scarce regarding the applicability of salutogenic theory and practice to prevention of metabolic syndrome.
Assessment of need, potential, and motivation helps primary care practitioners design individual lifestyle intervention approaches for prevention of metabolic syndrome.
A cross-disciplinary salutogenic approach is suggested for primary care research and practice to combat lifestyle illnesses including metabolic syndrome.
Introduction
Metabolic syndrome (MetS) is an exploding global epidemic. It is caused by a cluster of several risk factors, most of which are associated with unhealthy lifestyles. The syndrome leads to increased cardiovascular morbidity and mortality [Citation1]. Previous research findings indicate that health views strongly reflect health behaviour and consequently liability for non-communicable illnesses [Citation2,Citation3].
Researchers today are encouraged to combine a quantitative and a qualitative approach in health sciences to complement each other [Citation4]. However, a mixed-methods approach is not widely applied in the research of non-communicable diseases. Merging quantitative and qualitative research would deepen present understanding of the complexity of the association between lifestyles and public health problems such as MetS.
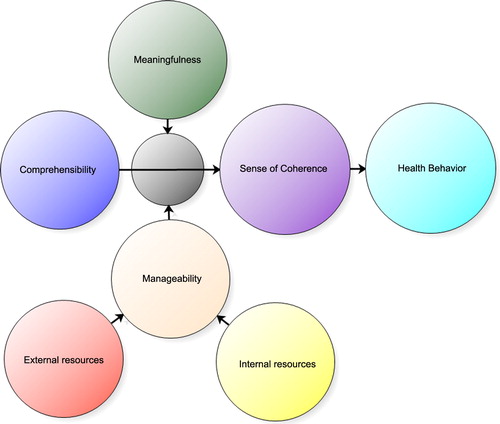
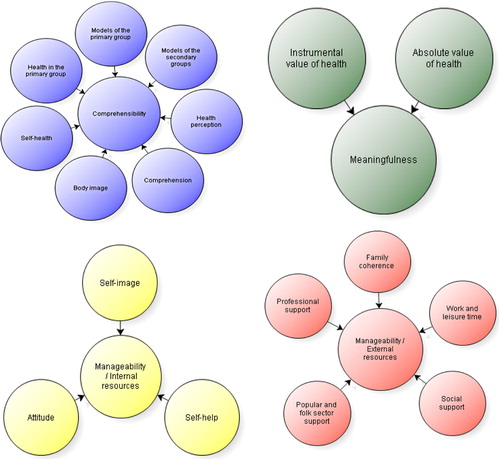
The concept of salutogenesis [Citation5,Citation6] as an opposite of pathogenesis is based on the presence of internal (intrapersonal) and external (social and societal) general resistance resources (GRR), which are necessary for coping with a range of physical and psychosocial stressors. Internal and external social and societal resources are shaped by cultural models [Citation7] and social capital [Citation8]. The concept can be measured quantitatively or explored qualitatively by determining the level of sense of coherence (SOC), which is a global orientation of human beings towards stressful life situations. The three dimensions of SOC are comprehensibility, meaningfulness, and manageability [Citation5,Citation6].
Quantitative (SOC) instruments have been constructed mainly for public health research purposes to measure individual capacity to cope in a salutogenic way [Citation9,Citation10]. The accuracy of these instruments has been criticized [Citation11]. However, the salutogenic approach is worth more investigation in public health research to gain more understanding of its applicability to primary care practice [Citation12]. There are only few research reports on the association of SOC with lifestyle-related cardiovascular risks, and MetS in particular [Citation13,Citation14].
By determining the subject's verified need, potential, and personal motivation for lifestyle modification in the current life situation, we explored applicability of new individual lifestyle intervention schemes at primary care level. Our approach was firmly grounded in the concept of salutogenesis.
Material and methods
We applied an explanatory sequential mixed-methods procedure, which merged quantitative epidemiological data obtained from a health survey, and subsequent qualitative data of focused interviews of 43 subjects. With the health survey (quantitative study) we determined participants’ MetS status, and probability for MetS (presence of two out of the five MetS criteria), and consequently assessed the verified need for interventions. Through the interviews we explored potential and personal motivation for lifestyle modification. Finally we merged all the data for final analysis. The target population was adults between the ages of 30 and 65 years at five-year birth intervals living in a Finnish semi-rural community.
We carried out our research project in three phases, the first two of which involved postal questionnaire study and health survey (quantitative methods), and the third phase involved personal interviews of 43 volunteers from the same group (qualitative methods). presents the research process and participation in each research phases.
The project started in 2004 with a postal questionnaire survey, continued in 2005 with a health survey of the respondents to the postal questionnaire survey, and was finalized by an interview study in 2006. We completed the analysis of the health survey data of 480 study participants by 2008, and the analysis of the interviews by 2009. Consequently from 2009 to 2010, we combined the data of the quantitative and qualitative analysis of the 43 interviewees. The research project was reported in 2011 as the first author's PhD thesis (in Finnish).
Postal questionnaire study
For the postal questionnaire survey in 2005, we invited all 760 adult community members born in 1939, 1944, 1949, 1954, 1959, 1964, 1969, and 1974 (age range from 30 to 65 years of age). This was 10% of the total population of 7513 living in the community. Altogether 594 (78%) of the invited adult community members responded to the postal questionnaire. The respondents reported their own and their first-degree relatives’ (parents, siblings, children) cardiovascular illnesses and diabetes. They also reported their own smoking status, level of all physical exercise, and weight and height.
Health survey
Of the 594 respondents to the postal questionnaire study, 480 (63%) (230 men (59%) and 250 women (68%)) participated in a complete health survey. It consisted of a structured health questionnaire and a health examination. The health questionnaire included socio-demographic information, further statements on lifestyles, and health views. The questionnaire also included the BDI-21 inventory for assessment of self-reported mood, and the 15D questionnaire that measures subjective health related quality of life (HRQoL).
The BDI-21 questionnaire was sent to 405 subjects after the health survey, while it was included in the master health survey questionnaire of 75 subjects. Of the 480 study participants in the health survey, 442 (211 men and 231 women) filled in the BDI-21 inventory [Citation15]. Of these, 26 subjects with incomplete data were excluded from the analysis leaving a total of 416 subjects (55% of the age cohorts) for the final analysis. The BDI-21 total score was the sum score of the 21 separate BDI items, which contain four statements each, reflecting the intensity of a particular item of mood. The BDI-21 items are: mood, pessimism, sense of failure, lack of satisfaction, guilty feelings, sense of punishment, self-hate, self-accusation, self-punitive wishes, crying spells, irritability, social withdrawal, indecisiveness, body image, work inhibition, sleep disturbances, fatigability, loss of appetite, weight loss, somatic preoccupation, and loss of libido.
The 15D instrument is a 15-dimensional, standardized, self-administered questionnaire of HRQoL that can be used both as a profile and as a single index score measure [Citation16]. The 15 dimensions are: mobility, vision, hearing, sleeping, breathing, eating, speech, elimination, usual activities, mental function, discomfort and symptoms, depression, distress, vitality, and sexual activity. For each dimension, the respondent chooses one of five levels (ranked from one to five) that best describes his/her state of health at the moment. The valuation system of the 15D instrument is based on an application of the multi-attribute utility theory. A set of utility or preference weights, elicited from the general public through a three-stage valuation procedure, is used first to generate level values for each dimension on a 0–1 scale (1 = no problem; 0 = being dead) and then to aggregate them additively into an overall HRQoL score, i.e. a 15D score (a single index number) over all the dimensions on a scale of 0–1 (1 = no problem; 0 = being dead).
The health examination involved anthropometric measurements, measurement of blood pressure and heart rate, and blood tests which all were used for MetS diagnosis. Weight was taken in light clothing (Seca standing scale) to the nearest 0.1 kg and height was measured in a standing position to the nearest 1.0 cm. Body mass index (BMI) was calculated from the formula: weight/height2. Waist circumference was measured at the midpoint between the lowest rib and the iliac crest, and blood pressure was taken in a sitting position at five-minute intervals after 10 minutes of rest. For the blood pressure measurements, we used a calibrated Omron M4-1 semi-automatic device (Omron Healthcare Co Ltd, Kyoto Japan), and a mercury sphygmomanometer in situations where manual measurement was the only reliable recording method. For the statistical analysis, we calculated the means of the three measurements. Glucose level was tested from capillary blood with a glucometer calibrated for plasma glucose level, and other laboratory tests were done from the serum of a venous blood sample after 12 hours of fasting. All the laboratory investigations were performed according to the routine protocol of the Medical Laboratory of Kuopio University Hospital.
We used the NCEP 2005 criteria for MetS definition [Citation17]. MetS was defined from anthropometric measurements and blood test results. The presence of at least three of the five NCEP 2005 MetS criteria classified the subject as having MetS, and two criteria classified the subjects as being liable to developing MetS later on in his/her life. The criteria are as follows: (i) fasting plasma glucose level ≥ 5.6 mmol/l and/or diabetes medication or previously diagnosed adult type diabetes, (ii) serum triglyceride level ≥ 1.7 mmol/l and/or medication, (iii) serum HDL cholesterol level < 1.03 mmol/l in men and < 1.29 mmol/l in women and/or medication, (iv) systolic blood pressure ≥ 130 mm Hg and/or diastolic blood pressure ≥ 85 mmHg and/or antihypertensive medication, (iv) waist girth > 102 cm for men and > 88 cm for women.
Focused interviews
The final phase of the study consisted of tape-recorded interviews, which were all transcribed. All health survey participants accepted to be interviewed. However, only 43 interviewees were selected as this was considered to be a sufficient amount for the required information. As qualitative research is meant to describe phenomena and not yield representative results, we applied purposive sampling by selecting interviewees evenly from both genders, and all age cohorts. Half of the interviewees filled MetS criteria and half did not. The only exclusion criterion was too close a relationship between the interviewee and interviewer, which was considered very important in such a small community. The first author (JM), who has practised since 1979 as a GP in the same community, and who shares the Savo dialect of the Finnish language with most of the interviewees, conducted all interviews. The interviews covered health and health service related themes. We focused on salutogenic themes to assess the level of SOC. Average time of one interview was 97 minutes.
To understand messages and meanings of the interviewees, the first author (JM) listened to all taped interviews twice while checking correctness of the transcribed texts. The first author (JM) helped the second author (AMV, anthropologist) to understand some Savo dialect expressions that were used particularly by some interviewees belonging to the older age cohorts. The first (JM) and the second (AMV) author read through all the texts for analysis. Consequently, both researchers analysed the contents first separately, and consequently they compared the findings in a series of discussions. All this was done for the sake of reliability and validity (trustworthiness). Triangulation was supported by comparing the interview findings with the statements of the interviewees on health and health service views in the health questionnaire. [Citation18]
Further, the contents of the interviews were analysed using NVivo 7 software for qualitative research [Citation19]. This methodology supported triangulation. The software was used to code and categorize the contents, to quantify some attributes, and to support reporting of the findings (illustrations of SOC assessment were drawn accordingly).
The SOC status of each interviewee was assessed from the presence of all three elements of SOC (comprehensibility, meaningfulness, manageability) as described in . The researchers agreed on the sub-elements of the three SOC elements (). NViVo 7 software was utilized for grouping and categorizing the findings according to the SOC elements and sub-elements.
Merging of the quantitative and qualitative study findings
Finally, the findings of the quantitative and qualitative research of the 43 interviewees were combined. illustrates the merging process. As a result, an individual lifestyle profile was constituted for each subject. This profile served as baseline information for assessment of individual lifestyle intervention prospects. The merging process also aimed at designing appropriate lifestyle intervention approaches for the identified lifestyle profile groups.
Figure 4. Lapinlahti 2005 study: Merging process of qualitative and quantitative data (MetS = metabolic syndrome; SOC = Sense of Coherence).
There were three key prerequisites for lifestyle intervention, namely the verified need, individual potential, and personal motivation for lifestyle modification in the current life situation. The need for traditional lifestyle intervention (diet, physical exercise, smoking, and use of alcohol) was assessed from the health survey questionnaire. The need for psychosocial intervention was assessed from the interview findings. The potential (internal and external resources) and personal motivation for lifestyle intervention was obtained from the interview findings. Individual intervention prospects were based on the SOC status of the interviewees against the verified objective need for intervention.
Results
Health survey results
Prevalence and liability of metabolic syndrome
indicates the basic characteristics of the 480 health survey participants. Nearly four our of 10 health survey participants (n = 480) had MetS according to the definition by the National Cholesterol Education Program (NCEP) Adult Treatment Panel III in 2005. Only 10.6% of all study participants had no MetS criteria, while 26.2% had one criterion. In all, 24.5% had two criteria. This group was regarded as liable to develop MetS in the future (liability for MetS). Another 18.1% had three, 13.1% had four, and 6.8% had all five MetS criteria.
Table I. Lapinlahti 2005 study: Basic characteristics of the 480 study subjects.
Metabolic syndrome, socioeconomic factors, and lifestyle in men and women
Association between MetS, socioeconomic factors, and lifestyle was more prominent in women than in men. Statistically significant differences were found only in women between MetS and the following: low vocational education (p = 0.007), low physical activity (p = 0.007), and low vegetable intake (p = 0.005).
Final findings
Lifestyle intervention prospects
Of the 43 interviewees, 18 subjects were assessed as having very good prospects, and 15 subjects as having good prospects for lifestyle betterment. Of these 33 subjects, 20 individuals met the NCEP MetS definition or were liable (had two MetS criteria) to develop MetS later on in their lives. The impact of their lifestyle intervention was assumed to be good. Of the remaining 10 interviewees, the intervention prospects of whom were regarded as poor, nine participants had MetS.
Lifestyle profile groups
Based on individual assessments, six lifestyle profile groups were found. These were: “Weak or Fake Sense of Coherence”, “Poor Valuation of Health”, “Poor Health Awareness”, “Defective External Resistance Resources”, “Defective Internal Resistance Resources”, and “Strong or Strengthening Sense of Coherence”. The summary of the combined results of health survey and interviews are presented in .
Table II. Lapinlahti 2005 study: Summary of the health survey and theme interview findings of 43 study participants.1
All but one of the 12 participants in the group of “Weak or Fake Sense of Coherence” had MetS. In the same group, nine participants were assessed as having poor lifestyle intervention prospects due to their low potential and low personal motivation for lifestyle modification. Similarly in the group of “Defective External Resistance Resources”, all but two participants had MetS or were liable to develop it. However, all participants in this group were assessed as having good or very good lifestyle intervention prospects due to their high personal motivation towards lifestyle modification, though their potential was seen as somewhat limited mainly due to external factors. Motivation for lifestyle change was assessed as high also in the groups “Defective Internal Resistance Resources” and “Strong or Strengthening Sense of Coherence”.
Participants in the groups “Defective External Resistance Resources”, “Defective Internal Resistance Resources”, and “Strong or Strengthening Sense of Coherence” would require a totally new approach for lifestyle modification. All participants in the groups “Poor Valuation of Health” and “Poor Health Awareness” were assessed as having good or fairly good lifestyle intervention prospects. However, they would require an improved conventional lifestyle intervention (health awareness support) to increase their level of health understanding.
Discussion
Principal findings
The prevalence of MetS in the present study was at the same level as in other previous population studies in Finland. Association between MetS and socioeconomic factors as well as lifestyle indicators was more prominent in women than in men. Based on our findings, MetS may be clustered in the group of “Weak or Fake Sense of Coherence”. However, these interview (qualitative study) findings are not representative for the whole population. When we combined quantitative and qualitative research findings, we identified six SOC lifestyle profile groups that require specific style intervention approaches in primary health care. We also found a cross-disciplinary approach important for health promotion and prevention of lifestyle illnesses at primary care level.
Remarks on the final study findings: clinical implications
Based on the profile grouping, four feasible lifestyle intervention approaches were identified for primary care practice. Subjects in the group “Strong or Strengthening Sense of Coherence” are more or less on the safe side, and they only need encouragement to maintain their healthy lifestyle. The second approach could be professional support to improve health understanding of subjects in the groups “Poor Valuation of Health” and “Poor Health Awareness”. The third approach could be support of external resistance resources of subjects in the group “Defective External Resistance Resources”. Most subjects in this group had practical constraints in everyday life that may critically jeopardize their efforts for lifestyle change. This concern applies particularly to women with various responsibilities in their primary groups (family, close relatives), and to young work-oriented family men. The fourth approach could be support of internal resistance resources of subjects in the group “Defective Internal Resistance Resources”. Due to personality features, these subjects may also suffer from poor stress adaptation, which may predict some cardiovascular risk factors such as high blood pressure. In our study, most of the subjects in this group represented redundant concern regarding their health.
Subjects in the group “Weak or Fake Sense of Coherence” may be quite resistant to any welfare intervention due to their low personal motivation and weak potential, which is mainly inability to make use of their internal and external resources. For that reason, the impact of their lifestyle intervention might be quite poor, or at least would require much more effort than is required for subjects in the other groups.
Strengths and weaknesses
It is rather difficult to combine representative epidemiological study results with non-representative interview findings. However, by interviewing 43 study participants we managed to acquire enough information to construct theoretical profiles for feasible lifestyle intervention schemes. The quantitative data may be considered as quite outdated. However, the results on the prevalence of MetS, cardiovascular risk factors, and their association with lifestyle and health views are still well up-to-date. Further, the findings of the interviews as to perceptions in general and health views in particular are quite resistant to changes over a short period of time [Citation20].
An obvious strength of the quantitative study is its full coverage of the target population. The participants represented quite well the population groups most at risk of MetS. However, the participation in the health survey was fairly low (63%), which may affect the final results. Though analysis of non- participation was not carried out, we assume that rather sensitive questions in the BDI-21 and 15D-questionnaires may have reduced participation. We presume also that there are a number of other reasons for the non-participation.
We could probably have gained the same information and with a lower workload by using one of the quantitative SOC instruments. The qualitative SOC assessment used was supported by the fact that the interviews helped us to construct more complete individual health profiles, and that they also produced additional information for other research purposes.
This research project was a novel effort to combine epidemiological and interview research strands in public health research. Merging qualitative and quantitative data always bears some biases of which researchers’ influence is not the least important. However, we can claim that this concern is also relevant for clinical encounters where the practitioner makes clinical decisions based on both accurate measurements and his/her subjective assessment.
Findings in relation to other studies
Our MetS prevalence figures are well in line with previous prevalence figures in Finland and other high-income countries [Citation21–23]. A stronger association was found among women than among men between MetS, health-related lifestyles, and some socioeconomic variables. This finding is also in line with previous knowledge [Citation24,Citation25].
As opposed to the participants with good or very good intervention prospects, the impact of lifestyle intervention of the participants with poor prospects was assumed to be rather poor mainly due to their low level of personal motivation towards lifestyle change. Our findings are supported by the findings of the quantitative SHIELD study, which compared health-related attitudes and behaviour of three different groups. In that study, these groups were called “I'm Doing”, “I Should Do” and “Don't Bother Me”. On one hand, the “Don't Bother Me” group in the SHIELD study consisted of people at high risk of MetS, as did our group “Weak or Fake Sense of Coherence”. They were characterized by poor concern about their diet, overall nutrition, and fitness and preference for medication rather than lifestyle change. The SHIELD study summarized that even with substantial external support these people may never embrace change in their health-related attitudes. On the other hand, the “I'm Doing” participants were more prone to healthy dietary choices and physical exercise and less adherent to medication than were the participant in the other groups [Citation2].
Further, in a Swedish interview study of an adult community with members having MetS, interviewees represented neglectful and fatalistic attitudes towards life. They also emphasized genetic reasons behind their condition. [Citation26] This study strongly supports findings in our study that demonstrated unwillingness of the poorly motivated high-risk interviewees to change their health behaviour. This was one contributing factor to their poor intervention prospects in our assessment.
Meaning of the findings
The findings of the present study suggest the need for new approach in health promotion and lifestyle change at primary health care level for reduction of the burden of cardiovascular illnesses. Health counselling should be client-centred taking into account the verified individual needs and personal motivation, and it should adhere to the current life situation and the sociocultural setting. Further, health professionals should support clients’ external and internal resistance resources, not forgetting psychosocial resources. All measures should be based on the confirmed need, potential, and personal motivation in the life context of the client. From these study findings, we assume that this approach could also be applied to prevention and management of other lifestyle-related conditions.
Assessment of sense of coherence could be combined with motivational interviewing [Citation27] for client-centred health education in primary health care practice. This could be tested in clinical settings.
Ethical consideration
The research project was approved by the Ethical Committee of Kuopio University Hospital and the University of Eastern Finland.
Funding acknowledgements
The study would not have been possible without the financial support of the municipality of Lapinlahti, Finnish Cultural Foundation and the Development Programme for the Prevention and Care of Diabetes in Finland (DEHKO/D2D) through the Northern Savo Hospital District.
Declaration of interest
There are no conflicts of interest in connection with the paper. The authors alone are responsible for the content and writing of the paper.
References
- Galassi A, Reynolds K & He J. Metabolic syndrome and risk of cardiovascular disease: A metaanalysis. Am J Med 2006; 119:812–19.
- Lewis SJ, Rodbard HW, Fox KM, Grandy S & SHIELD Study Group. Self-reported prevalence and awareness of metabolic syndrome: Findings from SHIELD. Int J Clin Pract 2008;62:1168–76.
- Miettola J, Nykanen I & Kumpusalo E. Health views and metabolic syndrome in a Finnish rural community: A cross-sectional population study. Can J Rural Med: official journal of the Society of Rural Physicians of Canada = Journal canadien de la médecine rurale: le journal officiel de la Société de médecine rurale du Canada 2012;17:10–16.
- O’Cathain A. Editorial: Mixed methods research in the health sciences: A quiet revolution. J Mixed Methods Res 2009;3:3–6.
- Antonovsky A. Health, stress, and coping. San Francisco: Jossey-Bass; 1979.
- Antonovsky, A. Unraveling the mystery of health. San Francisco: Jossey-Bass; 1987.
- Potter J, Wetherell M. Discourse and social psychology: Beyond attitudes and behaviour. London: Sage Publications; 1987.
- Kunitz SJ. Social capital and health. Br Med Bull 2004;69: 61–73.
- Antonovsky A. The structure and properties of the sense of coherence scale. Soc Sci Med 1993;36:725–33.
- Eriksson M, Lindstrom B. Antonovsky's sense of coherence scale and its relation with quality of life: A systematic review. J Epidemiology Community Health 2007;61:938–44.
- Flensborg-Madsen T, Ventegodt S, Merrick J. Why is Antonovsky's sense of coherence not correlated to physical health? Analysing Antonovsky's 29-item Sense of Coherence Scale (SOC-29). Scientific World J 2005;5:767–76.
- Lindstrom B, Eriksson M. Salutogenesis. J Epidemiology Community Health 2005;59:440–2.
- Konttinen H, Haukkala A, Uutela A. Comparing sense of coherence, depressive symptoms and anxiety, and their relationships with health in a population-based study. Social Sci Med 2008;66:2401–12.
- Ochiai R, Daitou S, Aoki K. Relationship between sense of coherence and lifestyle in middle-aged workers in Japan. Health 2012;1:20–5.
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561–71.
- Sintonen H. The 15D instrument of health-related quality of life: Properties and applications. Ann Med 2001;33: 328–36.
- Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: An American Hearth Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735–52.
- Golafshani N. Understanding reliability and validity in qualitative research. Qualitative Report 2003;8:597–607.
- Richards L. Handling qualitative data: A practical guide. London: Sage Publications; 2005.
- Holland D, Quinn N. Cultural models in language and thought. Cambridge: Cambridge University Press; 1987.
- Ford ES. Prevalence of the metabolic syndrome in US populations. Endocrinol Metab Clin North Am 2004;33: 333–50.
- Ilanne-Parikka P, Eriksson JG, Lindstrom J, Hamalainen H, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Mannelin M, Rastas M, Salminen V, Aunola S, Sundvall J, Valle T, Lahtela J, Uusitupa M, Tuomilehto J & Finnish Diabetes Prevention Study Group. Prevalence of the metabolic syndrome and its components: Findings from a Finnish general population sample and the Diabetes Prevention Study cohort. Diabetes Care 2004;27:2135–40.
- Hu G, Lindstrom J, Jousilahti P, Peltonen M, Sjoberg L, Kaaja R, et al. The increasing prevalence of metabolic syndrome among Finnish men and women over a decade. J Clinical Endocrinol Metab 2008;93:832–6.
- Marquezine GF, Oliveira CM, Pereira AC, Krieger JE, Mill JG. Metabolic syndrome determinants in an urban population from Brazil: Social class and gender-specific interaction. Int J Cardiol 2008;129:259–65.
- Santos AC, Ebrahim S, Barros H. Gender, socio-economic status and metabolic syndrome in middle-aged and old adults. BMC Public Health 2008;8:62.
- Frisman GH, Bertero C. Having knowledge of metabolic syndrome: Does the meaning and consequences of the risk factors influence the life situation of Swedish adults? Nursing & Health Sciences 2008;10:300–5.
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. New York: Guilford Press; 2002.