Abstract
Objective. The main aim of the study was to investigate how many and what kind of problems patients present in consultations with their general practitioner (GP). A secondary aim was to explore patients’ views on what is important in consultations. Design. Cross-sectional study including observation of unselected consultations with recording on a pre-designed scheme, and a brief questionnaire filled in by patients. Setting. Four general practices in Oslo, Norway. Subjects. A total of 201 patients in consultations and 177 patients waiting to see their GP. Main outcome measures. Number and characteristics of problems raised by patients, and whether the problems were handled by GPs during the ongoing consultation. Patients’ expectations for the consultation. Results. The mean number of problems raised was 2.6 (range 1–16), and when appointments for acute conditions were excluded, the mean number was 3.3. Somatic problems comprised about half of all problems, and in more than one-quarter of consultations a mental health issue was presented. Female sex and increasing age predicted an increasing number of problems raised. In one-quarter of encounters four or more problems were presented. The vast majority of problems were dealt with by the GPs during the ongoing consultation. “That I am able to address all the problems I have” was rated as highly important by patients. Conclusion. GPs deal with multiple and unrelated problems in daily consultations, which is highly valued by patients. Management of concurrent problems in brief encounters demands training and adequate working conditions, in order to sustain this core value of general practice.
Which problems patients present to their GP in the consultation and how many problems are presented has been little investigated.
Direct observation revealed a mean of 2.6 problems, and four or more were presented in one-quarter of consultations.
A mental health issue was brought up in more than one-quarter of encounters.
The vast majority of problems were dealt with by the GP during the ongoing consultation.
Introduction
A core value in general practice is to understand a patient's problems in a holistic or bio-psycho-social context [Citation1,Citation2]. Over time, the general practitioner (GP) relates to the patient as a person with a unique history and in a specific social and environmental context. When the patient makes an appointment with his/her regular GP, it is mostly the patient who defines what should be on the agenda. The doctor's duty is to explore the patient's symptoms and worries and to deal with them adequately [Citation3]. In contrast, if the patient is referred to a hospital or outpatient clinic, the problem is defined and described a priori.
A GP will frequently have to deal with multiple, complex, or unclear complaints. To do this adequately demands a specific type of competence, more comprehensive and different from traditional knowledge regarding diseases and their treatment [Citation4]. The GP must be able to deal with several “unedited” problems presented during a brief consultation, some of which may be simple and easy to handle, others not.
Which and how many problems patients actually present in consultations with their GPs has been sparsely investigated. Extensive literature searches in January 2013 and September 2014 revealed only a few publications [Citation5–9], none of them carried out in a Scandinavian setting. In a study from the US Flocke et al. found that on average 2.7 problems and eight physician actions were observed during an encounter [Citation5]. More than one problem was addressed in three out of four consultations, and each additional problem increased the length of the visit by 2.5 minutes. Beasley et al., also in the US, found that an average of 3.1 problems were presented per consultation [Citation6], while a recent study from the UK found an average of 2.5 problems per consultation, increasing with the patient's age [Citation7]. In a comprehensive study from the US in 1998, almost 4500 GP consultations were directly observed by research nurses, revealing the average number of problems presented in each consultation to be 2.3 [Citation8]. In a study from 2007 comparing GP consultations in Australia, New Zealand, and the US, Bindman et al. found that primary care physicians dealt with an average of 1.4 medical problems per visit [Citation9]. However, in this study the total number of recorded problems was limited to three per consultation in the US and four in Australia and New Zealand, and preventive and administrative tasks were excluded. Also, the GPs themselves recorded the problems on separate encounter sheets, which would tend to limit the number of problems recorded.
Because its contents have been so little exposed, the GP consultation has been called a “Black Box” [Citation8]. The main aim of the present study was to shed some light into this “Black Box” in a Norwegian setting. Based on personal experience and former research [Citation5–9], our hypotheses were that patients more often than not present several unrelated problems in one single consultation, and that these are handled by the GP. Our secondary aim was to explore patients’ expectations when going to see their GP.
Material and methods
Design, setting, and data collection
We conducted a cross-sectional observational study in four general practices in the city of Oslo, Norway, in 2013. The first author (EB, then a fourth-year medical student) collected data during direct observation of 201 unselected consecutive consultations, by means of a pre-designed recording scheme – one for each patient. The consultations were carried out by four GPs, working in four group practices in different parts of Oslo. Two GPs were middle-aged female specialists in general practice, the other two were in their thirties and under GP specialization – one male and one female (see ). In addition to the recordings, 177 other unselected patients answered a brief questionnaire before entering a consultation with the same four GPs.
Table I. Characteristics of general practitioners (GPs) and data collection.
Outcome measures
All problems raised during a consultation were written down in simple terms by the observer, using the wording of the patient. A problem was defined as “any topic presented during the consultation, about which the GP gathered information and made a decision” [Citation5]. The definition also included problems regarding persons other than the patient during the encounter – the so-called secondary patient. We recorded whether the problem was dealt with during the consultation or postponed. The patient's age and sex were recorded, as well as whether the GP seen was the patient's regular GP. The problems recorded were subsequently categorized into the following eight groups by the first author [Citation5]: somatic problem, mental health problem, social problem, preventive measure, pregnancy care, administrative issue, problem related to a secondary patient, and other.
The questionnaires comprised the question: What is important for you when you see the GP? The following alternatives were given: (1) That I get an appointment within a short time span, for example within one week. (2) That I am able to address all the problems I have. (3) That I see my regular GP and not another GP in the practice. (4) Other (please describe). The importance of each alternative was rated on a five-point scale, from 1 = not important to 5 = very important.
Statistics
The data were transferred from the recording schemes and the questionnaires into SPSS by the first author. By means of SPSS™ version 22 (IBM Corp, Armonk, NY, USA), we carried out a t-test and analysis of variance (ANOVA), as well as regression analysis to test factors predictive of raising multiple problems. A p-value < 0.05 was considered statistically significant.
Ethics
The study was approved by the Regional Committee for Medical and Health Research Ethics (ref.2013/411). Each patient in the observation study received an information sheet and an agreement form from the receptionist when arriving at the practice. In the case where a patient refused to participate, the observer left the consultation room without meeting the patient. When the patient was < 16 years of age, the agreement form had to be signed by the accompanying parent. In the questionnaire sub-study, information was provided on top of the questionnaire sheet, and a filled-in questionnaire was considered an agreement to participation. The questionnaire was handed to the patient by the receptionist before the consultation, collected in a box, and finally delivered to the first author. No person-identifiable data were recorded on the questionnaire or on the recording scheme. In total, less than 10 patients declined to be observed, and none declined to fill in the questionnaire.
Results
Observation study
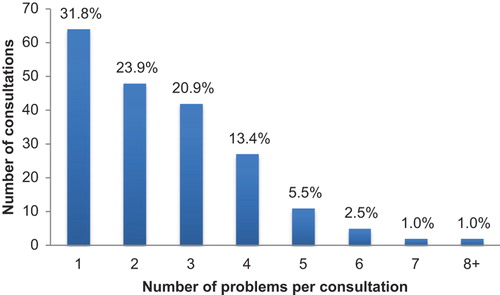
Characteristics of the four participating GPs and of the data collection are given in , and characteristics of the patients (n = 201) in . The mean number of problems presented during the consultations was 2.6 (range 1–16, ). Somatic problems were presented most frequently – they comprised almost half of all problems – followed by preventive measures and mental health problems (). In more than one-quarter (26.4 %) of consultations a mental health problem was presented, and in more than one-third (38.3 %) a preventive measure was addressed.
Table II. Characteristics of patients (n = 201) and of problems (n = 517) presented during unselected consultations in general practice.
More than three problems were presented in 23.4% of the consultations. In these consultations, 80.9% of patients were female, and mean age was 52.6 years. In the 10.0% of consultations where more than four problems were presented, 85.0% of patients were female and mean age was 55.3 years. Patients’ higher age and female sex independently predicted an increase in number of problems presented (). Patients younger than 50 years (69.7%) raised a mean of 2.3 problems per consultation, while those older than 50 years presented a mean of 3.3 problems. The 18.8% of patients older than 65 years presented 3.8 problems during their consultations. We did not find significant variation between genders in type of problems raised.
Table III. Effect of patients’ age and sex on number of problems (n = 517) presented in consultations (n = 201).
Close to 100% of patients presenting more than three problems were the GP's own list patients. Half of the problems presented by the GP were in the category preventive issues. The vast majority of the 517 problems presented during these 201 consultations were handled by the GP in the ongoing consultation.
In close to one-third of consultations, only one problem was presented. These consultations were mainly appointments made the same day for an acute condition. Patients presenting one problem were more frequently male (43.8%) compared with the total material (31.3 %), were 10 years younger (32.9 years) compared with the mean age of 42.4 years, and more frequently presented a somatic problem (65.5% versus 49.7% in the total material). In the remaining two-thirds of consultations – “ordinary consultations” – a mean of 3.3 problems were presented.
Questionnaire study
As shown in , the statement “That I am able to address all the problems I have” scored significantly higher, compared with the two other statements. Patients of GP 2 valued the importance of an appointment with own GP significantly higher, compared with GP 4's patients. Sixty patients provided a statement under “other”. The most frequent statements were: “to be taken seriously”, “to get enough time”, “competent doctor”, “friendliness” and “empathy”.
Table IV. Patients’ (n = 177) view on what is important in consultations in general practice.
Discussion
Main findings
This is probably the first Scandinavian study exposing GP consultations through direct observations, focusing on the problems presented by patients. The mean number of problems raised in these 201 consultations was 2.6 (range 1–16), and when appointments for acute conditions were excluded, the mean number was 3.3. Somatic problems comprised about half of all problems, but in more than one-quarter of consultations a mental health issue was presented. Female sex and increasing age predicted an increasing number of problems presented. The vast majority of problems were dealt with by the GP during the ongoing consultation. “That I am able to address all the problems I have” was rated as highly important by patients when seeing their GP.
Strengths and limitations
The main strength of our study is that data were collected by direct observation by one single person, who wrote down the patients’ requests in simple terms. The recording in unselected, consecutive consultations and the low number of patients refusing to participate also strengthen the internal validity of the study. There are, however, several limitations. Data were collected in only 201 consultations in four practices, so the study can be labelled exploratory. In order to obtain statistical power, for example to investigate possible variations between GPs, much larger samples would be needed – which in turn would require a different way of collecting data. The survey was carried out in the city of Oslo, and the results might well be different in rural parts of the country.
The presence of an observer in the consultation might influence the encounter, for example leading to avoidance of discussing sensitive issues [Citation10]. We tried to minimize this by placing the observer out of sight of the patient. The patients were not informed that the observer “counted” their requests; just that she observed what took place. The GPs, however, were informed about the hypothesis of the study, and we could speculate that this might make them more receptive towards the patients than usual. On the other hand, the GPs had to keep track of their ordinary schedule.
To decide whether a specific point made should be defined as a separate problem or as part of a problem that had already been recorded was not always easy. The observer was a medical student, inexperienced in carrying out consultations herself, while her supervisor – the second author – has long experience as a GP. The two authors discussed all unclear cases after the recording – and if still in doubt, they chose the label of one problem, not two. To label a certain complaint a somatic or a mental problem could sometimes be difficult. Any bodily symptom was defined as somatic, even if caused by health anxiety.
Comparison with earlier research
Our results correspond well with what has been found in earlier studies from the US and UK, where the mean number of problems raised in consultations was found to fall between 2.3 and 3.1 [Citation5–8]. The methods used for data collection in these studies vary from direct observation by students or research nurses [Citation5,Citation8] to video recording [Citation7] and questionnaires filled in by GPs [Citation6]. In another study based on direct observations and focusing on the effect of workload on consultations, the mean number of problems presented was 1.8 per consultation and slightly higher (1.9) for GPs with large patient lists [Citation11].
Our finding that increasing age was related to increasing number of problems raised is supported by some earlier studies. Beasley found that patients over 65 years of age raised a mean of 3.8 problems [Citation6], exactly the same number as in our study. In a study from the US focusing on time use for elderly patients and based on videotaping of consultations, Tai-Seal et al. found that a median of six topics were covered during a mean visit length of 15.7 minutes [Citation12]. In our study female patients presented significantly more problems than male patients. The studies of Beasley et al. [Citation6] as well as Salisbury et al. [Citation7] do not support this finding.
Our study showed some differences between the four participating GPS, as patients seeing GP 2 raised significantly more problems compared with patients seeing GP 4 – a mean of 2.9 versus 2.0. Patients seeing GP 4 were on average 10 years younger than patients seeing GP 2, which may be part of the explanation. However, GPs will probably have their own working style, which may limit or facilitate what a patient brings up. Patients have been found not to voice all their needs in consultations [Citation13], and we may well assume that patients behave as they believe they are expected to when facing a particular doctor. Our exploratory study was not powered to investigate variations between GPs, so these results should be interpreted with caution.
The 177 respondents in the questionnaire study valued being able to address all their problems in the consultation more highly than getting an appointment within a short time span and seeing their own GP at any appointment. Other studies have investigated this topic on a larger scale [Citation14–17]. Cheragi-Sohi et al. [Citation14] as well as Gerard et al. [Citation15] carried out discrete choice experiments, where patients valued certain aspects of the GP consultation. A study carried out in six general practices in UK revealed that patients evaluated a thorough physical examination highest, followed by being able to see a doctor who knew them well [Citation14]. Short waiting time for an appointment was not rated as highly important. Seeing a doctor of choice was the factor given the highest value in Gerard's study, higher than having a rapid appointment [Citation15]. “To be able to address all my problems” was not one of the options in these studies. Grol et al. investigated patients’ priority with regard to GP care among 3500 patients in eight different countries, among them Norway [Citation16]. “Getting enough time in consultations” was ranked top – above “feel free to talk about my problems”. Based on a systematic literature review of patients’ priorities for general practice including 19 papers, Wensing et al. found that “humaneness”, “competence/accuracy”, “patients’ involvement in decisions”, and “time for care” ranked top [Citation17].
We did not find any validated questionnaire short enough for our purpose, and thus designed the one we used. Based on the responses under “other” we would include the items “medically competent doctor” and “empathetic doctor” in future research.
Implications
General practice is probably the only health care setting where patients can freely address their worries and present multiple, unrelated, and often complex problems. Our study showed that patients valued highly being able to present all their problems, the vast majority of which were handled by the GPs during the ongoing consultation. To deal repeatedly with patients’ multiple questions within brief encounters and to translate them into medically sound actions is said to be the most complex intellectual exercise in clinical medicine [Citation18]. It involves a sense of timing, an ordering of priorities, and a clear understanding of the social context – and it takes years to master [Citation18]. This in turn has implications for medical education – both undergraduate and in particular for GPs’ vocational training. We need to direct more educational efforts to the issues of effective management of concurrent problems, in order to avoid doctors’ overload. And as populations age and patients in general practice become increasingly multi- morbid [Citation19,Citation20], we need to make sure GPs’ working conditions allow them to keep on mastering and even enjoying their daily “intellectual exercise” [Citation18]. In countries where consultations last only 10 minutes or less, GPs may find it particularly hard to deal with multiple problems. Signs reading “one problem for one consultation, please” show the challenges facing both patients and GPs [Citation20]. That a holistic and comprehensive view on patients remains a core value in general practice becomes only more important as the number of long-term conditions increases in the population.
Funding
There has been no external funding for this study.
Acknowledgements
Thanks are offered to Christian Bjørland for help with statistics and to Arne Fetveit for critically reviewing the manuscript.
Conflicts of interest
The authors report no conflicts of interest.
References
- Engel GL, Engel G. The need for a new medical model: A challenge for biomedicine. Science 1977;196:129–36.
- Borrell-Carrió F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: Principles, practice, and scientific inquiry. Fam Med 2004;2:576–82.
- Brown J, Stuart M, McCracken E, McWhinney I, Levenstein J. The patient-centred clinical method: Definition and application. Fam Pract 1986;3:75––9.
- Kirkengen AL, Ekeland TJ, Getz L, Hetlevik I, Ulvestad E, Vetlesen AJ. What constitutes competence? That depends on the task. Scand J Prim Health Care 2013;31:65–6.
- Flocke S, Frank SH, Wenger DA. Addressing multiple problems in the family practice office visit. J Fam Pract 2001;50: 211–16.
- Beasley JW, Hankey TH, Erickson R, Stange KC, Mundt M, Elliot M, et al. How many problems do family physicians manage at each encounter? A Wren Study. Ann Fam Med 2004;2:405–10.
- Salisbury C, Procter S, Stewart K, Bowen L, Purdy S, Ridd M, et al. The content of general practice consultations: Cross- sectional study based on video recordings. Br J Gen Pract 2013; 63:751–9.
- Stange KC, Zyzanski SJ, Jaén CR, Callahan EJ, Kelly RB, Gillanders WR, et al. Illuminating the “black box”: A description of 4454 patient visits to 138 family physicians. J Fam Pract 1998;46:377–89.
- Bindman AB, Forrest CB, Britt H, Crampton P, Majeed A. Diagnostic scope of and exposure to primary care physicians in Australia, New Zealand, and the United States: A cross-sectional analysis of results from three national surveys. BMJ doi:10.1136/bmj.39203.658970.55 (published 15 May 2007).
- Starfield B, D.S, Morris I, Bause G, Siebert S, Westin C. Presence of observers at patient–practitioner interactions: Impact on coordination of care and methodologic implications. Am J Public Health 1979;69:1021–6.
- Zyzanski SJ, Stange KC, Langa D, Flocke SA. Trade-offs in high-volume primary care practice. J Fam Pract 1998;46: 397–402.
- Tai-Seal M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res 2007;42: 1871–94.
- Barry CA, Bradley CP, Britten N, Stevenson FA, Barber N. Patients’ unvoiced agendas in general practice consultations: Qualitative study. BMJ 2000;320:1246–50.
- Cheraghi-Sohi S, Hole AR, Mead N, McDonald R, Whalley D, Bower P, Roland M. What patients want from primary care consultations: A discrete choice experiment to identify patients’ priorities. Ann Fam Med 2008;6:107–15.
- Gerard K, Salisbury C, Street D, Pope C, Baxter H. Is fast access to general practice all that should matter? A discrete choice experiment of patients’ preferences. J Health Serv Res Policy 2008;13(Suppl 2):3–10.
- Grol R, Wensing M, Mainz J, Ferreira P, Hearnshaw H, Hjortdahl P, et al. Patients’ priorities with respect to general practice care: An international comparison. European Task Force on Patient Evaluations of General Practice (EUROPEP). Fam Pract 1999;16:4–11.
- Wensing M, Jung HP, Mainz J, Olesen F, Grol R. A systematic review of the literature on patient priorities for general practice care, Part 1: Description of the research domain. Soc Sci Med 1998;47:1573–88.
- Loxtercamp D. What a doctor is good for. BMJ 2014;349: g6894.
- Salisbury C, Johnson L, Purdy S, Valderas JM, Montgomery AA. Epidemiology and impact of multimorbidity in primary care: A retrospective cohort study. Br J Gen Pract 2011;61:e1221. DOI:10.3399/bjgp11X548929.
- Hobbs FDR, Baker M, Davies SC. Morbidity matters: Challenge for research (Editorial). Brit J Gen Pract 2015;65: e215–16. DOI:10.3399/bjgp15X684301.