Abstract
Objective is to explore how multimorbidity is defined in the scientific literature, with a focus on the roles of diseases, risk factors, and symptoms in the definitions. Design: Systematic review. Methods: MEDLINE (PubMed), Embase, and The Cochrane Library were searched for relevant publications up until October 2013. One author extracted the information. Ambiguities were resolved, and consensus reached with one co-author. Outcome measures were: cut-off point for the number of conditions included in the definitions of multimorbidity; setting; data sources; number, kind, duration, and severity of diagnoses, risk factors, and symptoms. We reviewed 163 articles. In 61 articles (37%), the cut-off point for multimorbidity was two or more conditions (diseases, risk factors, or symptoms). The most frequently used setting was the general population (68 articles, 42%), and primary care (41 articles, 25%). Sources of data were primarily self-reports (56 articles, 42%). Out of the 163 articles selected, 115 had individually constructed multimorbidity definitions, and in these articles diseases occurred in all definitions, with diabetes as the most frequent. Risk factors occurred in 98 (85%) and symptoms in 71 (62%) of the definitions. The severity of conditions was used in 26 (23%) of the definitions, but in different ways. The definition of multimorbidity is heterogeneous and risk factors are more often included than symptoms. The severity of conditions is seldom included. Since the number of people living with multimorbidity is increasing there is a need to develop a concept of multimorbidity that is more useful in daily clinical work.
The increasing number of multimorbidity patients challenges the healthcare system. The concept of multimorbidity needs further discussion in order to be implemented in daily clinical practice.
Many definitions of multimorbidity exist and most often a cut-off point of two or more is applied to a range of 4–147 different conditions.
Diseases are included in all definitions of multimorbidity.
Risk factors are often included in existing definitions, whereas symptoms and the severity of the conditions are less frequently included.
Key Points
Introduction
The occurrence of multimorbidity (MM), which can be defined as the co-existence in one patient of two or more concurrent chronic conditions (e.g., diseases, risk factors, or symptoms) is increasing.[Citation1,Citation2]. Even though the prevalence increases with age, the majority of patients suffering from MM are of working age.[Citation3] For society, MM results in increased costs and more frequent hospital admissions.[Citation4] For the individual, mortality increases [Citation5] and quality of life decreases with the number of conditions.[Citation6]
Definitions of MM are wide-ranging with conditions varying in number, kind, and severity. Sources of data and settings around the definitions are diverse, and sometimes social aspects or mental health are included in the definition.[Citation7–9] The definition of MM is mainly based on diseases.[Citation9] In general, a disease is an entity based on either symptoms and/or objective measures. A disease is often labelled with a diagnosis, and the diagnosis serves as a tool for health professionals to communicate and find optimal treatments and solutions for medical problems.[Citation10,Citation11] Risk factors for developing disease, however, are also often treated as diseases, as the purpose of paying attention to a risk factor is to create the basis for actions from the patient and the doctor to prevent disease.[Citation12,Citation13] Symptoms may be defined as “any expression of disturbed function or structure of the body and mind by a patient”,[Citation14] and the patient’s interpretation of the intensity and the presumed danger of symptoms is central to decisions about if and when a doctor is consulted.[Citation15,Citation16] Diseases and risk factors can sometimes be less meaningful to patients since they do not always explain co-occurring symptoms.[Citation17] Furthermore, a diagnosis, whether it comes from a disease or a risk factor, can lower self-rated health [Citation18] and the relevance of becoming labelled with MM when only suffering from risk factors is questionable. On the other hand, symptoms cannot always be explained and can contain more dimensions of the human mind than strictly medical.[Citation19] This means that substantially different aspects of health are included in definitions of MM. Existing MM definitions may seem more suitable for epidemiological research than for clinical work. In the light of the increasing prevalence and burden of MM, definitions which are more useful in daily practical work could be more helpful for both clinicians and patients.
The aim of this study was to review the literature on MM in order to examine how it is defined: What diseases, risk factors, and symptoms are included in the definition? Are the duration and severity of conditions considered? Are complications to a disease included together with this disease in the definition of MM or are they included as separate disease categories, e.g., retinopathies in the course of diabetes? Is clustering considered, e.g., the likelihood of conditions to appear together?
Methods
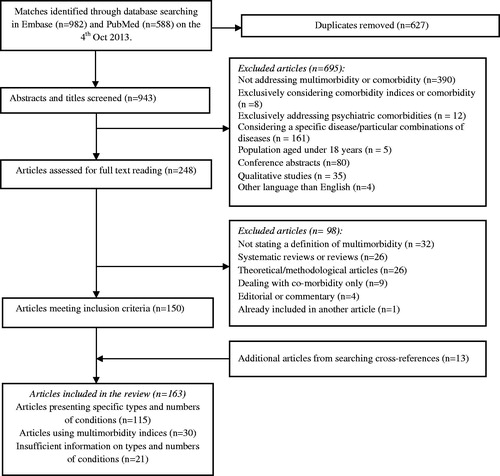
The review process was conducted according to PRISMA guidelines.[Citation20]
Search strategy
A literature review was conducted in MEDLINE (PubMed) and Embase. The databases were searched up until 4 October 2013 (protocol can be forwarded on request). We applied the search string with different linguistic variations of the terms multimorbidity and comorbidity, and also with related synonyms, in order to increase sensitivity, i.e., the chance of finding articles considering MM without using the term itself. Since the word “multimorbidity” does not exist as a MeSH-term (Medical Subject Heading) in MEDLINE, we searched for it as a keyword. We searched for comorbidity both as a MeSH-term and as a keyword. The search was restricted to research on humans, in the English language, and articles with available abstracts. In addition, the same search was performed in The Cochrane Library up until 10 October 2013, but without restrictions. After exclusion of irrelevant references and removal of duplicates, no references remained from The Cochrane Library. One author (TGW) performed and conducted the search. For the search in MEDLINE ().
Box 1. Results of search strategy in MEDLINE.
Selection of studies
After removal of duplicates, one author (TGW) screened all titles and abstracts for relevance. The eligibility of potentially relevant articles was assessed in full text (by TGW). For inclusion in the final synthesis, the articles had to be empirical and contain a definition of MM. Systematic reviews and theoretical articles were excluded because they mainly summarized the work of others without creating their own definitions (). Since the aim of this study was to describe how MM is defined, we did not assess the quality of the articles included. Reference lists for all eligible articles and the systematic reviews that were excluded were searched by title for further articles. The first author (TGW) extracted data items into a pre-specified table. The following items were extracted: cut-off point in the number of conditions in the definition of MM, population size, setting, sources of data, the number and kind of conditions included, risk factors, symptoms, complications, duration of the conditions, considerations of clustering between conditions, and finally considerations about and measurement of the severity of conditions included. (The full document and the references of all 163 articles included in our study are available as an electronic appendix 1 and 2 at http://almenpraksis.ku.dk/english/research/appendix_1.pdf/ and at http://almenpraksis.ku.dk/english/research/appendix_2.pdf/ Ambiguous findings that emerged after titles and abstracts were screened, and then read in full text, were discussed and resolved with one of the co-authors (NdFO).
Definition of diseases, risk factors and symptoms
Diseases were defined based on the assumption that they were health conditions diagnosed by objective measures, symptoms or both, and that a distinct diagnostic code exists to describe them. Risk factors were defined as conditions or measurements associated with the probability of disease or death [Citation21,Citation22] not necessarily recognised by the patient. Symptoms were defined by using ICPC’s definition of symptoms.[Citation23]
Results
Of 248 articles screened, we included 163 in our study (). The majority of these articles were observational and only three were randomized controlled trials.
Definition of MM, population size, setting, and data sources
Of the 163 articles we selected, 61 (37%) used a cut-off point of two or more conditions in their definition of MM (i.e., diseases, risk factors, and symptoms); four (2%) used a cut-off point of one condition, and 11 (7%) used a cut-off point of three conditions. Thirteen articles (8%) had several cut-off points, 19 (12%) used different MM-indices without a specific cut-off, while 55 (34%) did not specify cut-offs at all.
The population size varied considerably in the selected articles. Twenty-four articles (15%) had >100.000 participants and 48 (29%) had <1000 participants, with a range from 38 patients in the smallest to approximately 31 million in the largest. Participants were mainly recruited from the general population (68 articles, 42%), while many came from primary care (41 articles, 25%), and some from secondary care (16 articles, 10%). In one article, participants were recruited from a nursing home,[Citation24] and in 26 articles (16%) they came from specific databases, for example veterans,[Citation25] twins,[Citation26] or employees.[Citation27] Eleven articles (7%) included people from several settings simultaneously. Data were from self-reports (56 articles, 34%), registries (36 articles, 22%), medical records (22 articles, 13%), clinical examinations (3 articles, 2%), and medication data (2 articles, 1%). Finally, 44 articles (27%) had data from several sources concurrently.
Of the 163 articles included in our study, 115 (71%) used individually constructed definitions of MM and only a handful of the articles used an existing definition. The results of the 115 articles are presented below. Thirty articles (18%) defined MM using either existing morbidity indices, which were not originally designed to rate MM, or a clinical database of ICPC codes (see below). Three articles were included in two categories: as an individually developed definition and as an index. These articles used an index but explicitly selected some of the conditions from the index in question, indicating a process of reflection when defining MM (see electronic appendix 1). Finally, 21 articles (13%) presented insufficient information about types of conditions, or did not select the conditions in advance, and they are not reported upon here.
In the 115 articles that used individually constructed definitions of MM, the pool of conditions to choose from varied from 4 [Citation28] to 147.[Citation29] The conditions included were primarily chronic as defined by WHO: “health problems that require on-going management over a period of years or decades”.[Citation30] Other definitions were also used, e.g., if the condition was presumed permanent or caused by pathological alterations without chance of reversibility.[Citation31]
Diseases
All 115 articles reported information on diseases. Some included clear diagnostic entities such as myocardial infarction,[Citation32] while others included broader diagnostic groups like heart disease.[Citation33] Diabetes, stroke, and cancer were the most frequently occurring diseases (). Fibromyalgia, sexually transmitted diseases, parasites, and infections were the least frequently occurring diseases.
Table 1. Most prevalent diseases, risk factors and symptoms in the definition of multimorbidity in the 115 articles.
Risk factors
Ninety eight articles (85%) included one or more of the following risk factors: hypertension, osteoporosis, hypercholesterolemia, obesity, and overweight (). Risk factors were included in the definitions in the same way as diseases with one risk factor representing one condition.
Symptoms
Seventy one articles (62%) reported information on symptoms. As for diseases and risk factors, one symptom represented one condition. The most frequently occurring symptom was back pain, followed by visual impairment, and urinary incontinence (). Several symptoms occurred in only one definition, e.g., itching, nausea, dysphagia, diarrhea and abdominal pain.
The role of duration, severity, clustering of conditions, and occurrence of complications
The duration of a condition was explicitly mentioned and specified as an inclusion criterion for the definition of MM in 32 of the 115 articles (28%). However, when used, duration was operationalized in many different ways by, for instance, including only conditions present during the last year, or using more specific time limits for certain conditions, such as excluding cancer diagnosed more than 5 years before the study (). Severity was included to some extent in 26 of the articles (23%). It varied from patients’ self-reported severity of a condition, to only including diseases with defined severity stages, e.g., heart failure with at least NYHA II (New York Heart Association functional classification, stage 2). Considerations on how conditions are clustered in the individually constructed MM definitions were only apparent in a few articles. These mainly described conditions within different organ groups, or they grouped conditions with the same pathophysiological mechanisms. However, considerations of clustering did not influence the results since most of the conditions were not reported upon as a group but as separate diagnoses. Complications were in general not stated as such even though, for example, renal failure that could be considered a complication of diabetes was included in some definitions of MM. Therefore, information on clustering and complications could not be summarised.
Table 2. Every aspect of duration mentioned in the 115 articles.
Multimorbidity indices
Almost all indices include diseases. The Adjusted Clinical Groups (ACG) Case Mix System and its subgroups, Aggregated Diagnosis Groups (ADG), Medication-based Rx-MG, Expanded Diagnosis Clusters (EDC), and Resource Utilization Bands (RUB) almost all contain information on both risk factors and symptoms. Severity is also included in most ACG subgroups (). For Clinical Classifications Software (CCS), risk factors and symptoms are included in the index, but not severity. The Cumulative Illness Rating Scale (CIRS), which includes diseases from 13 different organ systems, does not specify whether risk factors or symptoms are included but it places severity at the centre of the index (with rating of every condition on a four grade scale). Charlson Comorbidity Index (CCI) includes some symptoms and rates severity to some extent, but contains no risk factors. Systems such as the Quality and Outcomes Framework (QoF) and The Functional Comorbidity Index (FCI) include risk factors and symptoms but do not consider their severity. The Index of Coexistent Disease (ICED), on the other hand, contains both risk factors and severity, but has no symptoms. Finally a Dutch database, The Registration Network Family Practices (RNH) includes risk factors, but neither symptoms nor severity. Some articles that used an index did not explicitly mention if they used all conditions included in the index or just a selection.
Table 3. Multimorbidity indices and databases used in 30 articles out of the total of 163 articles.
Discussion
We found great heterogeneity in the definition of MM and the pool of conditions to choose from varied from 4 to 147. Most often a cut-off point of two or more conditions was used to define MM. Diseases were used in all definitions, and the most common were diabetes, stroke, cancer, ischaemic heart disease, and COPD (). Risk factors were included in 85% of the individually developed definitions of MM and in all indices except CCI. Two further indices gave inadequate information (). Hypertension was the most frequent risk factor and was included to the same degree as a cancer diagnosis in MM definitions. Other risk factor-based conditions were osteoporosis, hypercholesterolemia, obesity, and overweight (). Symptoms were included in 62% of the articles with great diversity regarding the types of symptoms. The most frequent symptoms were back pain, visual impairment, urinary incontinence, alcohol disorder, and hearing impairment (). Duration was mentioned in 28% of the articles () and, to some extent, the severity of conditions was included in 23% of the articles.
The role of diseases
Diseases are included in all definitions of MM. However, they do not always explain the patient’s experience of symptoms, and patient needs and symptom experience are not necessarily an indication of an underlying disease. Relying only on diseases when defining MM may lead to a concept that does not reflect patients’ perspectives. Previously, diabetes has been found to be the most frequent disease in the definition of MM, followed by stroke, cardiovascular disease, hypertension, and cancer.[Citation9] We identified a similar pattern, even though we found that cancer was used more often than cardiovascular disease. This could be due to different ways of defining cardiovascular disease.
The role of risk factors
Risk factors, based on objective rather than subjective measures, are easy to quantify [Citation34] and therefore easy to use in epidemiological research. Hypertension and hyperlipidaemia were observed as the most prevalent conditions in a population study that included almost 31 million Americans.[Citation35] Similarly, in other studies in different settings and countries, hypertension is reported as the most prevalent chronic condition.[Citation36,Citation37] We found this mirrored in the definitions of MM as well. One systematic review found that prevalence was the main reason for including conditions in MM.[Citation9] Nevertheless, conditions that are common in the population, like allergies and hypertension, are not necessarily those with the largest impact on patients’ functional status or quality of life.[Citation38] Furthermore, the burden of illness reported by patients is lower among those having hypertension compared to patients with other conditions.[Citation37] If relying too much on risk factors when defining MM, the MM measure will probably become too coloured by aspects concerning awareness of future illness, rather than the actual disease burden or functional status.
The role of symptoms
Symptoms are generally the focus of patients’ concerns and are dependent on the experiences and history of the patient and often the reason for contacting a doctor. For the doctor, the symptom and what the patient presents are central for the diagnostic process and the doctor grades according to importance and frames what the patient says.[Citation39] Headache and back pain seem to be the most debilitating symptoms among people who report poor self-rated health,[Citation40] and back pain is reported as among the most prevalent conditions in all age groups.[Citation41] Furthermore, symptoms are an important factor for mortality in line with diseases.[Citation42] In this review, we found that symptoms occur less frequently in the definition of MM than risk factors.
Relation to other studies
Since useful clinical guidelines for patients with MM are scarce it was expected [Citation43] that only a minority of the articles found in the literature search were randomized controlled trials. Furthermore, randomized controlled trials involving primary care patients rarely report whether patients with coexisting conditions are excluded or not, and if they are included only few conditions are considered.[Citation44] Pharmaceutical trials often have many exclusion criteria for chronic conditions compared to observational studies.
The considerable variability in the prevalence of MM between studies may have several explanations. First, the setting is important. MM is obviously very common in nursing homes, and patients recruited in family practice are more likely to have more conditions compared to those recruited in the general population.[Citation45] Second, MM increases with the range of conditions included in the definition.[Citation8] Third, the longer the observation period, the more conditions and clusters of diagnoses are captured.[Citation46] Fourth, sources of data can affect prevalence. Prevalence is higher when more conditions are considered or when the cut-off of two or more conditions is used instead of a higher cut-off. Furthermore, the prevalence of MM rises when conditions are counted as single diseases with a unique diagnosis code instead of being included in the group of codes (often organ system) the condition belongs to.[Citation47] On the other hand, complexity of the conditions and also health care use are dependent on if conditions are concordant or discordant, i.e. have the same pathophysiology with equal management or not [Citation48] and conditions that cluster tend to be more concordant.
Within the last 5 years, there have been several systematic reviews on MM. Their focus has varied from occurrence, patterns, and consequences of MM,[Citation8,Citation49,Citation50] to interventions,[Citation51] functional status,[Citation52] self-management,[Citation53] and implementation of care programs.[Citation54] One review focused on measures of disease burden and found indices like CCI, CIRS, and ACG System useful depending on the outcome of interest.[Citation55] We found 30 articles that used indices for measuring MM. Indices of MM may be better than simple counts of conditions to detect certain circumstances that are important for the patient, such as psychological distress.[Citation56] This is because some indices allow important information from the text of the medical record to be included with diseases. However, prevalence estimates using either chapters in ICPC, ICD-10, or CIRS have shown to be comparable.[Citation47]
To the best of our knowledge, only two reviews have studied the definition of MM until now. In 2009, Diederichs et al. collected information on the number and type of conditions from 39 selected articles.[Citation9] As in the present review, they found great heterogeneity between studies in the type of conditions that could account for MM and they highlighted the need for a uniform way to estimate MM. In 2013, Le Reste et al. suggested a comprehensive definition of MM specifically suited to primary care. Based on a selection of 54 qualitative articles, they concluded: “MM is defined as any combination of chronic disease with at least one other disease (acute or chronic) or biopsychosocial factor (associated or not) or somatic risk factor”. In accordance with our findings, all definitions of MM contained several chronic diseases. Thus, while it seems meaningful to include at least one chronic condition as Le Reste et al. suggest, we found that acute conditions are very rarely included. In some specialties one chronic condition could be meaningful in the co-occurrence of an extra acute condition, e.g., diabetes in a surgical patient. However, for general practice where the acute complaints can be less severe the importance of this way of defining MM can be less clear, especially if we will use MM prevalence to plan healthcare.[Citation47] Including biopsychosocial factors opens up the possibility of including symptoms, which is one way of integrating patient perspectives in MM-definitions, as long as a symptom is not classified as a chronic condition and already included. Thus, Le Reste et al. consider disease burden, risk factors, social network etc. to be modifiers of the effects of MM [Citation7] and their definition may better reflect daily clinical work in general practice in comparison with counting diseases. By including the disease burden, they also consider the severity of the conditions, which we found included in only a quarter of the articles we selected. While we found risk factors to be one of the most important features of the MM definition to date, Le Reste et al. maintain that risk factors only contribute to the definition of MM when they occur in combination with other chronic conditions, implying that risk factors alone cannot lead to MM. Further, Le Reste et al. include social networks as modifiers which seems meaningful since the contextual factors surrounding a patient are sometimes as important as a disease.[Citation57] However, operationalization of social factors is difficult. While patients can have a large social network, support from it can be of low quality, and religious beliefs or cultural traditions can give patients obligations that are difficult to capture in a definition. Furthermore, the point in time to concentrate on a problem can be more important than the diagnosis itself. For example, a diagnosis made 5 years ago is often not the focus of concern any more.[Citation58]
Limitations and strengths
The objective of this study was to shed light on the diversity of definitions of MM. It is possible, however, that our search strategy has overlooked important articles having a unique definition, and in this context the lack of a MeSH-term for MM was a limitation. We compensated for this by choosing a broad search strategy with several linguistic variations of MM to increase sensitivity. Furthermore, there was only one reader making the selection of articles, but even minor inconsistencies were settled in consensus between two authors. We could have included languages other than English in our study, but a substantial number of the selected articles came from authors whose mother tongue is not English. Therefore, we believe our findings are not restricted to English-speaking countries. A major strength of the current review is the thorough systematic work in accordance with PRISMA-guidelines. We therefore expect that most of the existing definitions of MM were detected and included.
Clinical implications
The increase in MM is consistent between countries and one study examining the development of MM over the last 20 years found the largest increase in MM prevalence for those with four or more conditions.[Citation2] MM accounts for many consultations in primary care. The number of conditions is associated with the number of consultations [Citation4] and is inversely associated with continuity of care.[Citation59] Furthermore, when defining MM as two or more conditions almost half of the patients in primary care are multimorbid [Citation47] and this will become even more pronounced in the future. However, counting diseases and mapping patterns are maybe of less relevance compared to the disability connected with and the severity of the conditions,[Citation52] also because interventions for MM have shown to be most effective when focusing on functional difficulties rather than the individual diseases.[Citation51] There is a need to discuss definitions of MM that are more relevant for daily clinical work with patients, and that have a better capability of capturing the patient’s perspective. These definitions can help us identify MM where it is imperative to treat, and MM where the best solution may be not to treat. Based on qualitative data, Le Reste et al. [Citation7] have given the most inspiring and comprehensive definition of MM so far, one that is particularly suited to primary care. Since this review has explored the role of symptoms and risk factors in the definition of MM, it can make a valid contribution to the discussion of future definitions of MM.
Conclusion
In line with earlier research, this review of 163 articles shows a large variation in the number and types of conditions that are included in the definition of MM, which consist mainly of diseases. The fundamental role of risk factors in the definition of MM is one reason for the high prevalence of MM. Symptoms and severity are included less often and this contributes to making the existing definitions more usable for epidemiologists than for clinicians and patients. This review adds to the discussion about more comprehensive and clinically relevant MM definitions.
Funding information
This study was supported by the Danish Research Fund for General Practice.
Disclosure statement
The authors report no conflicts of interest.
References
- van der Akker M BF, Knottnerus JA. Comorbidity or multimorbidity: what's in a name? A review of literture. Eur J Gen Pract. 1996;2:65–70.
- Uijen AA, van de Lisdonk EH. Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. 2008;14:28–32.
- Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43.
- Glynn LG, Valderas JM, Healy P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. FamPract. 2011;28:516–523.
- France EF, Wyke S, Gunn JM, et al. Multimorbidity in primary care: a systematic review of prospective cohort studies. BrJ Gen Pract. 2012;62:e297–e307.
- Fortin M, Lapointe L, Hudon C, et al. Multimorbidity and quality of life in primary care: a systematic review. Health Qual Life Outcomes. 2004;2:51.
- Le Reste JY, Nabbe P, Manceau B, et al. The European general practice research network presents a comprehensive definition of multimorbidity in family medicine and long term care, following a systematic review of relevant literature. J Am Med Direct Assoc. 2013;14:319–325.
- Fortin M, Stewart M, Poitras ME, et al. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012;10:142–151.
- Diederichs C, Berger K, Bartels DB. The measurement of multiple chronic diseases – a systematic review on existing multimorbidity indices. J Gerontol A Biol Sci Med Sci. 2011;66:301–311.
- Malterud K. Diagnosis – a tool for rational action? A critical view from family medicine. Atrium. 2013;11:26–31.
- Undeland M, Malterud K. Diagnostic work in general practice: more than naming a disease. Scand J Prima Health Care. 2002;20:145–150.
- Hollnagel H, Malterud K. From risk factors to health resources in medical practice. Med Health Care Phil. 2000;3:257–264.
- Reventlow S. Risikoopfattelse og osteoporose hos kvinder i alderen 60-70 år. En kvalitativ undersøgelse af risikooplevelse, kulturelle forestillinger og kropslige oplevelser og kropspraksis. [Doctoral Disputats]. Københavns Universitet; 2008.
- Bentzen N, Bridges-Webb C. An international glossary for general/family practice. Fam Pract. 1995;12:341-369.
- Macleod U, Mitchell ED, Burgess C, et al. Risk factors for delayed presentation and referral of symptomatic cancer: evidence for common cancers. Br J Cancer. 2009;101:S92–S101.
- Kroenke K, Harris L. Symptoms research: a fertile field. Ann Intern Med. 2001;134:801–802.
- Undeland M, Malterud K. The fibromyalgia diagnosis: hardly helpful for the patients? A qualitative focus group study. Scand J Prim Health Care. 2007;25:250–255.
- Jorgensen P, Langhammer A, Krokstad S, et al. Diagnostic labelling influences self-rated health. A prospective cohort study: the HUNT study, Norway. Fam Pract. 2015;32:492–499.
- Eriksen TE, Risor MB. What is called symptom? Med Health Care Phil. 2014;17:89–102.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clin Res Ed). 2009;339:b2700.
- Nexoe J, Halvorsen PA, Kristiansen IS. Critiques of the risk concept – valid or not? Scand J Public Health. 2007;35:648–654.
- Reventlow S, Hvas AC, Tulinius C. “In really great danger…” The concept of risk in general practice. Scand J Prim Health Care. 2001;19:71–75.
- WHO. International Classification of Primary Care, Second edition (ICPC-2); [cited 2015 19 May]. Available from: http://www.who.int/classifications/icd/adaptations/icpc2/en/.
- Akner G. Analysis of multimorbidity in individual elderly nursing home residents. Development of a multimorbidity matrix. Arch Gerontol Geriatr. 2009;49:413–419.
- Steinman MA, Lee SJ, John BW, et al. Patterns of multimorbidity in elderly veterans. J Am Geriatr Soc. 2012;60:1872–1880.
- Caracciolo B, Gatz M, Xu W, et al. Relationship of subjective cognitive impairment and cognitive impairment no dementia to chronic disease and multimorbidity in a nation-wide twin study. J Alzheimer's Dis. 2013;36:275–284.
- Holden L, Scuffham PA, Hilton MF, et al. Patterns of multimorbidity in working Australians. Popul Health Metrics. 2011;9:15.
- Findley P, Shen C, Sambamoorthi U. Multimorbidity and persistent depression among veterans with diabetes, heart disease, and hypertension. Health Soc Work. 2011;36(2):109–119.
- Rizza A, Kaplan V, Senn O, et al. Age- and gender-related prevalence of multimorbidity in primary care: the Swiss FIRE project. BMC Fam Pract. 2012;24:113.
- WHO. Innovative care for chronic conditions: building blocks for action: global report. Geneva, Switzerland: WHO; 2002.
- Formiga F, Ferrer A, Sanz H, et al. Patterns of comorbidity and multimorbidity in the oldest old: the Octabaix study. Eur J Intern Med. 2013;24:40–44.
- Drewes YM, den Elzen WP, Mooijaart SP, et al. The effect of cognitive impairment on the predictive value of multimorbidity for the increase in disability in the oldest old: the Leiden 85-plus Study. Age Ageing. 2011;40:352–357.
- Andrade LH, Bensenor IM, Viana MC, et al. Clustering of psychiatric and somatic illnesses in the general population: multimorbidity and socioeconomic correlates. Braz J Med Biol Res. 2010;43:483–491.
- Hacking I. Making up people: clinical classifications. Lond Rev Books. 2006;28:23–26.
- Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83.
- Schram MT, Frijters D, van de Lisdonk EH, et al. Setting and registry characteristics affect the prevalence and nature of multimorbidity in the elderly. J Clin Epidemiol. 2008;61:1104–1112.
- Burgers JS, Voerman GE, Grol R, et al. Quality and coordination of care for patients with multiple conditions: results from an international survey of patient experience. Eval Health Prof. 2010;33:343–364.
- Perruccio AV, Power JD, Badley EM. The relative impact of 13 chronic conditions across three different outcomes. J Epidemiol Community Health. 2007;61:1056–1061.
- Malterud K, Guassora AD, Graungaard AH, et al. Understanding medical symptoms: a conceptual review and analysis. Theoret Med Bbioethics. 2015;36:411–424.
- Vos HMM, Bor HH, Rangelrooij-Minkels MJAV, et al. Multimorbidity in older women: the negative impact of specific combinations of chronic conditions on self-rated health. Eur J Gen Pract. 2013;19:117–122.
- Fuchs J, Busch M, Lange C, et al. Prevalence and patterns of morbidity among adults in Germany. Results of the German telephone health interview survey German Health Update (GEDA) 2009. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2012;55:576–586.
- Stalbrand IS, Svensson T, Elmstahl S, et al. Subjective health and illness, coping and life satisfaction in an 80-year-old Swedish population-implications for mortality. Int J Behav Med. 2007;14:173–180.
- Fortin M, Contant E, Savard C, et al. Canadian guidelines for clinical practice: an analysis of their quality and relevance to the care of adults with comorbidity. BMC Fam Pract. 2011;12:74.
- Fortin M, Dionne J, Pinho G, et al. Randomized controlled trials: do they have external validity for patients with multiple comorbidities? Ann Fam Med. 2006;4:104–108.
- Fortin M, Hudon C, Haggerty J, et al. Prevalence estimates of multimorbidity: a comparative study of two sources. BMC Health Serv Res. 2010;6:111.
- Wong A, Boshuizen HC, Schellevis FG, et al. Longitudinal administrative data can be used to examine multimorbidity, provided false discoveries are controlled for. J Clin Epidemiol. 2011;64:1109–1117.
- Harrison C, Britt H, Miller G, et al. Examining different measures of multimorbidity, using a large prospective cross-sectional study in Australian general practice. BMJ Open. 2014;4:e004694.
- Calderon-Larranaga A, Abad-Diez JM, Gimeno-Feliu LA, et al. Global health care use by patients with type-2 diabetes: does the type of comorbidity matter? Eur J Intern Med. 2015;26:203–210.
- Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10:430–439.
- Prados-Torres A, Calderon-Larranaga A, Hancco-Saavedra J, et al. Multimorbidity patterns: a systematic review. J Clin Epidemiol. 2014;67:254–266.
- Smith SM, Soubhi H, Fortin M, et al. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev (Online). 2012;18:CD006560.
- Ryan A, Wallace E, O'Hara P, et al. Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes. 2015;13:168.
- Liddy C, Blazkho V, Mill K. Challenges of self-management when living with multiple chronic conditions: systematic review of the qualitative literature. Can Fam Physician. 2014;60:1123–1133.
- de Bruin SR, Versnel N, Lemmens LC, et al. Comprehensive care programs for patients with multiple chronic conditions: a systematic literature review. Health Policy. 2012;107:108–145.
- Huntley AL, Johnson R, Purdy S, et al. Measures of multimorbidity and morbidity burden for use in primary care and community settings: a systematic review and guide. Ann Fam Med. 2012;10:134–141.
- Fortin M, Bravo G, Hudon C, et al. Psychological distress and multimorbidity in primary care. Ann Fam Med. 2006;4:417–422.
- Shippee ND, Shah ND, May CR, et al. Cumulative complexity: a functional, patient-centered model of patient complexity can improve research and practice. J Clin Epidemiol. 2012;65:1041–1051.
- Valderas JM, Starfield B, Sibbald B, et al. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7:357–363.
- Salisbury C, Johnson L, Purdy S, et al. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2011;61:e12–e21.