To the Editor,
A 42-year-old Caucasian woman presented with a six month history of inter-scapular pain. Imaging at her local hospital demonstrated a lesion in the left upper lobe and another in the left base of her lung. Two pleurally based masses were removed and the left lower lobe was resected due to infiltration by tumour. She was referred to the Royal Marsden Sarcoma Unit, as histopathological review of the surgical tissue had revealed synovial sarcoma. A repeat CT scan performed two months following surgery demonstrated a soft tissue mass in the posterior chest wall in the paravertebral area as well as soft tissue thickening in the posterior mediastinum.
She was treated with six cycles of combination doxorubicin (20mg/m2 over 3 days) and ifosfamide (3000mg/m2 over 3 days), and achieved a good partial response, followed by consolidation radiotherapy to the right chest wall (60 Gy in 30 fractions).
Fifteen months later she underwent surgical resection of both recurrent masses and also a metastasis in the left lower lobe parenchyma. The resection margin along the vertebrae was involved on histological examination. A further resection of the vertebral body was subsequently performed. An asymptomatic new metastasis in the right lung was detected five months post spinal surgery. A subsequent interval scan demonstrated multiple lesions in the right lung. Consequently, she was commenced on ifosfamide (3000 mg/m2 over 3 days), to progressive disease after three cycles.
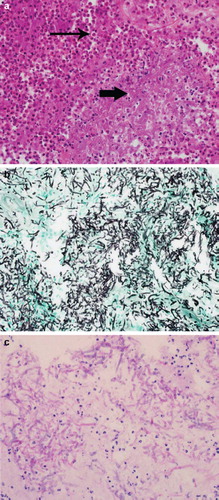
Approximately 12 months later she was admitted with spinal cord compression at T9 () and was treated with dexamethasone and radiotherapy (24 Gy in 6 fractions) and made a good symptomatic recovery. For her progressive pulmonary disease she was re-challenged with doxorubicin (50 mg/m2) with dexrazoxane (1000 mg/m2) cover. Following one cycle she was admitted with neutropenic sepsis and also developed a pathological fracture of the T9 vertebrae. Surgical decompression and posterior fusion was performed. Pathological review demonstrated fungal infection with a large cluster of fungal hyphae (thick arrow in ) and abundant polymorphs (thin arrow in ) signifying extensive acute inflammation, but no evidence of synovial sarcoma. The fungal hyphae are more clearly seen with the Grocott-methenamine silver stain, shown in black () and the Periodic acid Schiff stain (PAS) which highlights fungal cell walls magenta/red (). She was treated with voriconazole 200 mg bid, initially given intravenously for three weeks followed by maintenance 200 mg bid orally.
Figure 2. 2a. Haematoxyllin and eosin stain (large cluster of fungal hyphae shown by thick arrow) 2b. Grocott-methenamine silver stain (fungal hyphae seen in black) 2c. Periodic acid Schiff stain.
She subsequently received a second cycle of doxorubicin, but required revision of the spinal rods. A re-staging scan at that time demonstrated progressive disease. She was re-commenced on doxorubicin and received a further three cycles, but had progressive disease. The patient passed away peacefully five years after her original diagnosis.
Fungal infection is a rare cause of osteomyelitis accounting for 2–4% of cases [Citation1] and was first described by Keating in 1932 [Citation2]. Most fungal infections are isolated in the lungs due to inhalation of exogenous spores. The development of bony fungal lesions occurs as a result of haematogenous disseminated infection, and usually present with several foci of infection in the body. Spinal involvement is rare, with the medical literature confined to case reports [Citation3]. Clinical presentation of fungal vertebral osteomyelitis can include back pain, fever, malaise or night sweats and rarely with neurological symptoms, including spinal cord compression. The diagnosis can be difficult in a patient with widespread malignant disease, as the most likely differential is bony metastatic disease. Treatment of fungal vertebral osteomyelitis includes the use of antifungal agents, and surgery if there is abscess formation.
Although fungal vertebral osteomyelitis is a rare condition, oncologists should be aware of the potential diagnosis, particularly in a patient receiving chemotherapy who presents with symptoms of back pain, fever, night sweats and malaise. Our case illustrates the importance of suspicion if a solitary vertebra is involved, particularly with a history of previous surgical intervention at that site. A tissue diagnosis, especially in cases of spinal cord compression, should be sought so that appropriate therapy can be commenced. This case highlights the importance of awareness and vigilance for treatable non-malignant complications in patients with metastatic disease.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Jevtic V. Vertebral infection. Eur Radiol 2004;14(Suppl 3): E43–E52.
- Keating P. Fungus infection of bone and joint. South Med J 1932;25:1072–9.
- Tack KJ, Rhame FS, Brown B, Thompson RC, Jr. Aspergillus osteomyelitis. Report of four cases and review of the literature. Am J Med 1982;73:295–300.
