Abstract
The urinary bladder shows considerable individual variation in shape and position during a course of radiotherapy (RT). In this study we have developed and compared three different adaptive RT (ART) strategies for bladder cancer involving daily cone beam CT (CBCT) imaging and plan selection. Material and methods. Ten patients treated for bladder cancer had daily CBCTs acquired that were registered online using bony anatomy registration. Seven patients received intensity modulated RT (IMRT) with a simultaneous integrated boost (SIB) technique to the bladder and pelvic lymph nodes. Three patients received treatment to the bladder only. Retrospectively, we compared three ART strategies that were all based on daily selection of the most suitable plan from a library consisting of three IMRT-plans corresponding to a small, medium and large target volume. ART method A utilised population-based margins while methods B and C used the bladder as seen on CBCT-scans from the first week of treatment; method B without delineation of the bladder on CBCT and method C with delineation of the bladder. Total dose distributions were calculated using the planning CT. For each patient, we calculated ratios of the dose volume histograms (DVHs) for the three ART strategies relative to non-adaptive therapy. Results. The inter-patient variation was large for all three ART strategies. The mean ratios of the volumes receiving 57 Gy or more (corresponding to 95% of prescribed dose) for methods A, B and C were 0.66 (SD: 0.11), 0.67 (SD: 0.13) and 0.67 (SD: 0.16) respectively when compared to the non-adaptive plan. Conclusion. When using any of the ART strategies, it is possible to reduce significantly the volumes receiving high doses compared to the use of a standard non-adaptive plan. The differences in dose volume parameters between the three methods were small compared with the differences from the standard plan.
A major challenge in radiotherapy (RT) is to find the optimal trade-off between tumour coverage and sparing of the surrounding normal tissue. This has been the driving force behind the quest for better dose conformity that has shaped many of the developments in RT. The introduction of intensity-modulated RT (IMRT) has led to a significant step forward in dose conformity around the target with respect to the prescribed dose levels [Citation1], but the integral dose of IMRT plans has not been reduced compared to 3DCRT [Citation2]. The high degree of conformity requires a better setup precision and has lead to image-guided RT (IGRT) solutions using either 2D orthogonal setup images or 3D cone beam CT (CBCT). IGRT with daily/frequent correction of the isocenter position based on imaging of the patient on the treatment couch reduces the setup margins and thereby the volume treated to the prescribed dose [Citation3–6]. Further reduction in this volume are likely to be possible if ART strategies based on CBCT or repeated CT were considered [Citation7–9]. Without such approaches, large internal margins are still needed when treating targets in the pelvic region [Citation10]. Because of the nature of the variation in shape and size of the bladder [Citation11,Citation12], online adaptive strategies using CBCT for treating bladder cancer patients seems appealing.
The purpose of this study was to compare different ART strategies with respect to total integral dose and to explore the normal tissue sparing potential of such techniques. A method based on the planning CT only was compared with two more individualised approaches, one of them requiring target delineation on CBCT from the first four fractions and the other using the first five CBCT-scans without target delineation.
Material and methods
Patients
Bladder cancer patients with daily CBCT (OBI v. 1.3 and 1.4, Varian Medical Systems, Palo Alto, CA, USA) were considered and ten male patients with a total of 300 CBCT scans were included. The mean age was 74 years (range: 66–80 years). Seven of the patients had a T2N0M0 tumour, two patients had a T3 tumour and one patient had a T4a tumour. Two of the patients had the prostate included in the CTV. The patients were treated from June 2008 to January 2010.
CT-scanning, delineation and clinical treatment planning
All patients were instructed to empty their bladder prior to the acquisition of the planning CT and prior to all treatment sessions. Treatment planning was based on a fan-beam helical CT scan (Phillips Mx8000 IDT 16, Philips Medical Systems, Eindhoven, The Netherlands) with 3 mm slice spacing and a pixel size of 0.98 × 0.98 mm acquired about one week before treatment started. The clinical target volumes of the bladder (CTVplan) and lymph nodes (CTV-LN) were delineated in collaboration between a radiation oncologist and a diagnostic radiologist. The CTV included the bladder wall and its contents. The internal margin from CTVplan to ITV was 20 mm anterior and superior, 15 mm posterior and 10 mm in the remaining directions. The clinically used setup margins from ITV to PTV were 5 mm in the axial plane and 8 mm in cranial-caudal direction. The CTV-LN was contoured from the level of the promontory, the internal iliac nodes to the obturator fossa and the extern iliac nodes to the level of the femoral heads. Pre-sacral and para-rectal nodes under the sacroiliac joint were excluded. For the rectum, the recto-sigmoid flexure or sacroiliac joint was applied as the cranial limit and the anal verge as the caudal limit.
For the purpose of this study, the bowel cavity was contoured from the upper level of the 5th lumbar spine to the last CT slice that included a bowel segment excluding the bladder and rectum anterior to the abdominal/pelvic wall and laterally to the pelvic wall. A rectum planning organ at risk volume (PRV) was generated from the rectum using margins of 11 mm posterior and 16 mm anterior as suggested in a study by Muren and colleagues [Citation13]. A margin of 11 mm was applied laterally as the patients in this study were treated with IMRT and not CRT as in the work of Muren et al.
Patients were planned and treated with a 6-field dynamic IMRT plan using Eclipse (Eclipse v. 8.4 and 8.6, Varian Medical Systems). Treatment was delivered following set-up based on daily CBCT acquisition (see details in next session) and online bony anatomy registration. Dose homogeneity was specified according to ICRU 62 [Citation14]. The clinically used plan for each of the patients is referred to in the following as the standard plan.
Image material and construction of ART Volumes
The standard pelvic acquisition mode was used for daily CBCT imaging utilising a half fan x-ray beam and bow-tie filter (On-Board Imager, Varian Medical Systems, Palo Alto, CA, USA). A length of 16 cm in the cranial-caudal direction of the patient was scanned symmetrically around the isocenter. Default image reconstruction parameters were set to create CBCT image sets with a slice separation of 3 mm and an in-slice pixel size of 0.97 × 0.97 mm.
ART method A. Population-based treatment margins for bladder cancer were obtained from a study by Redpath and Muren [Citation15]. They calculated the percentage of the population that had their CTV covered for all but one fraction as a function of the margins in all six orthogonal directions. Using these data we obtained the margins needed in all six directions to cover 50%, 70% and 90% of the population, corresponding to the small, medium and large Plan Selection Volume (PSV) for ART method A.
ART method B. Method B utilised manual scoring of the bladder size compared to the CTVplan. PSVsmall was defined as CTVplan with an isotropic margin of 5 mm added. PSVlarge was created from CTVplan with an anterior and superior margin of 20 mm, a posterior margin of 15 mm and the remaining directions with 10 mm margin. Using the online match of each of the first five CBCT-scans to the plan CT, CTVplan could be seen as an overlay on each CBCT in our standard offline software (OBI software, Varian Medical Systems). With the CTVplan as an overlay we recorded, for each of the six directions, how many of the bladders on the first five CBCT scans that extended outside CTVplan. These numbers were used to scale the margin used for PSVB, medium. If, for instance, one patient had three of the CBCT bladders that needed a posterior margin outside the CTVplan, the posterior margin for PSVmedium was calculated as 3/5 of the posterior margin for PSVlarge. However, a minimum of 5 mm margin was added in all directions. The technique has two extremes; if all bladders in the first five fractions were covered by CTVplan, the volumes for the small and medium cases were identical; if all bladders extended beyond the CTVplan in all directions, volumes for medium and large cases were identical. This technique resulted in volumes that take systematic deviations into account.
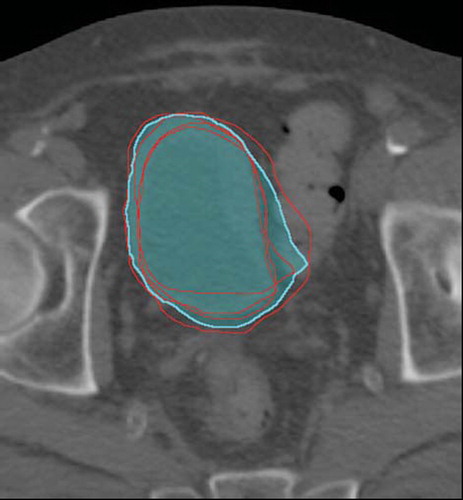
ART method C. Wright et al. explored several possibilities for constructing ART volumes, using the bladder as delineated on the planning CT and a number of CBCT-scans [Citation16]. The proposed volumes were for the small bladder size, i.e. the volume contained in at least two of five CTVs considered (). When applying this method we used the five CTVs as delineated on the planning CT and the CBCT-scans from the first four fractions; the latter was transformed to the planning CT using bony anatomy registration (the method was originally developed using soft-tissue registration on the bladder [Citation16]). The medium size volume PSVmedium was the union of the same five CTVs and the large size volume PSVC, Large was the same as PSVB, Large. In a clinical setting, this method will make the planning procedure (that would take place after the first week of treatment in order to acquire the involved CBCT scans), somewhat more time consuming than method B, as delineation on the CBCT-scans are needed.
Adaptive planning and daily plan selection
For each of the three methods, three corresponding PTVs were constructed by applying an isotropic margin of 3 mm to the PSVs to account for intra-fractional changes of the bladder shape and size. As the bladder should be covered by the chosen PSV, no setup margin was applied. The resulting mean volume ratios of the PTVs for the adaptive plans relative to the PTVs for the standard plan are given in for patients with simultaneous integrated boost technique (SIB) and for patients treated to the bladder only. For each ART strategy, three new treatment plans were constructed with the clinically used plan as the starting point for the optimisations. The optimisation constraints were adapted and a new optimisation volume was added to ensure conformity. The resulting plans had at least 99% of the corresponding PTV covered by 95% of the prescribed dose of 60 Gy.
Table I. The mean volume ratios of the PTVs for the three ART strategies vs. the standard non-adaptive RT are given separately for patients treated with SIB and those treated to the bladder only.
The online match of the CBCT-scans to the planning CT was reviewed offline for each fraction and for every patient using an overlay of the PSVs for each method. Selection of the treatment plan for each method was done by two observers. Whenever there was doubt (usually due to image quality issues), the larger volume was chosen. In all 30 CBCT scans, the smallest possible PSV that included the CBCT bladder was chosen. In the case of the two individualised methods B and C, the first five fractions were all supposed delivered using the plan with the largest PTV. Method C uses CBCT-scans from the first four fractions and one treatment day was added to allow for treatment planning in a clinical setting.
DVH analysis
The total summed dose distribution which would have been delivered to the patient if the ART strategies had been used was calculated on the planning CT, using the number of fractions that each plan had been chosen. DVHs of body outline, bowel cavity and the rectum PRV were calculated for the added ART-plans and the standard plan. DVH ratios for dose bins of 1 Gy for the added ART plans relative to the standard plan were calculated for each patient. Mean DVH ratios and standard deviations were calculated for the patients with SIB. The three patients that received RT for the bladder only were evaluated separately.
Results
Plan selection frequencies
A considerable inter-patient variation in plan selection frequencies were seen for all three ART strategies (). The inter-patient variation was less for method B than for method A, but on average the two methods were comparable. For ART method C the large plan was chosen in nearly 70% of the treatment fractions while the small plan was used in less than 10% of the fractions.
Figure 2. The plan selection frequencies (the percentages of times each of the Small, Medium and Large plan was chosen) for each patient are shown for method A, B and C respectively. The last column is the average plan selection frequencies across all ten patients. Patient no. 10 had the large size plan chosen for method A in every fraction, because of a large rectum on the planning CT.
Coverage of the bladder
Four of the patients had one or more treatment fraction where the PSVLarge did not cover the bladder as seen on the CBCT. One had a large rectum and bladder on the planning CT resulting in a region of the bladder near the border of the prostate that was not adequately covered in most fractions when using method A (). In some fractions the standard plan PTV did not cover the bladder. Two other patients had a planning CT that was not representative of the treatment anatomy. These patients had parts of the bladder outside the PSVLarge in one or more fractions and the frequency of target miss was larger for the population-based method.
Figure 3. The number of treatment fractions, where the PSVlarge did not cover the bladder as seen on the CBCT are shown for each method. Patient no. 1 had an intestinal flexure making a concavity in the top of the bladder on the planning CT. Patient no. 2 had large differences in the rotational components in the bony anatomy match. Patient no. 4 had an intestinal flexure pushing the bladder to the right on the planning CT. Patient no. 10 had a large rectum on the plan CT.
Evaluation of dose volume parameters
For all ten patients the mean ratio of the volumes receiving 57 Gy or more (corresponding to 95% of prescribed dose) for methods A, B and C were 0.66 (SD: 0.11), 0.67 (SD: 0.13) and 0.67 (SD: 0.16) respectively when compared to the non-adaptive plan. For patients treated with the SIB technique, the DVH analysis showed that all three ART strategies led to considerable reductions in the volumes receiving doses above 48 Gy (corresponding to the dose prescribed to the pelvic lymph nodes) while only small reductions were obtained for doses below 48 Gy (). For the body outline, as much as a 30% reduction in the volume ratios was seen in the high dose region; the mean ratio of the volume receiving 57 Gy or more (V57) for methods A, B and C was 0.68 (SD: 0.08), 0.70 (SD: 0.12) and 0.72 (SD: 0.16), respectively when compared to the non-adaptive plan. The differences between the methods were small, with a slight tendency for a smaller reduction for method C. The reduction in the high-dose region was even more pronounced for the bowel cavity. As for the bowel cavity and the body outline, the low dose region of the rectum PRV was only marginally reduced, while both the intermediate and high dose range show large reductions for all ART strategies.
Figure 4. Mean ratio DVHs for the body outline (a) with standard deviations as error bars. Corresponding figures are shown for bowel cavity (b) and rectum PRV (c). The dotted line at unity volume ratio indicates where the ART method and the standard plan have the same volume.
For patients treated to the bladder only, the DVH ratios of the body outline showed broadly the same patterns as for the SIB patients (). However, more pronounced differences were observed for doses below 48 Gy for the patients treated to the bladder only. For the body outline, as much as a 40% reduction in the volume ratios was seen in the high dose region; the mean ratio of the volume receiving 57 Gy or more for methods A, B and C was 0.61, 0.61 and 0.57 respectively. The large inter-patient variation is illustrated by DVH ratios for rectum PRVs for these three patients ().
Figure 5. For method A, B and C, ratio DVHs of body outline (a) and rectum PRV (b) are shown for the three patients receiving treatment of the bladder only. The dotted line at unity volume ratio indicates where the ART method and the standard plan have the same volume. Patient no. 5 had prostate included in the CTV.
The mean ratios of V57ART relative to V57standard resulting from use of each of the adaptive plans throughout the course (i.e. with no daily plan selection) were found to be very similar to the ratios of the PTV volumes ().
Discussion
In this study we have compared three different ART methods with respect to plan selection frequencies and dose volume parameters for the body outline, bowel cavity and rectum PRV. For all three ART strategies a considerable inter-patient variation in plan selection frequency was found. All three methods led to a considerable reduction in the volumes of normal tissues receiving doses close to the prescription dose.
The population-based method (method A) showed large inter-patient variations in plan selection frequency. As the planning CT (only) was the basis of the PSVs for all patients with this approach, the success of the method depends strongly on the planning CT representing the patient anatomy during the course of treatment. In practise this means that patients with a planning CT which represents the treatment anatomy accurately is likely to benefit from this method, whereas patients that happen to have an atypically large or small bladder or rectum on the planning CT are likely to be better suited for the individualised treatment strategies. Method A and the first of the individualised approaches (method B) were found to be comparable in terms of both average plan selection frequency and in the average DVH ratio, but method B had less inter-patient variation. With this method, patient-specific information from the first five CBCT-scans was taken into account when constructing the PSVs. The plan selection volumes for method C generally fitted the bladder well, but the difference between the small and medium size PSVs appeared to be too small. This resulted in a high plan selection frequency for the large volume and generally the reduction in DVH ratio seemed smaller than for the other methods. The same tendencies were seen for the bowel cavity. The large reduction in dose to the rectum PRV is very promising, especially as seen for the patients with only bladder treatment. However, caution has to be taken in reducing margins, because of the risk of compromising target coverage [Citation17]. In treating bladder cancer patients with ART strategies, in particular the problem of intra-fractional changes has to be thoroughly addressed. A study by McBain and co-workers reported movements of the bladder wall of more than 15mm in eight of 19 patients for a 14 minute time interval [Citation12]. Acquisition of a weekly CBCT-scan after treatment delivery could be a possibility to decide on whether to continue the ART treatment. It should also be pointed out that arc therapy approaches reduce the beam-on time to about 2 minutes, which should make the intra-fractional changes less important. Further detailed studies are needed to document the clinical consequences with respect to both target coverage issues as well as reduced morbidity in treating bladder cancer patients with ART.
In this study all three ART strategies were based on a bony anatomy match, whereas the study of Wright et al. [Citation16] that developed the approach formulated as our method C, involved soft-tissue match on the bladder. A study by Redpath and Muren showed considerable differences in margins needed using registration on bladder versus bony anatomy [Citation18]. This may be a reason for the slightly inferior performance of method C. Matching on bony anatomy makes it possible to calculate the total dose delivered to the patient assuming the patient anatomy does not change during the treatment course, as represents what is present clinical practice.
In a few instances in our offline plan selection process (that simulated an on-line process) there was uncertainty with regard to whether a plan would give adequate coverage. In most cases this was due to inadequate image resolution in the region of the transition between the bladder and prostate. In these occasions we always took a conservative approach and selected the largest PSV, as it would be the case for clinical application of ART for bladder cancer.
Mathematically we introduced the concept of the ratios between DVHs. This worked well in this study since the ART plans had a lower maximum dose than the corresponding non-adaptive plan. Otherwise division by zero would result in a singularity.
Caution should be taken in the interpretation of the calculated dose to organs at risk like the PRV rectum and bowel cavity on basis of a planning CT, as done in this study. Ideally, a dose calculation on the CBCT-scan of each treatment would take into account inter-fractional changes in patient anatomy. Proper deformable registration algorithms are needed in order to be able to add the daily dose delivered to targets and organs at risk. Improvements in deformable registration algorithms have been shown in studies by Noe Østergaard [Citation19]. In the case of the bladder, a recent study by Thörnkvist [Citation20] showed that deformable registration could be performed with reasonable precision for the bladder but not for the rectum for the algorithms tested. DVHs based on dose calculations using daily CBCT should give a better correlation with normal tissue complications. Until now, doses of about 70 Gy have been reported to correlate with rectal toxicity, but recently doses in the range of 40–50 Gy have also shown correlation in several studies [Citation20,Citation21]. These could be a powerful tool in deciding on dose escalation in bladder cancer radiotherapy.
Reductions in treated volume of about 30% were seen for the ART methods when applied to patients treated with the SIB technique, whereas patients treated to the bladder alone had a reduction of about 40% in treated volume. This is the same reduction as seen in the study of Pos et al. where the reduction in PTV volume for their ART strategy of partial bladder RT was considered [Citation22]. Such large reductions are likely to enable a significant dose escalation while keeping morbidity levels at a tolerable level [Citation23].
In conclusion, we have evaluated three different strategies for daily plan selection using CBCT with matching on bony anatomy. The differences between the ART strategies were small compared to the large differences when compared to the non-adaptive plan. The strategy using population-based margins should be relatively straightforward to implement clinically with respect to workflow, whereas the strategies based on the first five CBCT-scans are likely to be more time-consuming. Before using these strategies it is important to have an on-site measure of the intra-fractional changes in bladder shape and size.
Acknowledgements
The authors would like to thank Antony Redpath for his assistance regarding this paper and to acknowledge the work of Ulrik Vindelev Elstrøm and Rune Groth Hansen in implementing daily online IGRT at Aarhus University Hospital.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Søndergaard J, Høyer M, Petersen JB, Wright P, Grau C, Muren LP. The normal tissue sparing obtained with simultaneous treatment of pelvic lymph nodes and bladder using intensity-modulated radiotherapy. Acta Oncol 2009;48:238–4.
- Reese AS, Das SK, Curie C, Marks LB. Integral dose conservation in radiotherapy. Med Phys 2009;36:734–40.
- Wright P, Redpath AT, Høyer M, Grau C, Muren LP. The normal tissue sparing potential of adaptive strategies in radiotherapy of bladder cancer. Acta Oncol 2008;47:1382–9.
- Redpath AT, Wright P, Muren LP. The contribution of on-line correction for rotational organ motion in image-guided radiotherapy of the bladder and prostate. Acta Oncol 2008;47: 1367–72.
- Søndergaard J, Olsen K, Muren LP, Elstrøm UV, Grau C, Høyer M. A study of image-guided radiotherapy of bladder cancer based on lipiodol injection in the bladder wall. Acta Oncol 2010;49:1109–15.
- Pos F, Bex A, Dees-Ribbers HM, Betgen A, van Herk M, Remeijer P. Lipiodol injection for target volume delineation and image guidance during radiotherapy for bladder cancer. Radiother Oncol 2009;93:364–7.
- Grau C, Muren LP, Høyer M, Lindegaard J, Overgaard J. Image-guided radiotherapy – integration of biology and technology to improve clinical outcome. Acta Oncol 2008;47: 1182–5.
- Yan D, Vicini F, Wong J, Martinez A. Adaptive radiation therapy. Phys Med Biol 1997;42:123–32.
- Hawkins MA, Brooks C, Hansen VN, Aitken A, Tait D. Cone beam computed tomography- derived adaptive radiotherapy for radical treatment of esophageal cancer. Int J Radiat Oncol Biol Phys 2010;77:378–83.
- Chan P, Dinniwell R, Haider MA, Cho YB, Jaffray D, Lockwood G, . Inter- and intrafractional tumor and organ movement in patients with cervical cancer undergoing radiotherapy: A cinematic-MRI point-of-interest study. Int J Radiat Oncol Biol Phys 2008;70:1507–15.
- Lotz HT, Pos FJ, Hulshof M, van Herk M, Lebesque JV, Duppen JC, . Tumor motion and deformation during external radiotherapy of bladder cancer. Int J Radiat Oncol Biol Phys 2006;64:1551–8.
- McBain C, Khoo V, Buckley L, Sykes JS, Green MM, Cowan RA, . Assessment of bladder motion for clinical radiotherapy practice using cine-MRI resonance imaging. Int J Radiat Oncol Biol Phys 2009;75:664–71.
- Muren LP, Karlsdottir Á, Kvinnsland Y, Wentzel-Larsen T, Dahl O. Testing the new ICRU 62 ‘Planning Organ at Risk Volume’ concept for the rectum. Radiother Oncol 2005;75: 293–302.
- ICRU Report 62, Prescribing, recording and reporting photon beam therapy (supplement to ICRU Report 50). 1999.
- Redpath AT, Muren LP. An optimisation algorithm for determination of treatment margins around moving and deformable targets. Radiother Oncol 2005;77:194–201.
- Wright P, Redpath AT, Høyer M, Muren LP. A method to individualize adaptive planning target volumes for deformable targets. Phys Med Biol 2009;54:7121–33.
- Engels B, Soete G, Verellen D, Storme G. Conformal arc radiotherapy for prostate cancer: Increased biochemical failure in patients with distended rectum on the planning computed tomogram despite image guidance by implanted markers. Int J Radiat Oncol Biol Phys 2009;74:388–91.
- Redpath AT, Muren LP. CT-guided intensity-modulated radiotherapy for bladder cancer: Isocenter shifts, margins and their impact on target dose. Radiother Oncol 2006;81:276–83.
- Østergaard KN, De Senneville BD, Elstrøm UV, Tanderup K, Sørensen TS. Acceleration and validation of optical flow based deformable registration for image-guided radiotherapy. Acta Oncol 2008;47:1286–93.
- Thornkvist S, Petersen JB, Høyer M, Benzen L, Hysing L, Muren LP. Propagation of target and organ at risk contours in prostate cancer using deformable image registration. Acta Oncol 2010;49:1023–32.
- Fiorino C, Valdagni R, Rancati T, Sanguineti G. Dose-volume effects for normal tissues in external radiotherapy: Pelvis. Radiother Oncol 2009;93:153–67.
- Pos F, Hulshof M, Lebesque J, Lotz H, Van Tienhoven G, Moonen L, . Adaptive radiotherapy for invasive bladder cancer: A feasibility study. Int J Radiat Oncol Biol Phys 2006;64:862–8.
- Pos F, Remeijer P. Adaptive management of bladder cancer radiotherapy. Semin Radiat Oncol 2010;20:116–20.