Abstract
Purpose: To assess the impact of using breathing adapted radiotherapy on contralateral breast (CB) dose, to relate the thorax shape with the dose to the organs at risk (OARs) and to predict the risk for induced malignancies in CB using linear and non-linear models, following tangential irradiation of breast. Material and methods. Sixteen patients with stage I-II breast cancer treatment planned with tangential fields using deep inspiration breath hold (DIBH) and free breathing (FB) techniques were included in this analysis. The dose results mainly based on DVH analysis were compared. Four parameters were defined to describe thoracic shape. Excess relative risk (ERR) for cancer induction in CB, employing linear and non-linear models was calculated. Results. Average CB volumes exposed to a dose of 1 Gy is 1.3 times higher in DIBH plans than in FB plans. No significant difference in average V3Gy and V5Gy for DIBH and FB plans is observed. The average mean CB dose for DIBH and FB plans is 0.33 and 0.28 Gy, respectively. No correlation between thorax shape parameters and mean OARs dose is observed. The estimated average mean ERR with linear model is lower in FB plans (0.12) than for the DIBH plans (0.14). The estimated ERR with non-linear model is 0.14 for DIBH plans and 0.15 for FB plans. Conclusion. No significant difference in CB dose between DIBH and FB plans is observed. The four thorax shape parameters defined in this study can not be related to the dose at OARs using DIBH and FB radiation techniques. The ERR estimates for secondary CB cancer are nearly the same for FB and DIBH planning when using a linear and non-linear risk prediction models.
Postoperative radiotherapy (RT) is an important part of the multidisciplinary treatment of early breast cancer (BC). It is established that postoperative radiotherapy reduces local-regional recurrence rates of primary breast cancer by 2/3 of that of surgery alone [Citation1]. There is also clinical evidence that RT may increase long-term survival rates of early breast cancer [Citation2–4]. Radiation exposure can on the other hand lead to increased late radiation effects like cardiac mortality [Citation5] and radiation induced contralateral breast (CB) cancer [Citation6,Citation7] in this patient group.
Radiation exposure to parts of the heart, particularly in left-sided BC, ipsilateral lung and CB seems to be unavoidable in BC patients receiving RT.
Modern treatment techniques have the potential of reducing the risk of radiation induced late side effects by reducing the normal tissue organ volume exposed to radiation. It has been demonstrated that breathing adapted radiotherapy (BART), also referred to as respiratory gated RT, during deep inspiration breath-hold (DIBH) can provide lung and especially heart dose reduction without compromising dose coverage to the planning target volume (PTV) [Citation8,Citation9]. It is of interest to explore a possible influence of gated irradiation on dose to the CB through a detailed evaluation of the dose distribution and comparing it with conventional free breathing (FB) technique. A mean CB dose ranging from 1 to 15% of the prescribed dose as a result of irradiation of the breast is already reported using conventional technique [Citation10]. In this study treatment plans employing DIBH technique are compared to FB technique in order to investigate the possible impact of DIBH with respect to CB exposure.
DIBH radiation technique can be resource-demanding. Therefore it is desirable to know in advance which patient benefits most from treatment with this technique. For this reason a possible correlation between thorax shape and the dose to the involved organs at risk (OARs) employing both DIBH and FB radiation treatments are investigated in the current study.
Earlier diagnoses of breast cancer and relatively longer survival also emphasize the concern for radiation induced CB malignancy. The CB dose distributions are further used to estimate the potential risk of secondary malignancy in the CB associated with radiation therapy [Citation11].
Material and methods
In this study, CT series of 16 patients stage I/II with operable, pT1-pT2 tumors who had undergone breast conserving surgery referred for adjuvant radiotherapy at Stavanger University Hospital were included. Eleven patients had left-sided cancer and five had right-sided, however in the previous study [Citation9] the left breast was defined as target in all patients in order to quantify the doses to the heart and other OARs for tangential left breast treatment. Seven of 16 patients received adjuvant chemotherapy. The study was approved by the Regional Committee for Medical Research Ethics, and a written consent was obtained before the patients were included in the study. The prescribed dose in the study was 50 Gy to the breast, in 2 Gy fractions. Each patient underwent two CT scans; during FB and DIBH, respectively. Each CT scan was undertaken at 3 mm intervals and encompassed both breast and the whole thoracic cavity to include heart and both lungs.
The Varian RPM™ respiratory gating system, version 1.6 (Varian Medical Systems, Palo Alto, CA) was used for respiratory control. Each patient received an individual, but standardized respiratory training session before CT scanning. The patients were placed in the treatment position in an immobilization device, and the DIBH breathing pattern was explained and rehearsed with the patient. An infrared reflecting marker was placed on the patient, normally over the xiphoid process, and a video camera registered the anterior posterior movement of the marker, and hence the chest wall, due to respiration. The accelerator can then be controlled to irradiate only in a preselected interval of the chest wall displacement, the so-called gating window. In this study, the gating window was individually chosen to the mean amplitude of the stable plateau phase of DIBH.
Remaining mammary glandular tissue constitute the clinical target volume (CTV) after breast conserving surgery. The contralateral breast, heart, and ipsilateral lung are considered organs at risk. The volumes were delineated according to national guidelines. For consistency, delineation of CTV and the contralateral breast was performed by the same oncologist for all patients, using the Eclipse treatment planning system, version 8.0 (Varian Medical Systems). The details of CTV, heart and lung dose analyses are already published as well as a preliminary report on the dose to CB by Vikström et al. [Citation9]. In the current paper a detailed analysis of the dose distribution in CB is provided.
The CB dose analysis included the mean, maximum dose and a set of appropriate V-values (V1Gy, V3Gy and V5Gy) for CB where V is the volume (%) receiving a defined dose (Gy).
Sixteen breast cancer patients were planned employing tangential fields. A similar PTV dose distribution in both plans was emphasized [Citation9]. The calculation algorithm was Eclipse Analytical Anisotropic Algorithm (AAA). The dose distribution was normalized to the mean dose of the PTV. The grid size in the dose calculation matrix was 0.25 cm.
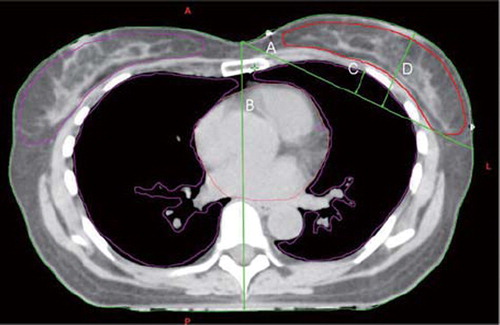
Four thorax shape parameters were defined as illustrated in . The tangential diameter, A, was defined as the line between the middle of the patient (center line) along the most dorsal part of the CTV to the body contour. Orthogonally from the tangential diameter, the maximum lung and breast diameter, C and D, were measured. The orthogonal distance in the center line of the chest, B, was also measured. All measurements were performed in the CT slice containing the isocenter of the plan. The mean dose to ipsilateral lung, heart and CB was used to investigate a possible correlation between the doses in the OARs and the defined thorax shape parameter values.
Figure 1. Four thorax shape parameters are defined; A = Tangential diameter, B = central diameter, C = Lung orthogonal diameter and D = breast orthogonal diameter.
To assess difference between DIBH and FB plans, paired t-test, independent sample t-test and Wilcoxon non-parametric test were employed. A p-value of <0.05 was considered to be statistically significant.
Linear and non-linear models (Equations 1 and 2) as described in more detail in an earlier study [Citation11] and in the appendix were employed to estimate excess relative risk (ERR) for breast cancer induction.
where ERRD is ERR per dose (Gy) and with a suggested value of 0.86 Gy–1 for breast cancer induction caused by acute irradiation [Citation12] and D is the mean CB dose. In this study ERRD was reduced by a factor of 2 and set to 0.43 Gy−1 to account for fractionated radiation treatment [Citation11].
The non-linear model is suggested by Dasu et al. [Citation13] and consists of two terms. The first term describes the induction of DNA mutations, and thus pre-malignant cells. The second term describes the cell survival:
where D is each dose interval of the dose-volume histogram, n number of fractions, α1 and β1 are radiation induced mutation parameters, and α2 and β2 are cell survival parameters.
The risk was estimated using the following parameter values α1/β1 and α2/β2 = 4 Gy, α1 = 0.002 Gy-1 and α2 = 0.25 Gy–1. The risk of malignancy induction is calculated for each dose interval of the dose volume histogram using the non-linear model [Citation11]. The details of the risk prediction by non-linear model have been published previously [Citation11].
Results
The average mean CB dose is 0.7% and 0.6% of the prescribed dose for DIBH (0.33 Gy) and FB plans (0.28 Gy) (). The CB V1Gy dose is higher in DIBH plans (6.8%) compared to FB plans (5.1%) (ρ = 0.1). The CB V5Gy and maximum doses are slightly higher in FB plans (0.3 and 5.4%) than in DIBH plans (0.1 and 5.2%) as shown in . These differences are not statistically significant.
Table I. Summary of cumulative DVH analysis for CB for the cohort of 16 breast cancer patients included in this study, for tangential fields with FB (conventional) and DIBH techniques. CB data are shown as V1Gy, V3Gy, V5Gy, mean, and maximum.
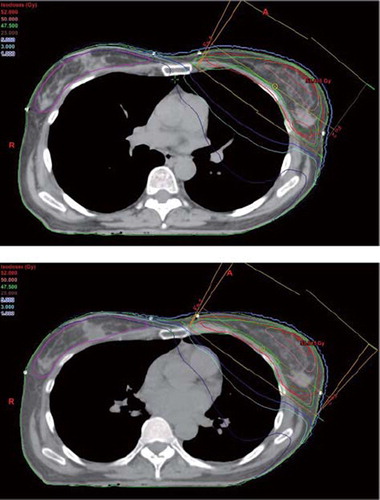
The four defined thoracic shape parameters for both DIBH and FB plans are shown in , upper and lower panel, respectively. The average breast and tangential diameters are approximately the same for FB plans (6.77 and 20.55 cm) compared to DIBH plans (6.75 and 20.41 cm) (). The average lung and central diameters for DIBH plans are slightly higher than for the average FB plans with a difference of 0.2 and 1.1 cm (), due to increased lung volume under DIBH condition.
Table II. Contour measurements data. Four parameters are made to define thorax shape for both DIBH and FB plans.
The mean dose to heart, ipsilateral lung and CB is shown in for both DIBH and FB plans, upper and lower panel, respectively. No clear correlation is observed between the mean dose to OARs () and the defined thorax shape parameters as shown in . However, the difference in average mean dose for heart and lung using DIBH and FB techniques is significant as shown in an earlier study [Citation9].
Table III. Mean dose for three organs at risk and ERR estimated with linear and non-linear risk models for DIBH and FB plans in 16 breast cancer patients. Individual differential DVHs and mean CB dose are used to calculate ERR with non-linear and lineal model. Following parameter values are employed in risk estimations with non-linear model; α1/ß1 and α2/ß2 = 2 Gy, α1 = 0.002 Gy-1 and α2 = 0.25 Gy-1.
Calculated excess relative risk (ERR) using the linear and non-linear models, as described by Equations 1 and 2 and in an earlier study [11 & appendix], is also shown in for the 16 patients planned with DIBH and FB techniques. The average ERR estimates using linear model is lower in FB plans. The difference between calculated ERR with linear risk estimation model for DIBH and FB plans is not statistically significant (ρ = 0.6). The mean ERR estimated with non-linear model is slightly higher for the FB plans (0.15) compared to DIBH plans (0.14), but this difference is not statistically significant (ρ = 0.7).
Discussion
Breathing-related movement has been a continuous challenge in radiotherapy and vast efforts have been invested in addressing this issue. Several studies have investigated the effect of delivering the radiation treatment to a pre-determined breathing amplitude with respect to possibility of reduced involvement of organs at risk. Korreman et al. [Citation14] have studied the impact of different respiratory techniques on cardiopulmonary doses to BC patients receiving adjuvant RT. They concluded that end-inspiration gating and DIBH both reduced the cardiac doses and spared pulmonary tissue to a large extent. Chen et al. [Citation15] assessed the irradiated cardiac volume in 17 patients treated with RT. They concluded that deep inspiratory maneuvers significantly decreased cardiac volume included in the left breast radiation field. These results are consistent with the data shown in the study of Vikström et al. [Citation9]. The focus of earlier studies on gating in breast cancer RT has been on sparing heart and lung tissue. To our knowledge, no studies have investigated the possible impact of using gated RT on the dose to other organs at risk, such as the contralateral breast (CB).
The average V1Gy and mean dose are slightly higher in the DIBH plans (). This appears to be related to the decreased lung density observed with deep inspiration. It is demonstrated in the study of Hanley et al. [Citation16] and Stromberg et al. [Citation17] that lower lung density results in dose reduction to the normal tissue located inside the field portals, but the dose impact on the out of field region is not discussed in their study. With the DIBH technique lung density decreases, leading to an increased photon beam transmission through lung tissue. Our investigation as illustrated in and indicates that this has caused an increased dose in the medial sternum region as shown in the upper panel figure (DIBH) compared to the lower panel figure (FB) and may explained the increased medial dose in the irradiated region and increased CB dose.
Figure 2. The reduced lung and cardiac and increased medial sternum dose as a result of decreased lung density in DIBH plan (upper panel) compared to the FB plan (lower panel).
Respiratory gated RT may require some additional time and resources which could limit the possibility to offer the technique to all BC patients. However, the benefit of gating differs a lot between patients. To assess a relationship between the thorax shape and dose to OARs seems to be useful in choice of breast cancer patients who benefit most from DIBH technique. In a study carried out by Vikström et al. [Citation9], the correlation between heart dose and maximum heart distance (MHD) is shown. Vikström and colleagues have found that lower average MHD leads to lower mean heart dose which was achieved by DIBH techniques in breast cancer radiation. The analysis of central lung distance (CLD) value in the same study indicates that an increased mean CLD causes a reduction in mean ipsilateral lung volume using DIBH technique [Citation9]. In another study carried out by Correa et al. [Citation18] a clear correlation between cardiac test abnormalities and median central lung distance (CLD) was found. Their analysis of CLD parameter value refers to an increased mean CLD for patients with cardiac test abnormalities [Citation18]. In our investigation, no correlation between the four defined thorax shape parameters and dose to the OARs heart, lung and CB employing the DIBH and FB radiation techniques is observed. A reason for this can be the breast cancer population included in this study is too small to represent the spectrum of breast cancer patients treated in daily practice or that the internal anatomical differences are large and no correlation to external markers exists.
Assuming a linear dose-tumor induction relationship, an insignificant decrease of average risk for secondary CB cancer was observed with FB planning (). This observed decrease of ERR estimated linearly derives from the lower mean doses ( and ) administered to CB with FB planning. The average ERR predicted with non-linear risk model is nearly similar for both plans () as the dose difference in both low and middle high dose regions are nearly identical for both techniques (). The study of Boice et al. [Citation19] shows a mean breast dose of 0.76, 12.15, 1.5 and 2.47 Gy in Atomic bomb survivors, Nova Scotia/Massachusetts fluoroscopy and Rochester mastitis patients, respectively. The same data indicated an increase in relative risk per cGy of 0.9, 0.78, 0.53 and 0.49% in the same studies, respectively [Citation19]. Tubiana [Citation20] discussed the carcinogenetic effect for doses as low as 2 Gy per fraction. These data show how important it is to keep the breast dose as low as possible. Our study shows a slightly lower CB dose in low dose region when using FB technique (). However, with the significantly lower cardiopulmonary doses achievable with DIBH technique [Citation9] this significant increase in CB dose is a reasonable price to pay. Our results also show that the average risk for induction of secondary CB malignancy is lower when using a linear risk model under the FB condition compared to DIBH ( and ). However, it is important to point out that the scarce knowledge about the parameter values and the pre-malignant cell behavior in higher dose region has an unavoidable impact on the risk assessment with mathematical models which makes it less valid and robust (supplementary appendix to be found online, at http//www.informaworld.com/doi/abs/10.3109/0284186X.2010.541933).
In conclusion, treatment planning of 16 left-sided breast cancer patients with tangential fields using either DIBH or FB techniques, where also the risk for radiation induced malignancies in the contralateral breast is calculated, shows no statistically significant difference in CB dose between DIBH and FB plans. No correlation between the defined thorax shape parameters and dose to OARs in this study's population employing DIBH or FB planning was revealed. The ERR estimates for secondary CB cancer are lower for FB planning when using a linear risk prediction model.
Supplementary material available online
Supplementary Material
Download PDF (113.9 KB)Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) – Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: An overview of the randomised trials. Lancet 2005;366:2087–106.
- Early Breast Cancer Trialists’ Collaborative Group. Effects of radiotherapy and surgery in early breast cancer. An overview of the randomized trials. N Engl J Med 1995;333:1444–55.
- Steele Jr, Jessup GD, Winchester LM, Murphy DP, Menck HR. Clinical highlights from the National Cancer Data Base: 1995. CA Cancer J Clin 1995;45:102–11.
- Vallis KA, Tannock IF. Postoperative radiotherapy for breast cancer: Growing evidence for an impact on survival. J Natl Cancer Inst 2004;96:88–9.
- Gagliardi G, Lax I, Ottolenghi A, Rutqvist LE. Long term cardiac mortality after radiotherapy of breast cancer – application of the relative seriality model. Br J Radiol 1996;69:839–46.
- Boice JD Jr. Radiation and breast carcinogenesis. Med Pediatr Oncol 2001;36:508–13.
- Gao X, Fisher SG, Emami B. Risk of second primary cancer in the contralateral breast in women treated for early-stage breast cancer: A population-based study. Int J Radiat Oncol Biol Phys 2003;56:1038–45.
- Pedersen AN, Korreman S, Nyström H, Specht L. Breathing adapted radiotherapy of breast cancer: Reduction of cardiac and pulmonary doses using voluntary inspiration breath-hold. Radiother Oncol 2004;72:53–60.
- Vikström J, Hjelstuen MHB, Mjaaland I, Dybvik KI. Cardiac and pulmonary dose reduction for tangentially irradiated breast cancer, utilizing deep inspiration breath-hold with audio-visual guidance, without compromising target coverage. Acta Oncol 2010; [Epub ahead of print], 1–9.
- Johansen S, Olsen DR, Danielsen T, Malinen E. Contralateral breast doses following radiotherapy of the breast and regional lymph nodes: Measurements and treatment planning calculations. Radiother Oncol 2007;82:332–6.
- Johansen S, Danielsen T, Olsen DR. Estimated risk for secondary cancer in the contra-lateral breast following radiation therapy of breast cancer. Acta Oncol 2008;47:391–6.
- Preston DL, Mattsson A, Holmberg E, Shore R, Hildreth NG, Boice JD Jr. Radiation effects on breast cancer risk: A pooled analysis of eight cohorts. Radiat Res 2002;158:220–35.
- Dasu A, Toma-Dasu I, Olofsson J, Karlsson M. The use of risk estimation models for the induction of secondary cancer following radiotherapy. Acta Oncol 2005;44:339–47.
- Korreman SS, Pedersen AN, Josipovic M, Aarup LR, Juhler-Nøttrup T, Specht L, . Cardiac and pulmonary complication probabilities for breast cancer patients after routine end-inspiration gated radiotherapy. Radiother Oncol 2006;8:257–62.
- Chen MH, Cash EP, Danias PG, Kissinger KV, Bornstein BA, Rhodes LM, . Respiratory maneuvers decrease irradiated cardiac volume in patients with left-sided breast cancer. J Cardiovasc Magn Reson 2002;4:265–71.
- Hanley J, Debrois MM, Mah D, Mageras GS, Raben A, Rosenzweig K, . Deep inspiration breath-hold technique for lung tumors: The potential value of target immobilization and reduced lung density in dose escalation. Int J Radiat Oncol Biol Phys 1999;45:603–11.
- Stromberg JS, Sharpe MB, Kim LH, Kini VR, Jaffray DA, Martinez AA, . Active breathing control (ABC) for Hodgkin's disease: Reduction in normal tissue irradiation with deep inspiration and implications for treatment. Int J Radiat Oncol Biol Phys 2000;48:797–806.
- Correa CR, Das IJ, Litt HI, Ferrari V, Hwang WT, Solin LJ, . Association between tangential beam treatment parameters and cardiac abnormalities after definitive radiation treatment for left-sided breast cancer. Int J Radiat Oncol Biol Phys 2008;72:508–16.
- Boice JD Jr, Land CE, Shore RE, Norman JE, Tokunaga M. Risk of breast cancer following low-dose radiation exposure. Radiology 1979;131:589–97.
- Tubiana M. Can we reduce the incidence of second primary malignancies occurring after radiotherapy? A critical review. Radiother Oncol 2009;91:4–15.
- Hall EJ, Wuu CS. Radiation-induced second cancers: The impact of 3D-CRT and IMRT. Int J Radiat Oncol Biol Phys 2003;56:83–8.
- Sachs RK, Brenner DJ. Solid tumor risk after high doses of ionizing radiation. Pnas 2005;102:13040–5.
- Sachs RK, Shuryak I, Brenner D, Fakir H, Hahnfedt P. Second cancers after fractionated radiotherapy: Stochastic population dynamics effects. J Theor Biol 2007;249:518–31.