To the Editor,
The use of radiation therapy in the post-lumpectomy/mastectomy setting in breast cancer is current standard of care and is an effective means of decreasing locoregional recurrences with good cosmetic results [Citation1–3]. However, after 10–15 years of radiation treatment, excess lung and cardiac mortalities are also coming into the picture for older radiation treatment techniques [Citation4,Citation5]. Modern treatment techniques such as field-in-field (FIF), intensity modulated radiation therapy (IMRT) and rotational therapy provide dose-volume information for outcome analysis. The conventional treatment methods [two-dimensional (2D)] are still being used in many parts of the world and require volumetric information in order to estimate the dose to a portion of lung and cardiac tissue. The volume of critical structures in the treatment fields can vary greatly due to intrinsic factors such as patient anatomy and tumor location; straining the balance between dose homogeneity and dose to the adjacent organs.
Minimizing heart and lung dose when planning for breast radiation are well known concepts and being routinely performed with 3D treatment, however correlating treatment parameters from 2D to 3D treatment is still needed for the analysis of the outcome. Although the incidental dose to the structures surrounding the breast tissue is relatively low in image based treatment, it has been implicated in causing numerous adverse effects, especially in predisposed patients. A recent prospective study demonstrated that limiting the dose to the lung≤ 25 Gy can significantly limit pulmonary toxicity [Citation6]. Mathematical models [Citation7–10] have demonstrated the correlation of lung distance to the amount of treated lung. Central lung distance (CLD) has been shown to be a significant indicator of ipsilateral irradiated lung volume [Citation7,Citation9,Citation11]. A CLD of< 3 cm has been widely accepted for standard breast fields but is not always applicable with more complex plans such as a three field technique or with modern techniques such IMRT and FIF approaches.
Historically, radiotherapy to the breast with Co-60 demonstrated a relative risk of 3.2 for cardiac effects. With newer techniques and the introduction of megavoltage beams this relative risk has likely decreased but radiotherapy has still been shown to increase cardiovascular mortality in breast radiation patients [Citation12–15]. Some review articles have also documented the cardiovascular toxicity in radiation treatment [Citation16,Citation17]. Although the effect of modern technology on this phenomenon has not been comprehensively studied, SEER data has shown increased cardiac mortality in long-term follow-up [Citation4,Citation18]. Correa et al. [Citation18] has shown an increased incidence of cardiac diagnostic test abnormalities in women irradiated to the left side and found a higher than predicted incidence of cardiovascular disease in the irradiated patient population. Patients with abnormal cardiac diagnostic test were also found to have larger median CLDs. It was found that at 10 years, women with left-sided breast cancer had an increased number of cardiac deaths [Citation4,Citation5]. However, women with right-sided breast cancers had an increased rate of non-cardiac deaths. Overall survival was not significantly different between left- or right-sided patients. It has also been theorized that patients who received a dose to the left ventricle of 25 Gy or greater were more likely to have perfusion changes on cardiac imaging.
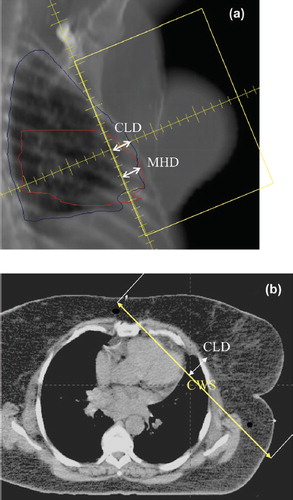
Most of the listed studies correlated the treatment sequelae of breast irradiation with tangential treatment parameters such as CLD, Chest wall separation (CWS), and maximum heart distance (MHD) as shown in . These simple parameters (CLD, CWS, MHD) correlate with the tissue volume in tangential fields. In general, the 2D metrics have not been correlated with modern complex treatment modalities, such as 3DCRT, FIF and IMRT. In a recent study, Teh et al. [Citation19] attempted to correlate dose-volume information (V10, V20, V30, V40) with clinical outcome. It was found that treatment parameters were weakly correlated with dose-volume. Radiation pneumonitis was demonstrated in< 1% in their population with 14.5 months of follow-up, however, the 2D parameters did not show any correlation to the heart volume.
With advances in imaging, modern breast treatments heavily depend on the computed tomography (CT)-based treatment planning where dose-volume histograms (DVH) are readily available with advanced dose calculation to account for inhomogeneity. Such information could be used to optimize treatment plans to reduce dose to the normal structures and is expected to play a pivotal role in the future for the understanding of radiation related sequelae. It is important, however, that these treatment parameters be correlated with the toxicity for those patients that have been treated 10–20 years ago and are being followed now. Due to long lag time in the detection of complications of the cardiac toxicity, such information is critical for the correlation which is attempted in this study. Lung and heart dose-volume were evaluated for possible correlation with 2D treatment parameters in external beam radiation therapy of the breast cancer. The goal of this study is to correlate older 2D parameters with more modern DVH parameters to allow ongoing follow-up/evaluation of patients treated many years ago and comparison with patients treated with modern planning.
Material and methods
With institutional review board (IRB) approval the records of 204 women treated at Indiana University Hospital for breast carcinoma via external beam irradiation using tangential or three-field breast techniques were identified. One hundred and thirty patients were excluded because their dosimetric data were not obtainable due to changes in our treatment planning system. Additionally, four patients were excluded because they were treated with partial breast irradiation. Seventy patients were subsequently available for analysis. All women included in our study were planned utilizing a Phillips Ultra-Z CT simulator in the spiral mode with 3 mm slice thickness. Radio-opaque wires were placed mid-sternum for the medial border, 1 cm below the clavicular head for the superior border, 2 cm below the inframammary fold for the inferior border, and in the mid-axilla for the lateral border. Most patients were immobilized either on a breast board or a vac-lock at an angle board, usually 10°. A monocentric technique was used for the treatment. The posterior aspect of the field was half beam blocked to provide a non-divergent beam edge to reduce dose to lung and heart as shown in a and b.
The Eclipse treatment planning system (Varian, Palo Alto, CA, USA) was used for patient treatment planning. The analytical anisotropic algorithm (AAA) inhomogeneity correction was used. Of the 70 women, 44 patients were treated for the left breast and 26 patients for the right breast. Typical prescribed dose was 1.8–2 Gy/fraction for a total dose of 48–54 Gy with 6 and/or 15 MV photons.
From the 70 patients, delineation of radiographic parameters was completed from the CT simulations. Documented for each patient was the total dose and maximum dose; V5, V10, and V20 for both the lung and heart using DVH; CLD (defined as the perpendicular distance from the posterior edge of the tangential field to the posterior part of the anterior chest wall in the middle of the field); CWS (defined as the non-divergent posterior field edge from the sternum to the lateral exterior aspect of the chest wall [Citation7,Citation9,Citation20]). The parameters V5, V10, V20 represent the volume of an organ receiving 5 Gy, 10 Gy and 20 Gy, respectively. For the patients treated tangentially to the left breast, the maximum heart distance, MHD, the maximum distance of the cardiac silhouette perpendicular to the longitudinal edge of the treatment field () were also measured. Correlation of dosimetric parameters, i.e., V5, V10 and V20 of heart and lung, with CLD, CWS and MHD was evaluated by linear regression and p-values are calculated for significance using statistical methods.
Results and discussion
The median CLD for the left and right lung were 1.86 cm± 0.62 cm and 1.59 ± 1.25 cm, respectively. The CLDs for the left breast were correlated with calculated V5, V10, V20 with correlation coefficients (R2) of 0.1155, 0.2862 and 0.3329 and p-values of 0.024, 0.002, and 0.0001, respectively. For the right lung the CLD, R2 values are 0.2228, 0.4007, 0.4529 and corresponding p-values are 0.015, 0.0005, 0.002 for V5, V10, V20, respectively. This shows that the CLD is directly correlated with the dose-volume—albeit a lower value of R2 but still the p-values are significant. A detail of the statistics (R2, p-value and confidence interval, CI) for left and right breast and heart is enclosed in . The correlation revealed that a simple parameter like CLD, acquired from any DRR or radiograph, may be correlated with complex variables such as 3D dose-volume. For the left breast the slope of the V5, V10 and V20 were nearly constant, 4.9 ± 0.4 cm suggesting that physical dimension and DVH were directly correlated. The slopes for right breast for V5-V20 ranged from 5.5–6.7 cm with an average of 6.2 ± 0.6 cm.
Table I. Statistical analysis of breast parameters.
The breast sequelae are associated with maximum dose in breast tissue. In our patient population with CWS in the range 16–35 cm, maximum dose was found to be directly correlated (R2= 0.4178, p= 0.001) with the size of the breast. This correlation indicates that for patients with large CWS, advance techniques like FIF and IMRT should be attempted from first place.
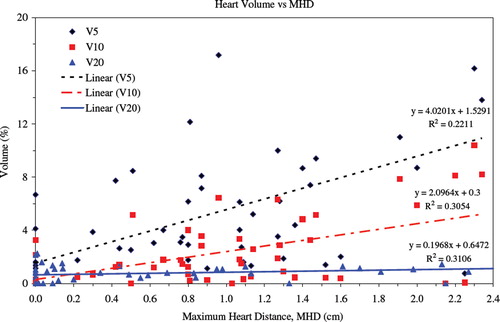
In our data, MHD ranged from 0–2.25 cm, with a mean of 0.9 cm. The median maximum heart distance was 0.89 ± 0.7 cm. The analysis for the heart DVH was reflected through the heart volume V5, V10, and V20 plotted versus MHD shown in . The regression coefficient r2 and corresponding p-values that are correlated with MHD for V5, V10, and V20 are 0.2209, 0.3058, 0.3102 and 0.0022, 0.0002, 0.0001, respectively. Note that the MHD of a few patients was measured to be zero, but a finite amount of radiation to the heart was found in these patients. This is probably due to scattered radiation and internal electrons that deposit dose. The magnitude of dose was dependent on the position of the heart from the beam edge. This prediction could not be derived from the physical width measurements; hence CT-based planning and evaluation of DVH was critical. Also there was no attempt for cardiac gating or respiratory motion management in the treatment of breast cancer that has shown to reduce lung and heart volumes.
Figure 2. Correlation of heart dose volume (V5, V10 and V20) to MHD. Data points are from treatment planning and lines are the linear regression with R2 values. The p-values are shown in .
Our study demonstrates that the correlation of treatment parameters (CLD, CWS, and MHD) provide a direct link to the volume of the lung and heart treated to a given dose. The literature documents a 0–29% range in the incidence of pneumonitis when treating breast cancer. This range is in part due to the older treatment techniques and in many studies, irradiation of the internal mammary lymph nodes [Citation21]. None of the patients in our study had the internal mammary chain treated. The parameter V20 has been widely used in the literature for estimation of lung complications, however newer data suggests that more stringent parameters of V10 and V5 should be used [Citation22]. In a retrospective study of 89 patients, Teh et al. [Citation19] attempted to correlate dose-volume information (V10, V20, V30, V40) with radiation pneumonitis. With a median follow-up of 4.5 months, only one patient developed steroid requiring radiation pneumonitis after six months with overall incidence of 1.1%. In another retrospective study of 353 patients, Minor et al. [Citation23] were also unable to find a correlation between CLD and pneumonitis and found only 1.2% pneumonitis even with> 3.0 cm CLD in 21.7% of the patients. Since 2D parameters are not directly related the observed toxicities, a direct correlation between volume and toxicity could resolve this issue.
Mean heart dose and biologically effective heart dose (BED) have also been found to be useful measures in the prediction of cardiac toxicity. Dose to the left coronary artery (LCA) has also been investigated as a predictor of toxicity. Taylor and colleagues [Citation24] found that LCA dose was a good predictor of mean heart dose, BED, and an approximate estimate of the mean dose to the left anterior descending artery (LAD). Taylor et al. [Citation24] described a strong correlation between MHD and mean heart dose (R2= 0.81); for every 1 cm of MHD the dose to the heart increased by 2.9%.
Borger et al. [Citation25] assessed the risk of cardio vascular disease (CVD) after adjuvant radiation in 1601 patients. With a median follow-up of 16 years, increasing MHD did not demonstrate a significant trend for increased CVD. Patients with a MHD> 3 cm did have a higher risk of ischemic cardiac events but these findings were not statistically significant [Citation25].
Our study shows correlations even though not strong but support the hypothesis nonetheless that MHD from 2D could be correlated to the observed complexity. The difference in observed complication and MHD has to do with scatter dose and sensitivity to cardiac structures. MHD demonstrated a correlation but increasing MHD did not show an increase in cardiac toxicities [Citation25]. Therefore, perhaps more strict parameters need to be identified. The V5, V10, V20 in relation to CLD and MHD may warrant further investigation.
Conclusions
The clinical outcome and the estimation of the radiation related sequelae are directly related to the dose and the volume of the tissue irradiated. Different studies have assessed parameters like pneumonitis and cardiac toxicities but have not demonstrated statistical significance. Breast radiation is increasing in complexity in terms of treatment techniques such as IMRT or accelerated partial breast irradiation. More concrete parameters would potentially allow adjuvant radiation to progress with an improvement in the toxicity profile. Using this retrospective analysis of 70 patients, it was concluded that the V5, V10, and V20 do correlate to the treatment parameters of CLD, CWS and MHD. The correlations are better for higher dose (V20) compared to V5 for all cases (). These correlations reinforce the importance of more stringent dose constraints to these structures and may help to limit toxicities in the individualization of treatment plans. This study also provides a link from 2D treatment parameter to 3D treatment parameters for the comparison of outcome in older study.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Fisher B, Anderson S, Bryant J, Margolese R, Deutsch M, Fisher E, . Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002;347:1233–41.
- Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, . Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002;347:1227–32.
- Darby S, McGale P, Correa C, Taylor C, Arriagada R, Clarke M, . Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: Meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 2011;378:1707–16.
- Darby SC, McGale P, Taylor CW, Peto R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: Prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol 2005;6:557–65.
- Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans E, . Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: An overview of the randomised trials. Lancet 2005;366:2087–106.
- Krengli M, Sacco M, Loi G, Masini L, Ferrante D, Gambaro G, . Pulmonary changes after radiotherapy for conservative treatment of breast cancer: A prospective study. Int J Radiat Oncol Biol Phys 2008;70:1460–7.
- Bornstein BA, Cheng CW, Rhodes LM, Rashid H, Stomper PC, Siddon RL, . Can simulation measurements be used to predict the irradiated volume in the tangential fields in patients treated for breast cancer? Int J Radiat Oncol Biol Phys 1990;18:181–7.
- Neal AJ, Yarnold JR. Estimating the volume of lung irradiated during tangential breast irradiation using the central lung distance. Br J Radiol 1995;68:1004–8.
- Das IJ, Cheng EC, Freedman G, Fowble B. Lung and heart dose volume analyses with CT simulator in radiation treatment of breast cancer. Int J Radiat Oncol Biol Phys 1998;42:11–9.
- Rotstein S, Lax I, Svane G. Influence of radiation therapy on the lung tissue in breast cancer patients: CT-assessed density changes and associated symptoms. Int J Radiat Oncol Biol Phys 1990;18:173–80.
- Lingos TI, Recht A, Vicini F, Abner A, Silver B, Harris JR. Radiation pneumonitis in breast cancer patients treated with conservative surgery and radiation therapy. Int J Radiation Oncol Biol Phys 1991;21:355–60.
- Rutqvist LE, Lax I, Fornander T, Johansson H. Cardiovascular mortality in randomized trail of adjuvant radiation therapy versus surgery alone in primary breast cancer. Int J Radiat Oncol Biol Phys 1992;22:887–96.
- Giordano SH, Kuo YF, Freeman JL, Buchholz TA, Hortobagyi GN, Goodwin JS. Risk of cardiac death after adjuvant radiotherapy for breast cancer. J Natl Cancer Inst 2005;97:419–24.
- Harris EE, Correa C, Hwang WT, Liao J, Litt HI, Ferrari VA, . Late cardiac mortality and morbidity in early-stage breast cancer patients after breast-conservation treatment. J Clin Oncol 2006;24:4100–6.
- Taylor CW, Nisbet A, McGale P, Goldman U, Darby SC, Hall P, . Cardiac doses from Swedish breast cancer radiotherapy since the 1950s. Radiother Oncol 2009;90:127–35.
- Darby SC, Cutter DJ, Boerma M, Constine LS, Fajardo LF, Kodama K, . Radiation-related heart disease: Current knowledge and future prospects. Int J Radiat Oncol Biol Phys 2010;76:656–65.
- Gagliardi G, Constine LS, Moiseenko V, Correa C, Pierce LJ, Allen AM, . Radiation dose-volume effects in the heart. Int J Radiat Oncol Biol Phys 2010;76:S77–85.
- Correa CR, Das IJ, Litt HI, Ferrari V, Hwang WT, Solin LJ, . Association between tangential beam treatment parameters and cardiac abnormalities after definitive radiation treatment for left-sided breast cancer. Int J Radiat Oncol Biol Phys 2008;72:508–16.
- Teh AYM, Park EJH, Shen L, Cheung HT. Three-demnsional volumentric analysis of irradiated lung with adjuvant breast irradiation. Int J Radiat Oncol Biol Phys 2009;75:1309–15.
- Das IJ, Cheng C-W, Fein DA, Fowble B. Patterns of dose variability in radiation prescription of breast cancer. Radiother Oncol 1997;44:83–9.
- Lind PAM, Marks LB, Hardenbergh PH, Clough R, Fan M, Hollis D, . Technical factors associated with radiation pneumonitis after local±regional radiation therapy for breast cancer. Int J Radiat Oncol Biol Phys 2002;52:137–43.
- Allen AM, Czerminska M, Janne PA, Sugarbaker DJ, Bueno R, Harris JR, . Fatal pneumonitis associated with intensity-modulated radiation therapy for mesothelioma. Int J Radiat Oncol Biol Phys 2006;65:640–5.
- Minor GI, Yashar CM, Spanos WJ, Jr., Jose BO, Silverman CL, Carrascosa LA, . The relationship of radiation pneumonitis to treated lung volume in breast conservation therapy. Breast J 2006;12:48–52.
- Taylor CW, Nisbet A, McGale P, Darby SC. Cardiac exposures in breast cancer radiotherapy: 1950s–1990s. Int J Radiat Oncol Biol Phys 2007;69:1484–95.
- Borger JH, Hooning MJ, Boersma LJ, Snijders-Keilholz A, Aleman BM, Lintzen E, . Cardiotoxic effects of tangential breast irradiation in early breast cancer patients: The role of irradiated heart volume. Int J Radiat Oncol Biol Phys 2007;69:1131–8.