Abstract
Background. Predictive models for swallowing dysfunction were developed previously and showed the potential of improved intensity-modulated radiotherapy to reduce the risk of swallowing dysfunction. Still the risk is high. The aim of this study was to determine the potential of swallowing-sparing (SW) intensity-modulated proton therapy (IMPT) in head and neck cancer (HNC) for reducing the risk of swallowing dysfunction relative to currently used photon therapy. Material and methods. Twenty-five patients with oropharyngeal (n = 21) and hypopharyngeal (n = 4) cancer received primary radiotherapy, including bilateral neck irradiation, using standard (ST) intensity-modulated photon therapy (IMRT). Prophylactic (54 Gy) and therapeutic (70 Gy) target volumes were defined. The dose to the parotid and submandibular glands was reduced as much as possible. Four additional radiotherapy plans were created for each patient: SW-IMRT, ST-IMPT, 3-beam SW-IMPT (3B-SW-IMPT) and 7-beam SW-IMPT (7B-SW-IMPT). All plans were optimized similarly, with additional attempts to spare the swallowing organs at risk (SWOARs) in the SW plans. Probabilities of swallowing dysfunction were calculated with recently developed predictive models. Results. All plans complied with standard HNC radiotherapy objectives. The mean parotid gland doses were similar for the ST and SW photon plans, but clearly lower in all IMPT plans (ipsilateral parotid gland ST-IMRT: 46 Gy, 7B-SW-IMPT: 29 Gy). The mean dose in the SWOARs was lowest with SW-IMPT, in particular with 7B-SW-IMPT (supraglottic larynx ST-IMRT: 60 Gy, 7B-SW-IMPT: 40 Gy). The observed dose reductions to the SWOARs translated into substantial overall reductions in normal tissue complication risks for different swallowing dysfunction endpoints. Compared with ST-IMRT, the risk of physician-rated grade 2–4 swallowing dysfunction was reduced on average by 8.8% (95% CI 6.5–11.1%) with SW-IMRT, and by 17.2% (95% CI: 12.7–21.7%) with 7B-SW-IMPT. Conclusion. SWOAR-sparing with proton therapy has the potential to substantially reduce the risk of swallowing dysfunction compared to similar treatment with photons.
Developments in radiation therapy techniques for head and neck cancer (HNC) patients, especially computer-optimized techniques such as intensity-modulated radiation therapy (IMRT), created new possibilities to reduce dose to organs at risk (OARs), thereby reducing radiation-induced side effects. For example, IMRT has been shown to significantly spare salivary glands, thereby reducing radiation-induced xerostomia [Citation1,Citation2]. In recent years, there has been growing interest in another important side effect of head and neck radiotherapy: swallowing dysfunction [Citation3,Citation4]. In previous studies attempts have been made to spare potential relevant swallowing OARs (SWOARs) [Citation4–6]. However, knowledge about which SWOARs were most relevant in relation to normal tissue complication was insufficient.
Our previous research focused on determining which SWOARs were most relevant in relation to radiation-induced swallowing dysfunction [Citation7]. This showed the importance of the mean dose to the superior pharyngeal constrictor muscle (PCM) and to the supraglottic larynx in predicting physician-rated RTOG grade 2–4 swallowing dysfunction at six months post-treatment [Citation7]. In addition, the mean dose to the middle PCM and the esophageal inlet muscle were important prognostic factors for various aspects of patient-rated swallowing problems after curative radiotherapy or chemoradiation. By limiting the dose to these structures – the most relevant SWOARs – the impact of treatment on quality of life could also be limited.
Additional dose constraints for SWOARs can be defined in radiotherapy treatment planning to reduce the dose to the most relevant SWOARs [Citation4,Citation5,Citation8]. We recently conducted an in silico planning comparative study which showed that the SWOARs could indeed be spared with IMRT without increasing the dose to parotid glands and without violating any other current planning objectives [Citation9]. These dose reductions to the SWOARs are expected to translate into reductions in the risk of physician- and patient-rated swallowing dysfunction [Citation7].
Due to their favorable physical properties, protons could be even more effective than photons – i.e. standard radiotherapy – for limiting the mean dose to OARs in the head and neck region [Citation10–12]. New generation proton delivery techniques such as intensity modulated proton therapy with pencil beam scanning (IMPT) have been introduced in clinical practice in recent years [Citation13]. It was already demonstrated that with IMPT the mean dose to the major salivary glands and the oral cavity could be significantly reduced in oropharyngeal cancer [Citation14,Citation15]. Until now, no attempts have been made to spare the SWOARs with protons and we hypothesized that with IMPT, the dose to the SWOARs could be further reduced as well.
Therefore, the research questions of the current in silico planning comparative study were: 1) Compared with IMRT, can the dose delivered to relevant SWOARs be reduced using IMPT, planned with a standard 3-beam and a more complex 7-beam setup? 2) What is the expected clinical benefit of this SWOAR-sparing? To answer these questions, we used recently developed predictive models [Citation7] for swallowing dysfunction.
Materials and methods
Patients and system data
The population of this study was composed of 25 patients who previously underwent primary radiotherapy or chemoradiation for oropharyngeal (n = 21) or hypopharyngeal (n = 4) cancer. Patients without dental metal artifacts who received bilateral neck irradiation were randomly selected from our previous cohort [Citation7]. Planning computed tomography (CT)-scans were acquired in supine position with a 2 mm slice thickness. Photon IMRT treatment planning was performed with the Pinnacle3 treatment planning system (version 9.1, Philips Radiation Oncology Systems, Fitchburg, WI, USA). Proton IMPT treatment planning was performed with the XiO treatment planning system (version 4.45, Elekta CMS Software GmbH, Freiburg, Germany).
Regions of interest
The planning target volumes (PTV) used in the present study were identical to those defined for the actual radiation therapy for each patient and included a uniform margin of 5 mm for position uncertainties. For each patient, two PTVs were defined: a prophylactic PTV, including the elective nodal areas on both sides of the neck with a prescribed total dose of 54.25 Gy (PTV54), and a therapeutic PTV with a prescribed total dose of 70 Gy (PTV70). The definition of the clinical target volumes was described previously in more detail [Citation15–17]. A simultaneous integrated boost technique was used consisting of 35 fractions, with a fraction dose of 1.55 Gy and 2.00 Gy prescribed to PTV54 and PTV70, respectively.
In addition to the SWOARs that were identified in our previous study [Citation7], critical structures (brainstem and spinal cord) and other OARs were outlined for the purpose of treatment planning and evaluation () [Citation18,Citation19]. No margins were used for OARs, except that for the critical structures a uniform 5 mm expansion was used only during treatment planning optimization.
Table 1. Volumes of interest and corresponding planning criteria.
IMRT and IMPT planning and optimization
For each patient, two 7-beam IMRT treatment plans were created: a standard IMRT plan (ST-IMRT), aimed at reducing the mean dose to the parotid and submandibular glands as much as possible without compromising the planning objectives with a higher priority (), and a second IMRT plan that was based on the ST-IMRT treatment plan with additional optimization aimed at reducing the radiation dose to the SWOARs (SW-IMRT) [Citation9]. All plans were created based on the objectives and planning priorities as specified in . In a similar fashion, ST-IMPT and SW-IMPT treatment plans were created for each patient: 1) a standard IMPT plan with a 3-beam setup (ST-IMPT); 2) a SW-IMPT plan with a 3-beam setup (3B-SW-IMPT); and 3) a SW-IMPT plan with a 7-beam setup (7B-SW-IMPT). The 3-beam plans used gantry angles of 50°, 180° and 310°. The 7-beam plans used gantry angles of 50°, 100°, 150°, 180°, 210°, 260° and 310° or, depending on the shape of the target volume and the position of the shoulders, 30°, 80°, 130°, 180°, 230°, 280° and 330°. Each beam was set to distribute spots throughout the PTVs and no further than 1 cm outside PTV54. Spots were distributed over the target volume with a 5 mm separation in the plane perpendicular to the beam direction; in depth, spot layers were positioned such that the 80% level of the Bragg peaks matched. The final average spot size (ς at the Bragg peak), taking into account degradation by the range shifter, the air gap and the patient, ranged from 6 to 8 mm for energies from 84 to 230 MeV. The ultimate planning objectives and planning priorities of IMRT and IMPT were similar (), however, the optimization parameter values and weights were adjusted in a trial-and-error adaptive fashion, with both IMRT and IMPT, until a satisfactory plan was finally obtained.
Dose-volume data and normal tissue complication probability evaluation
Target coverage, and various dose-volume parameters () were evaluated. Multivariate regression models for different swallowing dysfunction endpoints [Citation7] were used to calculate the normal tissue complication probability (NTCP) values for each plan regarding: 1) physician-rated RTOG grade 2–4 swallowing dysfunction [Citation20]; 2) patient-rated moderate to severe problems with swallowing of solid, soft and liquid food; and 3) patient-rated choking when swallowing. Probabilities were calculated for each patient by simulating two options for age (18–65 vs. > 65 years). The patient-rated problems correspond to moderate to severe problems as assessed with the EORTC QLQ-H&N35 questionnaire [Citation7,Citation21].
Results
Primary objectives and irradiated volumes
For each case, target coverage was always within the predefined constraints, and the dose in the critical structures (brainstem and spinal cord) and the maximum plan dose were always within limits ( and ). The values for V5 Gy – V51.5 Gy within the patient outline (representing the volume receiving a low-to-intermediate dose), and the integral dose (mean dose within patient outline × patient outline volume) were substantially smaller with the IMPT plans (). The V58 Gy (the volume receiving ≥ 107% of the prescribed prophylactic dose) was the only parameter that was larger with IMPT. Sparing of SWOARs with IMRT resulted in somewhat larger V51.5 Gy to V66.5 Gy volumes, indicating a worsening of the target dose conformity. This increase was not observed when SWOARs were spared with IMPT.
Table 2. Dose-volume results of relevant structures and corresponding NTCP values for swallowing dysfunction.
Dose delivered to OARs and SWOARs
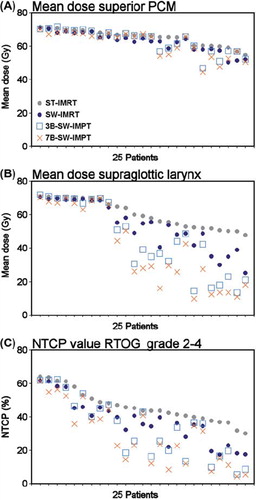
Salivary gland doses were lowest with the IMPT plans (). For both IMRT and IMPT, sparing of SWOARs did not result in increased parotid dose. Overlap with the PTV hampered sparing of the submandibular glands in most patients. Both the ST-IMRT and ST-IMPT plans resulted in fairly similar dose parameter values for the SWOARs (). SW-IMPT generally resulted in lower SWOAR mean dose values than SW-IMRT. As most patients had oropharyngeal cancers, the PTVs overlapped considerably with the superior PCM and the middle PCM in the majority of cases, and allowed for only marginal sparing of these structures (). With IMRT – but even more with 3B-SW-IMPT and especially with 7B-SW-IMPT – larger reductions of the mean supraglottic larynx dose were obtained (). Compared to ST-IMRT, the mean dose to the supraglottic larynx was reduced by 6.9 Gy (95% CI 4.1–9.7 Gy) with SW-IMRT, by 14.6 Gy (95% CI 8.9–20.2 Gy) with 3B-SW-IMPT and by 20.0 Gy (95% CI 13.5–26.4 Gy) with 7B-SW-IMPT. Due to the variable location of the SWOARs relative to the PTVs, the potential of protons to spare the SWOARs differed considerably among individual patients (). As the esophagus inlet muscle was often near the PTV, in most patients the V60 Gy of the esophageal inlet muscle could not be improved with the various radiotherapy techniques.
Figure 1. Sagittal and axial representation of dose distributions with standard (ST)-intensity-modulated radiotherapy (IMRT), swallowing-sparing (SW)-IMRT and 7-beam SW-intensity-modulated proton therapy (IMPT) in a sample patient.
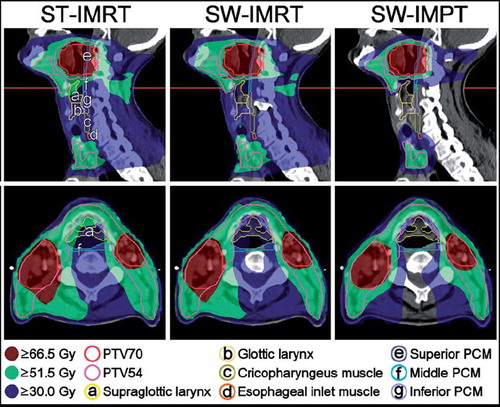
Figure 2. Mean dose delivered to the superior pharyngeal constrictor muscle (PCM) (A) and supraglottic larynx (B), and corresponding normal tissue complication probability (NTCP) of physician-rated RTOG grade 2–4 swallowing dysfunction (C) with standard (ST)-intensity-modulated radiotherapy (IMRT), swallowing-sparing (SW)-IMRT and SW-intensity-modulated proton therapy (IMPT). In each figure, patients were re-sorted according to the corresponding value with ST-IMRT.
NTCP of swallowing dysfunction
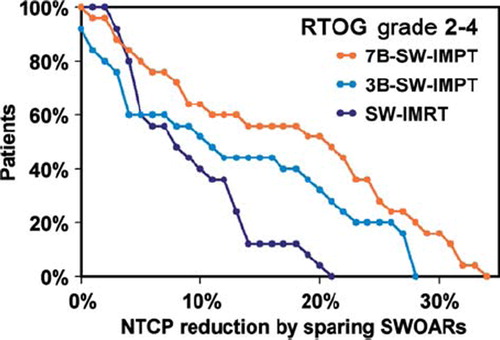
SWOAR dose reductions obtained with swallowing-sparing IMRT and IMPT resulted in reduced NTCP values for swallowing dysfunction (). Compared to ST-IMRT, on average the probability of physician-rated RTOG grade 2–4 swallowing dysfunction was reduced by 8.8% (95% CI 6.5–11.1%) with SW-IMRT, by 12.5% (95% CI 8.1–16.8%) with 3B-SW-IMPT and by 17.2% (95% CI 12.7–21.7%) with 7B-SW-IMPT ( and ). The results clearly show that not all patients are expected to benefit from SW-IMPT (). Patient-rated moderate to severe problems with solid and soft food depended not only on the dose in the SWOARs, but also on age [Citation7]; these risks were highest in patients aged > 65 years. The NTCP-value reductions were largest for the probability of problems with solid food. More specifically, compared with ST-IMRT and assuming patients were aged > 65 years, on average the probability of problems with solid food would be reduced by 10.0% (95% CI 7.2–12.7%) with SW-IMRT, by 14.8% (95% CI 9.7–19.9%) with 3B- SW-IMPT and by 19.9% (95% CI 14.6–25.2%) with 7B-SW-IMPT (). For patient-rated moderate to severe problems with swallowing soft food and liquids and moderate to severe choking when swallowing, the initial NTCP values were lower, and similar values were predicted for both SW-IMRT and SW-IMPT ().
Figure 3. Calculated normal tissue complication probability (NTCP) values of physician-rated RTOG grade 2–4 swallowing dysfunction in a patient with a considerable benefit. According to our models [Citation7], the NTCP with standard (ST)-intensity-modulated radiotherapy (IMRT), swallowing-sparing (SW)-IMRT and SW-intensity-modulated proton therapy with 7 beams (7B-SW-IMPT) depends not only on the mean dose to the superior pharyngeal constrictor muscle (PCM), but also on the mean dose to the supraglottic larynx region.
![Figure 3. Calculated normal tissue complication probability (NTCP) values of physician-rated RTOG grade 2–4 swallowing dysfunction in a patient with a considerable benefit. According to our models [Citation7], the NTCP with standard (ST)-intensity-modulated radiotherapy (IMRT), swallowing-sparing (SW)-IMRT and SW-intensity-modulated proton therapy with 7 beams (7B-SW-IMPT) depends not only on the mean dose to the superior pharyngeal constrictor muscle (PCM), but also on the mean dose to the supraglottic larynx region.](/cms/asset/e6ee7417-ecb6-4a4f-a75e-e7fe87234fe7/ionc_a_692885_f0003_b.jpg)
Figure 4. Potential reductions in the normal tissue complication probability (NTCP) of physician-rated RTOG grade 2–4 swallowing dysfunction as achieved by swallowing-sparing intensity-modulated radiotherapy (SW-IMRT) or intensity-modulated proton therapy with 3 or 7 beams (3B-SW-IMPT and 7B-SW-IMPT, respectively) relative to standard (ST)-IMRT. Cumulative plots are shown.
Discussion
This in silico planning comparative study demonstrated that the dose to SWOARs can be reduced with IMPT relative to IMRT. The lowest SWOARs doses were obtained with 7B-SW-IMPT. Relative to ST-IMRT, the mean dose in the superior PCM was reduced from on average 65 Gy to 62 Gy, in the middle PCM from 63 Gy to 57 Gy and in the supraglottic larynx from 60 Gy to 40 Gy. According to predictive models recently developed at our department [Citation7], these SWOAR dose reductions translated into a clinical benefit in terms of reduced probabilities of physician-rated RTOG grade 2–4 swallowing dysfunction and patient-rated swallowing problems. The NTCP of RTOG grade 2–4 swallowing dysfunction could be reduced from on average 46% to 29%.
The SWOAR dose reductions were obtained without compromising the initial objectives of the ST-IMRT and ST-IMPT plans. However, when attempts were made to spare the SWOARS with IMRT, the V51.5 Gy increased, indicating that with IMRT the dose distribution became slightly less conformal to PTV54. This did not occur when SWOARs were spared with IMPT. The results indicate that IMPT allows for better sparing of the salivary glands and SWOARs while smaller volumes receive low-to-intermediate doses.
The amount of potential swallowing-sparing varied between individual patients. This was influenced by varying patient anatomy and tumor extension, since differences in overlap between the PTV and a specific SWOAR may result in different possibilities for sparing the SWOARs. When there was a large or full overlap, in some patients IMPT dose values could even be slightly higher than IMRT values ( and ). In this study, most tumors were oropharyngeal cancers and therefore the PTVs often overlapped with the superior PCM, which hampered further dose reduction to this structure. In contrast, the supraglottic larynx was located more inferiorly and remotely from the tumor, resulting in substantially larger dose reductions. The options to spare the SWOARS may depend on the primary tumor site. We selected 165 consecutive HNC patients receiving primary radiotherapy at our department to study the overlap between the SWOARs and the PTV. Fifty of these patients had a laryngeal tumor with on average 19% of the superior PCM overlapping with the PTV and on average 71% of the supraglottic larynx overlapping with the PTV. Forty-nine patients had an oropharyngeal tumor, with on average 76% and 43% overlap, respectively. This shows that it depends on the primary tumor site which SWOARs can potentially be spared. In the case of the NTCP of RTOG grade 2–4 swallowing dysfunction, reductions can be obtained by reducing the dose in the superior PCM but also by reducing the dose in the supraglottic larynx [Citation7]. In the current study, NTCP reductions were mainly obtained by reducing the dose in the supraglottic larynx, whereas patients with laryngeal tumors are expected to benefit more from dose reductions in the superior PCM. In the current study, we only selected patients who received bilateral neck irradiation, because sparing of SWOARs seemed most challenging in these patients. As a result, the current study population includes a higher percentage of patients with more advanced T-stages (T3 and T4 tumors) and more advanced N-stages compared to the cohort of our previous study [Citation7]. Therefore, SWOAR sparing as well as parotid sparing was more difficult in the current population due to the generally larger target volumes and because most patients had a relatively large overlap between the target volumes, the parotid glands and the SWOARs.
Other investigators have analyzed the potential dosimetric gain of SWOAR-sparing with IMRT [Citation4–6,Citation8,Citation22,Citation23]. In most of these studies, the doses to the inferior SWOARs, such as the larynx and the inferior PCM, could be reduced with split-field IMRT, using specific blocking of the larynx in an anterior low-neck field that reduces the dose in the inferior SWOARs, but may also result in inadequate coverage of the caudal prophylactic PTV. In the current study, we demonstrated that SWOAR-sparing can be achieved without compromising PTV coverage.
Eisbruch et al. (2004) demonstrated that additional IMRT objectives for sparing the PCM and larynx could reduce the V50 Gy of these structures by 10% and 7%, respectively, compared to regular IMRT with similar target coverage [Citation4]. In that study, the doses to the PCM and larynx were related to abnormalities observed with video fluoroscopy (VF), direct endoscopy and CT, but the clinical relevance of the observed V50 Gy reductions could not be established. In a more recent study, Eisbruch et al. [Citation23] found for increased VF-based aspirations and worsened VF summary scores toxic doses (TDs)50 (Total Dose causing 50% toxicity) and TD25 of 63 Gy and 56 Gy for the whole PCM and 56 Gy and 39 Gy for the whole larynx, respectively. According to these mean dose based PCM and larynx models, 7-beam SW-IMPT would reduce the probability of the two VF-based endpoints from 35.5% to 27.7% and from 43.2% to 28.2%, respectively, relative to SW-IMRT. Incidence of observer rated grade ≥ 2 in the patient cohort considered by Eisbruch et al. (15) was much lower than in the present study due to the different selection of patients, different inclusion of nodal regions and the use of another toxicity grading system (being unable to take solid food normally gives a grade 1 according to CTCAEV3.0 vs. a grade 2 according to RTOG).
Although the current treatment planning study indicates that IMPT has the potential to reduce the probability of swallowing dysfunction relative to that with IMRT, clinical validation studies will be required to confirm that calculated dose reductions to SWOARs with photon therapy, and especially with proton therapy, actually result in the estimated NTCP reductions.
The results of the current study should be regarded as hypothesis generating for future clinical trials, e.g. to clinically validate the expected risk reductions in swallowing dysfunction. A number of issues may hamper proton therapy in head and neck cancer. First, IMPT is expected to be more sensitive to density heterogeneity changes, caused by anatomic or geometric changes in the patient during treatment than IMRT [Citation24,Citation25]. Any clinical application of IMPT should therefore be accompanied by image guidance, well-defined setup correction protocols and adaptive strategies when necessary. In the present study, similar PTV margins and optimization methods were used for IMRT and IMPT. However, a number of methods have been proposed to improve the robustness of proton plans, such as probabilistic planning methods which take into account various error scenarios during optimization. Other methods to account for these sources of error are the reduction of in-field dose gradients, the manipulation of optimization starting conditions and the application of beam-specific PTV margins may improve proton plan robustness [Citation26]. Each of these methods may yield different results and may either increase or decrease the dose in the SWOARs with proton therapy. Further studies will be performed in our institute to establish the actual influence of these methods on the SWOAR-sparing capabilities of IMPT.
Compared to 3B-SW-IMPT, 7B-SW-IMPT further reduced swallowing dysfunction. This leads to the question: which beam geometry would be best to use in HNC patients? It was previously demonstrated that 3-, 5- and 9-beam IMPT setups resulted in similar target dose homogeneity and parotid gland sparing [Citation27]. However, in that study, no high-risk dose (boost) region was considered and no efforts were made to spare SWOARs. The results of the current study indicate that, when taking into account multiple OARs, the number of beams (additional gantry angles) are indeed important because this increases the degrees of freedom to spare OARs, while simultaneously maintaining adequate target coverage.
In conclusion, compared to swallowing-sparing IMRT, swallowing-sparing IMPT can potentially provide a substantial reduction of the mean dose to the SWOARs. Moreover, IMPT improved salivary gland sparing. Compared with 3-beam SW-IMPT, the 7-beam SW-IMPT allowed for the largest SWOAR dose reductions. Recently developed models for physician-rated and patient-rated swallowing dysfunction indicate that these SWOAR dose reductions translate into a reduced probability of swallowing dysfunction and may therefore limit the impact of treatment on quality of life. The largest reductions in swallowing dysfunction were predicted for 7-beam SW-IMPT. These outcomes must be confirmed in clinical validation studies in which swallowing function is scored in HNC patients who are actually treated with swallowing-sparing proton therapy.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Vergeer MR, Doornaert PA, Rietveld DH, Leemans CR, Slotman BJ, Langendijk JA. Intensity-modulated radiotherapy reduces radiation-induced morbidity and improves health-related quality of life: Results of a nonrandomized prospective study using a standardized follow-up program. Int J Radiat Oncol Biol Phys 2009;74:1–8.
- Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, Leemans CR, Aaronson NK, Slotman BJ. Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol 2008;26:3770–6.
- Jensen K, Lambertsen K, Grau C. Late swallowing dysfunction and dysphagia after radiotherapy for pharynx cancer: Frequency, intensity and correlation with dose and volume parameters. Radiother Oncol 2007;85:74–82.
- Eisbruch A, Schwartz M, Rasch C, Vineberg K, Damen E, Van As CJ, . Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: Which anatomic structures are affected and can they be spared by IMRT? Int J Radiat Oncol Biol Phys 2004;60:1425–39.
- Caudell JJ, Burnett OL III, Schaner PE, Bonner JA, Duan J. Comparison of methods to reduce dose to swallowing-related structures in head and neck cancer. Int J Radiat Oncol Biol Phys 2010;77:462–7.
- Webster GJ, Rowbottom CG, Ho KF, Slevin NJ, Mackay RI. Evaluation of larynx-sparing techniques with IMRT when treating the head and neck. Int J Radiat Oncol Biol Phys 2008;72:617–22.
- Christianen MEMC, Schilstra C, Beetz I, Muijs CT, Chouvalova O, Burlage FR, . Predictive modelling for swallowing dysfunction after primary (chemo)radiation: Results of a prospective observational study. Radiother Oncol 2011 (in press) doi: 10.1016/j.radonc.2011.08.009.
- Fua TF, Corry J, Milner AD, Cramb J, Walsham SF, Peters LJ. Intensity-modulated radiotherapy for nasopharyngeal carcinoma: Clinical correlation of dose to the pharyngo-esophageal axis and dysphagia. Int J Radiat Oncol Biol Phys 2007;67:976–81.
- van der Laan HP, Christianen MEMC, Bijl HP, Schilstra C, Langendijk JA. The potential benefit of swallowing sparing intensity-modulated radiotherapy to reduce swallowing dysfunction: An in silico planning comparative study. 2012;103: 76–81.
- van de Water TA, Bijl HP, Schilstra C, Pijls-Johannesma M, Langendijk JA. The potential benefit of radiotherapy with protons in head and neck cancer with respect to normal tissue sparing: A systematic review of literature. Oncologist 2011;16:366–77.
- Ask A, Bjork-Eriksson T, Zackrisson B, Blomquist E, Glimelius B. The potential of proton beam radiation therapy in head and neck cancer. Acta Oncol 2005;44:876–80.
- Mendenhall NP, Malyapa RS, Su Z, Yeung D, Mendenhall WM, Li Z. Proton therapy for head and neck cancer: Rationale, potential indications, practical considerations, and current clinical evidence. Acta Oncol 2011;50:763–71.
- Schippers JM, Lomax AJ. Emerging technologies in proton therapy. Acta Oncol 2011;50:838–50.
- van de Water TA, Lomax AJ, Bijl HP, Schilstra C, Hug EB, Langendijk JA. Using a reduced spot size for intensity-modulated proton therapy potentially improves salivary gland-sparing in oropharyngeal cancer. Int J Radiat Oncol Biol Phys 2012;82:e313–9.
- van de Water TA, Lomax AJ, Bijl HP, de Jong ME, Schilstra C, Hug EB, . Potential benefits of scanned intensity-modulated proton therapy versus advanced photon therapy with regard to sparing of the salivary glands in oropharyngeal cancer. Int J Radiat Oncol Biol Phys 2011;79:1216–24.
- Gregoire V, Eisbruch A, Hamoir M, Levendag P. Proposal for the delineation of the nodal CTV in the node-positive and the post-operative neck. Radiother Oncol 2006;79: 15–20.
- Gregoire V, Levendag P, Ang KK, Bernier J, Braaksma M, Budach V, . CT-based delineation of lymph node levels and related CTVs in the node-negative neck: DAHANCA, EORTC, GORTEC, NCIC,RTOG consensus guidelines. Radiother Oncol 2003;69:227–36.
- van de Water TA, Bijl HP, Westerlaan HE, Langendijk JA. Delineation guidelines for organs at risk involved in radiation-induced salivary dysfunction and xerostomia. Radiother Oncol 2009;93:545–52.
- Christianen MEMC, Langendijk JA, Westerlaan HE, van de Water TA, Bijl HP. Delineation of organs at risk involved in swallowing for radiotherapy treatment planning. Radiother Oncol 2011;101:394–402.
- Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995;31:1341–6.
- Bjordal K, Hammerlid E, Ahlner-Elmqvist M, de Graeff A, Boysen M, Evensen JF, . Quality of life in head and neck cancer patients: Validation of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-H&N35. J Clin Oncol 1999;17:1008–19.
- Schwartz DL, Hutcheson K, Barringer D, Tucker SL, Kies M, Holsinger FC, . Candidate dosimetric predictors of long-term swallowing dysfunction after oropharyngeal intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 2010;78:1356–65.
- Eisbruch A, Kim HM, Feng FY, Lyden TH, Haxer MJ, Feng M, . Chemo-IMRT of oropharyngeal cancer aiming to reduce dysphagia: Swallowing organs late complication probabilities and dosimetric correlates. Int J Radiat Oncol Biol Phys 2011;81:e93–9.
- Lomax AJ. Intensity modulated proton therapy and its sensitivity to treatment uncertainties 1: The potential effects of calculational uncertainties. Phys Med Biol 2008;53: 1027–42.
- Lomax AJ. Intensity modulated proton therapy and its sensitivity to treatment uncertainties 2: The potential effects of inter-fraction and inter-field motions. Phys Med Biol 2008;53: 1043–56.
- Park PC, Zhu XR, Lee AK, Sahoo N, Melancon AD, Zhang L, . A beam-specific planning target volume (PTV) design for proton therapy to account for setup and range uncertainties. Int J Radiat Oncol Biol Phys 2012;82: e329–36.
- Steneker M, Lomax A, Schneider U. Intensity modulated photon and proton therapy for the treatment of head and neck tumors. Radiother Oncol 2006;80:263–7.