To the Editor,
The number of newly diagnosed patients with high grade malignant glioma (WHO grade III–IV [Citation1]) in Sweden is approximately 400 per year. These tumours belong to the most devastating oncologic diseases with a median survival of glioblastoma (WHO grade IV) of only a few months among elderly patients (≥ 65–70 years of age) [Citation2,Citation3]. In 1993, the Swedish National CNS-tumour Group was founded, and in 1999 the group initiated a Swedish National Brain Tumour Registry committed to providing a resource for gathering and disseminating epidemiologic data on all primary brain tumours. Only a decade ago, patients 60 years of age were regarded as ‘poor risk’ and therefore infrequently considered as candidates for radical surgery and radio-chemotherapy [Citation4]. In addition, population-based data from European cancer registries over the period 1988–2002 did not show any improvement in survival [Citation5], which is somewhat discouraging. Since then, however, some important studies have defined a more active therapeutic approach [Citation2,Citation3,Citation6,Citation7]. Here we report on a selection of data from a more recent time period, 1999–2009, from the population-based Swedish National Brain Tumour Registry based on the three regions in Sweden, which have a registration compliance of almost 100%. The objective of this report is to illustrate that an unselected patient population of high grade malignant glioma of age ≥ 60 may benefit significantly from development in medical care.
Methods
We analysed data reported from the regions with the most active registration during the period 1999–2009, and the patient coverage was between 94% and 100%. It was calculated as the percentage of diagnoses in the Swedish National Brain Tumour Registry of corresponding diagnoses recorded in the Swedish Cancer Registry during the same period, and included 1844 patients, of which 1037 patients were 60–84 years of age and 587 patients 60–69 years of age. Survival data for patients 60–84 years of age with high grade malignant gliomas, i.e. glioblastoma (WHO grade IV), anaplastic astrocytoma (WHO grade III) and anaplastic oligodendroglial tumours (grade III), was collected from three health care regions with the most active registration in Sweden; the Northern region, the Uppsala region and the South-east region. The choice of these specific regions was governed only by registration activity, and we have no reasons to assume that this population differs from the rest of the Swedish patient population. The included regions represented 45% of the population in Sweden as in 2007. By delimiting the diagnoses to a maximum of 84 years of age, less of the diagnoses should be diluted by patients with extremely poor prognosis irrespective of treatment.
All patients were followed until death or at latest 30 June 2010. Eight patients were lost to follow-up due to emigration and were censured at the date of emigration.
The investigated time periods were 1999–2003, 2004–2006 and 2007–2009 (referring to the year of pathologic diagnosis for each patient).
Survival was estimated from Kaplan-Meier survival curves, and a log-rank test was performed to assess whether the survival curves differed. Cox regression was performed to estimate the hazard ratio between years of diagnosis adjusted for sex and age group. The analysis restricted to ages 60–69 was adjusted for age groups 60–64, 65–69 and the analysis restricted to ages 60–84 was adjusted for age groups 60–64, 65–69, 70–74, 75–79, 80–84. All analysis on survival is based on all cause survival.
Results
For patients diagnosed between 60 and 69 years of age almost a doubling of the median survival has occurred during the last decade The median survival has increased from 5.8 months (95% CI 5.1–7.5) 1999–2003 to 8.5 months (95% CI 7.0–10.3) 2004–2006 and to 10.5 months (95% CI 9.0–12.6) 2007–2009 (). The hazard ratio estimated with Cox-regression and adjusted for sex and age group was 0.74 (95% CI 0.60–0.91) 2004–2006 compared with 1999–2003, based on two years of follow-up. The corresponding hazard ratio between 2007–2009 and 1999–2003 was 0.56 (95% CI 0.44–0.72).
Figure 1A and B. Two year survival for patients 60–69 years (A) and 60–84 years (B) with high grade malignant gliomas for the Northern region, Uppsala-Örebro region and the South-east region.
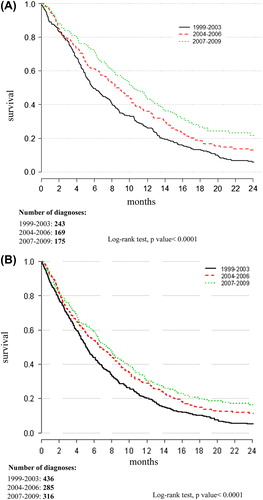
For patients diagnosed between 60 and 84 years of age, the median survival was 5.1 months (95% CI 4.6–5.8) 1999–2003, 6.7 months (95% CI 5.5–8.2) 2004–2006 and 7.5 months (95% CI 6.4–8.4) 2007–2009 (). The hazard ratio estimated with Cox-regression and adjusted for sex and age was 0.79 (95% CI 0.68–0.93) 2004–2006 compared with 1999–2003. The corresponding estimate between 2007–2009 and 1999–2003 was 0.69 (95% CI 0.58–0.82).
Discussion
A few main features characterize the development of treatment strategies for patients with high grade malignant gliomas during the last decade. A breakthrough was the employment of concomitant radio-chemotherapy which, after data of its superiority for glioblastoma was published in 2005 [Citation7] became accepted as clinical routine in the oncological community. The surgical technique has improved during the period by the more widespread use of the operation microscope, neuronavigation and functional MRI [Citation8,Citation9] which makes a more aggressive and radical surgery possible while sparing surrounding tissue. The introduction of 3D conformal dose planning techniques in radiotherapy has facilitated higher therapeutic doses to the tumour and an improved therapeutic ratio [Citation10]. Our observations of a considerable improvement in survival in patients in the age group of 60–84 years, based on data from the Swedish National Population-based Brain Tumour Registry, illustrate that this development has also served the older patient group. In particular, patients aged 60–69 years seem to have had the greatest benefit from advances in medical care. The reasons for this could be that this age group, in comparison with the age group of 60–84, is more resistant to complications or side effects of therapy, that the risk of death of other causes than high grade glioma is lower or possibly that the tumours of these patients are more sensitive to treatment due to differences in biological tumour characteristics [Citation11,Citation12].
The term median survival as it is used in this context requires a strictly defined date of diagnosis, and is consistently in this registry the date of the signed pathology report, which is of the utmost importance for diseases such as high grade glioma, where the expected remaining survival time is short.
We believe that our findings could increase the awareness of the value of an active treatment approach among clinicians, researchers and the community to dedicate resources to these previously more or less neglected patients.
The registration of data of diagnostic methods and different treatment strategies are underway but still immature. Nevertheless, we may assume that a national population-based registry, with close to 100% registration compliance for important diagnostic and outcome parameters and open publication of data, is an efficient instrument for the evaluation of quality measures and implementation of new therapeutic strategies [Citation13]. In the pace of the exponential development of cancer treatments, a high quality registry will probably be of increasing importance for our cancer patients.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
This work has been supported by funding from the Swedish national and local cancer research foundations.
References
- Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 2007;114:97–109.
- Malmstrom A, Gronberg BH, Marosi C, Stupp R, Frappaz D, Schultz H, et al. Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: The Nordic randomised, phase 3 trial. Lancet Oncol 2012;13:916–26.
- Wick W, Platten M, Meisner C, Felsberg J, Tabatabai G, Simon M, et al. Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: The NOA-08 randomised, phase 3 trial. Lancet Oncol 2012; 13:707–15.
- Laws ER, Parney IF, Huang W, Anderson F, Morris AM, Asher A, et al. Survival following surgery and prognostic factors for recently diagnosed malignant glioma: Data from the Glioma Outcomes Project. J Neurosurg 2003;99:467–73.
- Sant M, Minicozzi P, Lagorio S, Johannesen TB, Marcos-Gragera R, Francisci S. Survival of European patients with central nervous system tumors. Int J Cancer 2011;131: 173–85.
- Keime-Guibert F, Chinot O, Taillandier L, Cartalat-Carel S, Frenay M, Kantor G, et al. Radiotherapy for glioblastoma in the elderly. N Engl J Med 2007;356:1527–35.
- Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 2005; 352:987–96.
- Hsieh JC, Lesniak MS. Surgical management of high-grade gliomas. Expert Rev Neurother 2005;5(6 Suppl):S33–9.
- Sanai N, Berger MS. Operative techniques for gliomas and the value of extent of resection. Neurotherapeutics 2009; 6:478–86.
- Stieber VW, Mehta MP. Advances in radiation therapy for brain tumors. Neurol Clin 2007;25:1005–33, ix.
- Weller M, Platten M, Roth P, Wick W. Geriatric neoro- oncology: From myth to biology. Curr Opin Neurol 2011;24: 599–604.
- Wick W, Hartmann C, Engel C, Stoffels M, Felsberg J, Stockhammer F, et al. NOA-4 Randomized phase III trial of sequential radiochemotherapy of anaplastic glioma with procarbazine, lomustine, and vincriustine or temozolomide. J Clin Oncol 2009;27:5874–80.
- Holmberg LH. Can national cancer registration support clinical databases and clinical cancer research? Acta Oncol 2012;51:691–3.