Abstract
Patients with haematological malignancies are at increased risk of experiencing work-related problems. The aims of this study were to compare the risk of disability pension (DP) among patients diagnosed with eight subtypes of haematological malignancies to a reference cohort, and to determine if relative risks differ between these subtypes; to evaluate the influence of socioeconomic factors, demographic factors, and clinical factors on the risk of DP; and to investigate if these associations differ between the reference cohort and the patient cohort.
Material and methods. We combined data from national registers on Danish patients diagnosed with haematological malignancies between 2000 and 2007 and a reference cohort without a history of these diseases. A total of 3194 patients and 28 627 reference individuals were followed until DP, emigration, old age pension or anticipatory pension, death or 26 February 2012, whichever came first.
Results. A total of 550 (17%) patients and 1511 (5%) reference individuals were granted DP. Age- and gender-adjusted relative risks differed significantly between the subgroups of haematological malignancies and ranged from 2.64 (95% CI 1.84–3.78) for patients with Hodgkin lymphoma to 12.53 (95% CI 10.57–14.85) for patients with multiple myeloma. In the patient cohort we found that gender, age, comorbidity, ethnicity, educational level, household income, history of long-term sick leave, and need of treatment with anxiolytics or antidepressants after diagnosis were associated with receiving DP. However, most of these associations were stronger in the reference cohort.
Conclusion. All eight subtypes of haematological malignancies were associated with an increased risk of DP compared to the reference cohort. The relative risks differed according to subtype, and patients with multiple myeloma had the highest risk of DP. Furthermore, most socioeconomic, demographic and clinical factors had a stronger impact on the risk of DP in the reference cohort than in the patient cohort.
More than one third of patients diagnosed with haematological malignancies are between 20 and 64 years of age. Previous studies have documented that these patients are at increased risk of experiencing work-related problems compared to cancer-free control groups [Citation1–3] and patients with other cancer types [Citation4–7].
Denmark has a widespread tax-financed welfare system and it is thus possible for persons with permanently reduced work capacity to retire due to their disability and be financially compensated. A Danish cohort study showed that patients with leukaemia had a three-fold risk and patients with non-Hodgkin lymphoma a two-fold risk of disability pension compared to cancer-free controls [Citation1]. However, in this study haematological malignancies with very different treatment regimens and prognoses were pooled, and a recent study on return to work after long-term sick leave for patients diagnosed with haematological malignancies found that return to work was highly dependent on the type of haematological malignancy [Citation8]. To the best of our knowledge, no studies have investigated the risk of permanently reduced work capacity in patients with haematological malignancies divided into clinically relevant subtypes in comparison to a reference cohort without these types of malignancies.
It is well known, that, for example high age, low socioeconomic status and comorbidity are risk factors for receiving disability pension in the general population [Citation9], however, documentation on factors possibly associated with increased risk of permanently reduced work capacity among patients with haematological malignancies is scarce [Citation10].
Therefore the present study aimed to: 1) Compare the risk of disability pension (DP) among patients diagnosed with eight clinically relevant subtypes of haematological malignancies to an age- and gender-matched reference cohort without a history of these malignancies, and to determine if relative risks differ between these subtypes; 2) Evaluate the influence of socioeconomic factors, demographic factors, comorbidity, and post-diagnosis use of anxiolytics and antidepressants on the risk of DP; 3) Investigate if these associations differ between the reference cohort and the patient cohort.
Material and methods
Source population
The study period proceeded from 1 January 2000 to 26 February 2012 within the entire Danish population of approximately 5.6 million inhabitants.
In Denmark, the entire population has free access to tax-financed health care, and a considerable amount of health-related information is recorded in national population-based registers. Accurate and unambiguous linkage of register data at the individual level is possible by means of a unique civil registration number assigned to all Danish citizens [Citation11].
During the entire study period it was possible to retire due to age at 65 years in Denmark and there was an anticipatory retirement scheme from the age of 60 years.
Patient cohort
Patients diagnosed with haematological malignancies during a period from 1 January 2000 to 31 December 2007 were identified in the Danish Cancer Register, which contains data on the incidence of cancer in the Danish population since 1943 [Citation12]. Patients with haematological malignancies were identified according to the International Classification of Disease (ICD-10) and time of diagnosis. Information regarding morphology was also obtained. Haematological malignancies were categorised according to morphology into the subgroups: Hodgkin lymphoma (C81), diffuse large B-cell lymphoma (C83.3), follicular lymphoma (C82), multiple myeloma (C90), acute myeloid/lymphoid leukaemia (C91.0, C91–94, except from C92.1 and 93.1), chronic myeloid leukaemia (C92.1), chronic lymphoid leukaemia (C91.1) and others (all other diseases classified as C91–96).
We included patients between 19 and 55 years of age, because they had to be of working age at time of diagnosis and at least five years following diagnosis. We excluded permanently work disabled patients or patients emigrated at time of diagnosis.
Reference cohort
A random reference cohort was sampled among the Danish population using the Danish Civil Registration System (CRS) containing personal data on all permanent residents in Denmark. Each cancer patient was individually matched on gender and date of birth to 10 persons without a history of haematological malignancies. Each individual in the reference cohort was assigned the same date of diagnosis, as the patient they were matched to. Included reference individuals could not develop haematological malignancies during the inclusion period (2000 to 2007).
We excluded reference individuals who were permanently work disabled or emigrated at time of diagnosis. Furthermore, reference individuals who were matched to patients that were excluded because of the above mentioned criteria, were also excluded.
Outcome
In Denmark DP is granted by the authorities if a person's work capacity is reduced in permanence to such an extent that return to work is unlikely.
Information on granted DP was obtained from the Danish Register for Evaluation of Marginalisation (DREAM), which is based on data from the Danish Ministry of Employment, the Danish Ministry of Education, CRS and SKAT (the Danish tax system). DREAM includes data on all Danish citizens who have received welfare benefits since 1991. Each person is registered once a week with a code indicating the type of welfare benefit received. DREAM has a 100% coverage of those granted DP in Denmark from 2000 and until now [Citation13].
Socioeconomic factors
Information on cohabiting status, children living at home, household income, educational level, and housing tenure was obtained from registers administered by Statistics Denmark, which is a central authority compiling and publishing statistics on the Danish society, especially on social and economic factors.
We obtained information on educational level from 1 October the year before diagnosis. Cohabiting status, children living at home, household income and housing tenure were assessed from 1 January the year of diagnosis.
Demographic factors
Data on age and gender were retrieved from the CRS [Citation11], and age was calculated at the time of diagnosis. Information on ethnicity was obtained from DREAM.
Comorbidity
Data on comorbidity was obtained from the Danish National Patient Register (NPR), which includes information on all hospital admissions in Denmark since 1977, as well as contacts to emergency rooms or outpatient clinics since 1995. Diagnostic information has been coded by physicians according to the ICD-10 system since 1994 at each contact [Citation14].
We computed a Charlson Comorbidity Index (CCI) score on the basis of the diagnoses recorded in the NPR for each patient during a five-year period before they were diagnosed with the haematological malignancy. In CCI, a weight is assigned to define categories of comorbid diseases, and the index is the sum of these weights (from 0 to 6). A higher CCI score indicates an increased severity of conditions. Conditions with a weight of one includes: Myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, connective tissue disease, ulcer disease, mild liver disease and diabetes. Conditions with a weight of two includes: Haemiplegia, moderate or severe renal disease, diabetes with end organ damage and any malignancy. Moderate or severe liver disease is given a weight of 3 and metastatic solid tumour or HIV receives a weight of 6 [Citation15]. A positive-predictive value greater than 90% have been found for almost all ICD-10 diagnostic codes used to ascertain the Charlson comorbidity conditions in the NRP [Citation16].
Since we only had few patients with high levels of comorbidity prior to diagnosis, we classified the score into three groups: 0, 1–2, and ≥ 3.
Use of anxiolytics or antidepressants
Use of anxiolytics or antidepressants was used as an indicator of mental health status following diagnosis. To investigate whether patients who needed treatment with either anxiolytics or antidepressants after diagnosis had a higher risk of receiving DP, data on the prescription-based use of these drugs was obtained from the Danish National Prescription Register, which contains information on all dispensed prescriptions since 1994. These data include the type and amount of drug prescribed according to the Anatomical Therapeutical Chemical Classification System (ATC), and the date of drug redemption [Citation17].
The ATC codes of interest were antidepressants (N06A) and anxiolytics (N05B), and it was registered if the patients were prescribed these types of medication during the first three years following diagnosis.
Statistics
Individuals in the patient cohort and the matched reference cohort were followed from date of diagnosis until DP, emigration, old age pension or anticipatory pension, death or 26 February 2012, whichever came first.
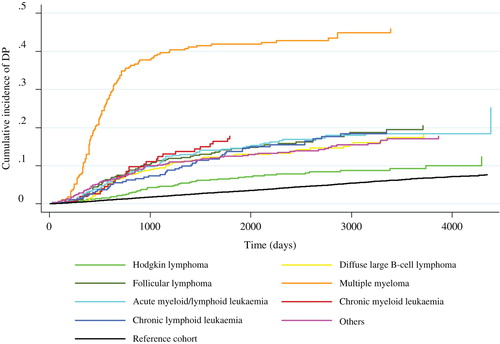
Cumulative incidence curves were computed to illustrate the incidence of DP according to type of haematological malignancy.
Using generalised linear regression models for pseudo observations [Citation18], age- and gender-adjusted relative cumulative risks (RR) of DP and associated 95% confidence intervals (CI) two, four and six years after diagnosis were estimated for the eight subgroups of haematological malignancies (Hodgkin lymphoma, diffuse large B-cell lymphoma, follicular lymphoma, multiple myeloma, acute myeloid/lymphoid leukaemia, chronic myeloid leukaemia, chronic lymphoid leukaemia and others) compared to the reference cohort (Model 1). Wald tests were used to test if the RRs differed between subgroups.
The associations between comorbidity, socioeconomic and demographic factors and the risk of DP four years after diagnosis were studied separately for the patient cohort and the reference cohort (Model 2). Covariates in the model included: Diagnosis (Hodgkin lymphoma, diffuse large B-cell lymphoma, follicular lymphoma, multiple myeloma, acute myeloid/lymphoid leukaemia, chronic myeloid leukaemia, chronic lymphoid leukaemia and others); gender (male, female); comorbidity (0, 0<); age (19–35, 36–40, 41–45, 46–50, 51–55 years); ethnicity (Danish citizens, immigrants or descendants from western countries, immigrants or descendants from non-western countries); cohabiting status (cohabiting, living alone); children living at home (yes, no); housing tenure (owner-occupied, rental); highest attained educational level (primary school or high school, higher education, vocational education); history of sick leave 12–24 months before diagnosis; (3–7 weeks, 8–13 weeks, 14–25 weeks and > 26 weeks); household income (low income (first quartile), middle income (second and third quartiles), and high income (fourth quartile)). The household income was reported after taxation and adjusted for number of persons in the household in the following way: household income/(no. of persons in household0.6). Wald test was used to test for overall interaction between the two cohorts and all the independent variables. In order to test for interaction for each factor and the two cohorts two tests were conducted. In the first test an interaction term was included between the two cohorts and all the independent variables at the same time. This model thereby enabled interaction between all factors and the two cohorts. In the second test, an interaction term was included between the two cohorts and each of the independent variables one at a time (without including other interactions). This model did thereby not enable interaction between any of the other factors and the two cohorts.
In Model 3 use of antidepressants or anxiolytics after diagnosis (entered as a time dependent variable and categorised as yes/no) was the main independent variable, and we adjusted for all covariates included in Model 2. The same analysis was also performed with the two drug groups separately. Again, we estimated the RRs four years after diagnosis, the analyses were performed separately in the two cohorts, and we tested for interaction between the two cohorts and the main independent variables using the same strategies as in Model 2.
In all three models two-sided Wald tests were used to test the overall association between each independent variable and the risk of DP. Death, anticipatory pension, and old age pension were considered competing events in all the analyses.
Results
A total of 3616 patients between 19 and 55 years of age were diagnosed with haematological malignancies for the first time between 2000 and 2007; and hence initially the reference cohort consisted of 36 160 individuals.
A total of 29 (1%) patients were excluded as they were emigrated and 393 (11%) because they were already permanently work disabled at time of diagnosis. Furthermore, 37 (0.1%) individuals were excluded from the reference cohort as they had a history of a haematological malignancy, 716 (2%) were excluded due to emigration and 2560 (7%) because they were permanently work disabled at diagnosis. Thus, a total of 3194 (88%) patients and 28 627 (79%) reference individuals were included in the study ().
In the end, at least four reference individual were matched to each patient. The median age was 45 years ranging from 19 to 55 years and 41% were women.
Subtypes of haematological malignancies
The 3194 patients were followed for a median of six years [interquartile range (IQR): 2–8], and a total of 550 (17%) were granted DP during the follow-up period. The highest proportion was found for patients with multiple myeloma (44%), and the lowest for patients with Hodgkin lymphoma (9%). The reference cohort was followed for a median of seven years (IQR: 6–10), and in all, a total of 1511 (5%) were granted DP during the follow-up period ().
Table I. Reference and patient cohort outcome stratified by subtype of haematological malignancy.
The cumulative incidence of DP by type of haematological malignancy is illustrated in . All sub-groups had higher incidences of DP than the reference cohort. The highest incidence was found for patients with multiple myeloma, and especially the first three years after diagnosis there was a notable increase in the incidence of DP for this subgroup of patients.
Figure 2. Cumulative incidence of DP according to type of haematological malignancy (death, old age pension and anticipatory pension were considered as competing events).
presents the results of the multivariable analyses of the risk of DP according to subtype of haematological malignancy compared to the reference cohort (Model 1). Both two, four and six years after diagnosis, haematological malignancy subgroup was significantly associated with the risk of DP (p < 0.001), and RRs differed significantly between the eight subgroups (p < 0.001). These associations were strongest two years after diagnosis and became slightly weaker year by year, as the risk of DP increased in the reference cohort with increasing age. The relative risks were lowest for patients with Hodgkin lymphoma and four years after diagnosis this subgroup had a 2.5-fold higher risk of receiving DP than the reference cohort (adjusted RR 2.64, 95% CI 1.84–3.78). The highest relative risk was found for patients with multiple myeloma, and four years after diagnosis, the risk of DP was 12-fold higher for this patient group compared to the reference cohort (adjusted RR 12.53, 95% CI 10.57–14.85). At this time-point, the other sub-groups of haematological malignancies had three- to six-fold higher risks of DP compared to the reference cohort.
Table II. Age- and gender-adjusted relative cumulative risk of disability pension two, four and six years after diagnosis for subtypes of haematological cancer compared to the reference cohort.
Influence of clinical, socioeconomic and demographic factors
The influence of clinical, socioeconomic and demographic factors on the risk of DP in the patient cohort and the reference cohort was investigated in Models 2 and 3, and the results of those analyses are presented in and .
Table III. The relative cumulative risk of disability pension four years after diagnosis according to clinical, demographic, socioeconomic factors and stratified by patients/references.
Table IV. The relative cumulative risk of disability pension four years after diagnosis according to use of antidepressants and/or anxiolytics after diagnosis stratified on patients/references.
Most of the associations were pointing in the same direction for the two cohorts but were stronger in the reference cohort compared to the patient cohort. An overall interaction between the two cohorts and the clinical, socioeconomic and demographic factors was found (p < 0.001). This indicates that the haematological malignancy modified the associations between the independent variables and DP. P-values from tests of interaction for each factor are presented in the last column in and .
Socioeconomic and demographic factors
The socioeconomic and demographic factors seemed to be equally distributed in the two cohorts. In both cohorts gender was found to be associated with the risk of DP, as the risk was higher for women than men (adjusted RR 1.31, 95% 1.10–1.57 and 1.33, 95% 1.09–1.62). A negative association was found between both income and educational level and the risk of DP in the two cohorts. A positive association was found between both age and the extent of sick leave before diagnosis and receiving DP in the two cohorts ().
Clinical factors
The proportion of individuals with a presence of comorbidity according to the Charlson Comorbidity Index was higher in the patient cohort (11%) than the reference cohort (6%). Furthermore, there was a positive association between level of comorbidity and the risk of DP in both cohorts. Individuals with a CCI score ≥ 3 had a 1.5-fold higher risk of DP in the patient cohort (adjusted RR 1.58, 95% CI 1.16–2.14), and a three-fold higher risk in the reference cohort (adjusted RR 2.98, 95% CI 1.52–5.83) compared to those with a CCI score of 0 ().
In the patient cohort, 18% were prescribed anxiolytics and/or antidepressants after diagnosis, compared to 7% in the reference cohort (). Moreover, we found an association between use of antidepressants and/or anxiolytics and the risk of DP, as patients who were prescribed these types of medication after the diagnosis of haematological malignancies were more likely to be granted DP compared to those who were not (adjusted RR 1.29, 95% CI 1.07–1.55). This association was also found when analysing the two drug groups separately and could also be observed in the reference cohort (adjusted HR 1.77, 95% CI 1.43–2.20).
Discussion
In this nationwide register-based cohort study we found that patients with eight subtypes of haematological malignancies (Hodgkin lymphoma, diffuse large B-cell lymphoma, follicular lymphoma, multiple myeloma, acute myeloid/lymphoid leukaemia, chronic myeloid leukaemia, chronic lymphoid leukaemia and others) had a higher risk of DP compared to a reference cohort; However, the relative risks differed considerably between the subtypes. The highest relative risks were found for patients with multiple myeloma, which might be explained by the chronic and progressive nature of this disease. The lowest relative risks were found for patients with Hodgkin lymphoma, which in contrary, is a curable disease. However, the proportion of death differed widely between the subgroups, and this should be taking into account when interpreting the results. The highest proportion of death was found for patients with acute myeloid/lymphoid leukaemia where 44% patients died during the follow-up period. This illustrates that although this subgroup did not have the highest relative risks of DP, these diseases have serious consequences for the patients. To the best of our knowledge, this is the first major study where the risk of DP has been estimated in clinically relevant subgroups of patients with haematological malignancies compared to a reference cohort. In most previous studies on the risk of DP among patients with cancer, haematological malignancies have been pooled in groups relevant in term of biology, but not by clinical relevance. Diseases such as acute myeloid/lymphoid leukaemia, chronic myeloid leukaemia, and chronic lymphoid leukaemia have, for instance been pooled under the term “leukaemia”, even though the relative survival five years after diagnosis in these groups range from 19% to 71% [Citation19]. This present study, however, showed that the risk of DP differed between many of the subgroups. A recent study on return to work for patients diagnosed with haematological malignancies on long-term sick leave showed similar results [Citation8], and together these two studies confirm a clear need of distinguishing between different types of haematological malignancies when considering future labour market participation.
A general pattern in this present study was that except for gender there was a tendency that the haematological malignancy modified the association between the socioeconomic, demographic and clinical factors and the risk of DP, and most of the factors had a stronger impact on the risk of DP in the reference cohort compared to the patient cohort. Since the reference cohort had stronger statistical power than the patient cohort, comparisons of level of significance for associations in the two cohorts must be made with caution. However, the tests of interaction also showed significant interaction between most of the factors and the two cohorts. We do not know the mechanisms behind this result, but it could maybe indicate that the impact of the haematological malignancy on the risk of DP was so predominant that it diminished the effect of both presence of comorbidity, history of long-term sick leave, socioeconomic and demographic factors and needing treatment with antidepressants or anxiolytics after diagnosis. Most previous studies have not investigated these associations separately for both cancer patient cohorts and reference cohorts, and therefore conclusions about factors associated with the risk of DP for cancer patients have only been based on results from patient populations. This study adds new knowledge since it shows that even though some factors are associated with the risk of DP among patients diagnosed with haematological malignancies these are even stronger in the general population. Furthermore, the results indicate that inclusion of reference cohorts in general should be considered when performing studies on labour market participation in patient cohorts.
We found that the proportion of patients with comorbidity was higher in the patient cohort compared with the reference cohort. The reason for this is unclear, though a few cases may relate to the increased risk of lymphomas in patients with diseases of the immune system, and of leukaemias and lymphomas in patients treated with chemotherapy [Citation20]. We also found the presence of comorbidity to be positively associated with the risk of DP in both the reference cohort and the patient cohort. Similar to our study, an association between comorbidity and risk of DP has been documented in studies on other cancer groups [Citation21–23].
We also found that patients treated with antidepressants or anxiolytics after the diagnosis of haematological malignancies were more likely to be granted DP compared to those who were not. To our knowledge, the association between mental health status following a haematological malignancy and the risk of DP has only been investigated in a Norwegian cross-sectional study from 1994. The study comprised 459 patients diagnosed with Hodgkin lymphoma 3–23 years before the study was conducted. Symptoms of depression and anxiety were measured using a validated self-reporting scale, and similar to the results of our study, both high scores of anxiety and depression were found to be associated with higher risk of being granted DP [Citation24]. We are aware that use of antidepressants or anxiolytics can only be regarded as a surrogate marker of mental health. We had no clinical observations except the haematological diagnosis, hence caution is necessary when comparing the findings to results based on self-reporting or to studies where anxiety and/or depression has been evaluated by other methods, i.e. evaluation by health professionals, audit of patient records, or central databases such as the NPR.
Strengths and limitations
One of the strengths of our study is the use of population-based registries with complete follow-up. This enabled us to describe the risk of DP among patients with haematological malignancies in a relatively large unselected population. The design was prospective allowing us to evaluate temporal associations, and all patients between 19 and 55 years of age diagnosed between 2000 and 2007 were eligible for inclusion. The fact that information on all variables was obtained through registers reduced the risk for recall and selection bias, and finally the risk of measurement bias due to misclassification of the outcome is modest, since we assume that DREAM has a 100% coverage of granted DPs in Denmark [Citation25].
However, the study also has some limitations. First, the multivariable analyses were performed under the assumption that except for the patient/reference cohort there was no interaction between any other variables. It would have been relevant to perform analyses stratified on age groups and on diagnosis in order to investigate if the associations differed according to these variables. However, due to the limited number of individuals in each age group and diagnosis sub-group, we were not able to make this stratification.
Second, for some of the explanatory variables there were missing values. The multivariable analyses were performed as complete-case analyses, and therefore cases with missing data were not included in the analyses. However, the amount of missing data was modest, and we assume that they were missing at random. Therefore we do not expect that this issue has biased our estimates.
Third, the reference cohort was sampled, so that individuals could not develop haematological malignancies during the inclusion period. The reference cohort was therefore potentially “more healthy” than the patient cohort. Due to the low incidence of haematological malignancies in the general population, we do, however, expect this potential selection bias to have little impact on our study.
Finally, we had no access to data on disease status (complete or partial remission), which could also have had an impact on labour market participation. Unfortunately, this was also the case for type of treatment, and even though treatment clearly is related to the diagnosis, important associations may be overlooked.
Similarly, we had no information on self-reported symptoms of late effects like physical impairments, fatigue, anxiety and depression, which in several studies have been shown to be endemic among patients with haematological malignancies [Citation26]. Future studies might combine register-based data sources with data from questionnaires in order to explore the association between these factors and labour market participation.
Conclusion
In conclusion, patients with all eight subtypes of haematological malignancies had a higher risk of DP compared to the reference cohort. The risk differed between the subtypes of haematological malignancies and the relative risk of DP was highest for patients with multiple myeloma.
In the patient cohort we found that gender, age, ethnicity, educational level, household income, history of long-term sick leave, comorbidity and need of treatment with anxiolytics or antidepressants after diagnosis were associated with risk of DP. However, the haematological malignancy seemed to reduce the influence of most of these factors, since they were stronger in the reference cohort.
The results of this study imply that clinicians should be aware that the risk of permanently reduced work capacity differs between subtypes of haematological cancer. This knowledge is important in order to initiate early targeted rehabilitation interventions aimed at preventing permanently reduced work capacity and maintaining appropriate labour market participation if possible. Furthermore, the results indicate that clinicians should acknowledge that even though the patterns of risk factors for DP in patients with haematological cancer are similar to those in the general population they are not necessarily as dominant, and therefore attention should also be paid to haematological cancer patients who are not exposed to risk factors that are generally known to be associated with a higher risk of DP.
Future studies should focus on which rehabilitations interventions that are feasible and effective for different cancer types and treatments taking age, gender, comorbidity and socioeconomic factors into account.
Acknowledgements
We thank Merete Labriola and Thomas Lund for helpful suggestions.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
This work has been supported by grants from The Danish Cancer Society (grant number R56-A3231), Aarhus University Hospital, The Health Insurance Foundation (grant number: 2012B026), Public Health and Quality Improvement, Central Denmark Region, Max and Inger Wørzners Memorial Foundation, Andersen-Isted Foundation.
References
- Carlsen K, Oksbjerg Dalton S, Frederiksen K, Diderichsen F, Johansen C. Cancer and the risk for taking early retirement pension: A Danish cohort study. Scand J Public Health 2008;36:117–25.
- Syse A, Tretli S, Kravdal O. Cancer’s impact on employment and earnings – a population-based study from Norway. J Cancer Surviv 2008;2:149–58.
- Torp S, Nielsen RA, Gudbergsson SB, Fossa SD, Dahl AA. Sick leave patterns among 5-year cancer survivors: A registry-based retrospective cohort study. J Cancer Surviv 2012;6:315–23.
- Park JH, Park EC, Park JH, Kim SG, Lee SY. Job loss and re-employment of cancer patients in Korean employees: A nationwide retrospective cohort study. J Clin Oncol 2008;26:1302–9.
- Roelen CA, Koopmans PC, Groothoff JW, van der Klink JJ, Bultmann U. Sickness absence and full return to work after cancer: 2-year follow-up of register data for different cancer sites. Psychooncology 2011;20:1001–6.
- Short PF, Vasey JJ, Tunceli K. Employment pathways in a large cohort of adult cancer survivors. Cancer 2005; 103:1292–301.
- de Boer AG, Verbeek JH, Spelten ER, Uitterhoeve AL, Ansink AC, de Reijke TM, et al. Work ability and return- to-work in cancer patients. Br J Cancer 2008;98:1342–7.
- Horsboel TA, Nielsen CV, Nielsen B, Jensen C, Andersen NT, de Thurah A. Type of hematological malignancy is crucial for the return to work prognosis: A register-based cohort study. J Cancer Surviv 2013;7:614–23.
- Krokstad S, Johnsen R, Westin S. Social determinants of disability pension: A 10-year follow-up of 62 000 people in a Norwegian county population. Int J Epidemiol 2002; 31:1183–91.
- Horsboel TA, DE Thurah A, Nielsen B, Nielsen CV. Factors associated with work outcome for survivors from haematological malignancies – a systematic literature review. Eur J Cancer Care (Engl) 2012;21:424–35.
- Pedersen CB. The Danish civil registration system. Scand J Public Health 2011;39(7 Suppl):22–5.
- Gjerstorff ML. The Danish cancer registry. Scand J Public Health 2011;39(7 Suppl):42–5.
- Hedegaard Rasmussen J. DREAM database. The national labor market authority, Ministry of Employment, Denmark: 2012. Report No. 28. Copenhagen: Ministry of Employment, 2012.
- Andersen TF, Madsen M, Jorgensen J, Mellemkjoer L, Olsen JH. The Danish national hospital register. A valuable source of data for modern health sciences. Dan Med Bull 1999;46:263–8.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 1987;40:373–83.
- Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sorensen HT. The predictive value of ICD-10 diagnostic coding used to assess Charlson Comorbidity Index conditions in the population-based Danish national registry of patients. BMC Med Res Methodol 2011;11:83.
- Kildemoes HW, Sorensen HT, Hallas J. The Danish national prescription registry. Scand J Public Health 2011; 39(7 Suppl):38–41.
- Parner ET, Andersen PK. Regression analysis of censored data using pseudo-observations. Stata J 2010;10:408,422.
- Roswall N, Olsen A, Christensen J, Rugbjerg K, Mellemkjaer L. Social inequality and incidence of and survival from Hodgkin lymphoma, non-Hodgkin lymphoma and leukaemia in a population-based study in Denmark, 1994–2003. Eur J Cancer 2008;44:2058–73.
- Royle JS, Baade P, Joske D, Fritschi L. Risk of second cancer after lymphohematopoietic neoplasm. Int J Cancer 2011; 129:910–9.
- Carlsen K, Harling H, Pedersen J, Christensen KB, Osler M. The transition between work, sickness absence and pension in a cohort of Danish colorectal cancer survivors. BMJ Open 2013;3:pii e002259.
- Kjaer T, Boje CR, Olsen MH, Overgaard J, Johansen J, Ibfelt E, et al. Affiliation to the work market after curative treatment of head-and-neck cancer: A population-based study from the DAHANCA database. Acta Oncol 2013;52:430–9.
- Damkjaer LH, Deltour I, Suppli NP, Christensen J, Kroman NT, Johansen C, et al. Breast cancer and early retirement: Associations with disease characteristics, treatment, comorbidity, social position and participation in a six-day rehabilitation course in a register-based study in Denmark. Acta Oncol 2011;50:274–81.
- Abrahamsen AF, Loge JH, Hannisdal E, Holte H, Kvaloy S. Socio-medical situation for long-term survivors of Hodgkin’s disease: A survey of 459 patients treated at one institution. Eur J Cancer 1998;34:1865–70.
- Christensen KB, Feveile H, Labriola M, Lund T. The impact of psychosocial work environment factors on the risk of disability pension in Denmark. Eur J Public Health 2008;18: 235–7.
- Johnsen AT, Tholstrup D, Petersen MA, Pedersen L, Groenvold M. Health related quality of life in a nationally representative sample of haematological patients. Eur J Haematol 2009;83:139–48.