To the Editor,
In definitive radiotherapy of locally advanced lung cancer, the lung dose constraints are often difficult to meet. In these cases treatment in deep inspiration breath hold (DIBH) is tempting, as the increased volume of the inflated lung enables fulfilment of the dose constraints [Citation1,Citation2]. However not all patients are suited for DIBH treatment.
We present three cases that demonstrate the caveats of the DIBH strategy.
Methods
All three patients were referred for definitive radiotherapy of non-small cell lung cancer (NSCLC) with 66 Gy in 33 fractions. Due to failure to fulfil dose constraints for lung in free breathing [mean lung dose (MLD) < 20 Gy and lung volume receiving 20 Gy or more (V20) < 37%], the patients were re-planned in DIBH with visual guidance using Real-time Position ManagementTM (RPM) system (Varian® Medical Systems) [Citation3]. Three-dimensional conformal technique was used for all plans.
Orthogonal kV images in DIBH were used for daily image guidance. DIBH cone beam computed tomography (CBCT), requiring three DIBH of 20 seconds, was acquired at 10th and 20th fractions as quality control [Citation4].
Results
The “good” case
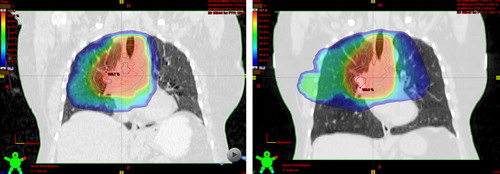
Patient #1 had an unspecified NSCLC (T3N3M0) with two tumours in the right upper lobe and lymph node metastases in levels 4R and 4L. Dose distribution on a free breathing midventilation scan resulted in a MLD of 21.1 Gy and V20 of 40.5%. In DIBH the total lung volume increased by 67%, MLD decreased to 19.7 Gy and V20 to 35.8% (). DIBH CBCTs showed reproducible tumour position during DIBH, suggesting a safe and accurate delivery of the dose to the tumour on a daily basis.
The “bad” case
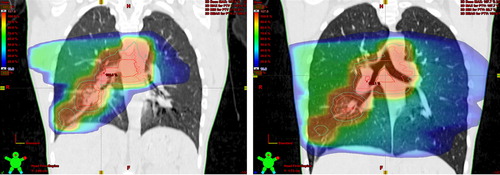
Patient #2 had a papillary adenocarcinoma (T3N3M0) with two tumours in the right lower lobe, intra bronchial tumour masses in the left main bronchus and mediastinal lymph node metastases in levels 4R, 4L and 7.
DIBH increased lung volume by 66%, but moved the targets apart resulting in an increase as well as a separation of the planning target volume (PTV), increasing MLD from 21.2 Gy to 23.1 Gy and V20 from 40% to 49% in free breathing versus DIBH (). Treatment was performed in free breathing.
The “ugly” case
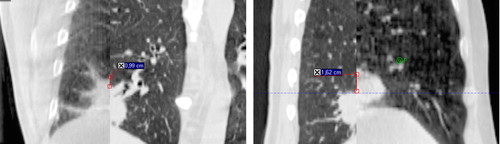
Patient #3 had an 8 cm large adenocarcinoma (T3N3M0) in the right lower lobe and lymph node metastases in levels 4R and 4L. Lung volume increased 82% in DIBH, decreasing MLD from 25.4 Gy to 18.7 Gy and V20 from 42% to 32%. DIBH CBCT at 10th fraction revealed inter-fractional variation in caudal tumour position of > 1.5 cm, despite good reproducibility of the external surrogate signal (). After this day, the DIBH level was adjusted daily to match the diaphragm position to its position on the treatment planning DIBH CT.
Conclusion
It is clear that not all NSCLC patients benefit from DIBH. Moreover, clinically significant uncertainties in DIBH reproducibility by means of external surrogate are present and daily setup to tumour is strongly recommended. We have started a feasibility study to investigate in detail the uncertainties in visually guided DIBH RT of lung cancer and to find the optimal image guidance protocol for DIBH [Citation5].
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Giraud P, Morvan E, Claude L, Mornex F, Le Pechoux C, Bachaud JM, et al. Respiratory gating techniques for optimization of lung cancer radiotherapy. J Thor Oncol 2011;6: 2058–68.
- Rosenzweig KE, Hanley J, Mah D, Mageras G, Hunt M, Toner S, et al. The deep inspiration breath-hold technique in the treatment of inoperable non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 2000;1:81–7.
- Keall PJ, Mageras GS, Balter J, Emery RS, Forster KM, Jiang SB, et al. The management of respiratory motion in radiation oncology. Report of AAPM Task Group 76. Med Phys 2006;33:3874–900.
- Duggan DM, Ding GX, Coffey CW, Kirby W, Hallahan DE, Malcolm A, et al. Deep-inspiration breath-hold kilovoltage cone-beam CT for setup of stereotactic body radiation therapy for lung tumors: Initial experience. Lung Cancer 2007;56: 77–88.
- Josipovic M, Persson GF, Håkansson K, Damkjær SMS, Bangsgaard JP, Westman G, et al. Deep inspiration breath hold radiotherapy for locally advanced lung cancer: Comparison of different treatment techniques on target coverage, lung dose and treatment delivery time. Acta Oncol 2013;52:1582–6.