Abstract
Background. Although families of children with cancer and other serious medical conditions have documented psychosocial needs, the systematic identification of needs and delivery of evidence-based care remain challenges. Screening for multifaceted family psychosocial risk is a means by which psychosocial treatment needs for pediatric patients and their families can be identified in an effective and inclusive manner.
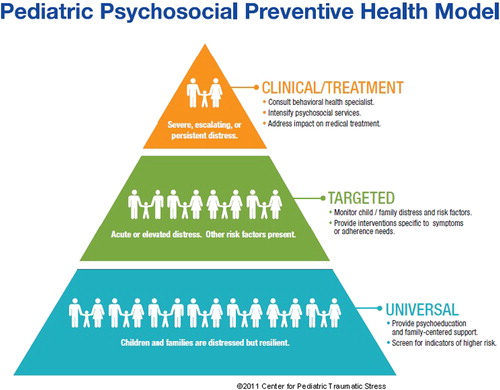
Material and methods. The Pediatric Psychosocial Preventative Health Model (PPPHM) is a model that can guide systematic assessment of family psychosocial risk. The Psychosocial Assessment Tool (PAT) is a brief parent report screener of psychosocial risk based on the PPPHM that can be used for families of infants through adolescents. The PPPHM and the PAT are described in this paper, along with a summary of data supporting systematic risk assessment.
Results. The PPPHM outlines three tiers of family psychosocial risk – Universal (low), Targeted (medium), and Clinical (high). The PAT is a validated measure of psychosocial risk. Scores on the PAT, derived from multiple sites and disease conditions, map on to the PPPHM with indications that one-half to two-thirds of families score at the Universal level of risk based on the PAT.
Conclusion. The PAT is a unique screener of psychosocial risk, both in terms of its breadth and underlying model (PPPHM), and its length and format. As an example of a means by which families can be screened early in the treatment process, PAT scores and corresponding PPPHM levels can provide direction for the delivery of evidence-based psychosocial care.
Background
The psychosocial demands on families in the face of life threatening pediatric illnesses are well known. Despite these demands, most families are able to cope and adjust to these situations. However, all families experience some level of distress and all families will likely benefit from psychosocial support. At the present time, treatment centers vary in the type and amount of psychosocial care offered to families. Perhaps more importantly, the delivery of this care is often not based on systematic data regarding the risks and needs of families, but rather based on available staff and resources, and existing referral patterns. The premise of this paper is that systematically screening for multifaceted family psychosocial risk is a means by which treatment needs for the patients and families can be identified in an effective and inclusive manner to facilitate a process of more in depth assessment and delivery of evidence-based care, as needed, matched to patient and family need.
Screening is an established public health mechanism that facilitates clinical care by identifying people with, or at risk for, specified problems. Screening can also ease the translation of research into practice by identifying groups of patients and families best suited to particular intervention approaches. Therefore, screeners of psychosocial risk should include questions based on key research findings (e.g. factors related to adjustment over time and the need for intervention) and be administered efficiently in order to pair screening results with appropriate interventions. Screening for behavioral and psychosocial concern in health settings has become a topic of increasing attention [Citation1]. However, screening specific to children and families in the health care environment is less frequently addressed. In contrast to adult screening, which is often focused on symptoms reported by individuals about themselves (e.g. depression screening), screening in child health and emerging work in primary care is usually parent report, focuses on child behavior problems or development, and usually includes information about the family.
A social ecological approach to screening offers a broad array of potential targets for intervention and includes strengths as well as vulnerabilities of families [Citation2]. Family assessments/screening focuses on inter-related systems with questions about the child, family, and illness prominent. Other systems intimately linked to successful adaptation and child health outcomes – healthcare settings, schools, social relationships, and communities – are also critical components of a comprehensive assessment. More distal systemic issues, such as culture, laws, and social class, provide additional context for a thorough conceptualization of risk and resilience. A comprehensive screen should include quick evaluation of relevant topics of the child's social ecology and in the context of a broader systemic model in order to identify factors impacting the child's functioning and to identify and prioritize interventions and key partners for long-term rehabilitation.
Despite the documented importance and perceived advantages of screening, there are few validated approaches [Citation3]. Approaches include: batteries of validated measures (e.g. well known measures of depression, anxiety, child behavior); very brief screeners, exemplified by the Distress Thermometer [Citation4]; and structured clinical interviews (e.g. HEEADSS 3.0; [Citation5]). Each approach has clear benefits, including strong psychometric properties for the longer batteries, length for the very brief screeners, richness for clinical interviews. Each also has drawbacks, such as length and scoring demands for batteries, lack of specificity for very brief screeners, and need for trained staff for clinical interviews.
This paper focuses on a model to guide screening, the Pediatric Psychosocial Preventative Health Model (PPPHM), and a screening tool for psychosocial risk, based on the PPPHM, the Psychosocial Assessment Tool (PAT). This paper provides a summary of current findings of the PAT and illustrates linkages to the PPPHM and implications for clinical care.
Material and methods
The Pediatric Psychosocial Preventative Health Model
The PPPHM () is based on a public health framework and used to conceptualize families with varying levels of psychosocial risk along with interventions matched to risk [Citation6]. At the base of the pyramid are Universal families, who are understandably concerned or distressed about their child's health problem but who are generally resilient and able to cope and adapt to their child's illness and treatment. The middle tier consists of Targeted families, with pre-existing concerns or difficulties that may contribute to continuing or escalating vulnerability during treatment. At the tip of the pyramid are Clinical families, with one or more pre-existing, chronic, and complex problems and resulting greatest need for prompt and often intensive intervention.
The Psychosocial Assessment Tool (PAT)
The Psychosocial Assessment Tool (PAT) is a brief (5–10 minutes) parent report screener of psychosocial risk in the context of the family in pediatrics. The PAT is based on the PPPHM and is composed of items that assess potential stressors (risks) associated with the child, family, and broader systems. The number of items varies depending on the age of child and of siblings (if any) and also the version used (e.g. adaptations for different diseases may result in additional items). The domains covered by the PAT are: demographic characteristics, diagnosis, family structure, family resources, social support, child knowledge of disease, school enrollment, school placement, child problems (internalizing, externalizing, social, cognitive), sibling problems, family problems, family beliefs, and stress responses. The PAT has been used with families across a broad age range, from infants to adolescents. The PAT is best administered via a web-based version or REDCap on a tablet computer but also can be administered in its original paper and pencil format. The PAT is currently used at 50 sites in 28 states in the US. The PAT has been translated into Spanish, Columbian Spanish, Dutch, Brazilian Portuguese, Hebrew, Greek, Polish, Italian, Japanese, Chinese, and Korean and is used internationally in these contexts. English adaptations for Canada, the United Kingdom, Australia, New Zealand, and Singapore are also available. The U.S. English and Spanish versions are “all-literacy” accessible with a fourth grade reading level.
Results
Summary of research on the PAT
The initial version of the PAT showed that families could be classified at diagnosis as high or low risk [Citation7]. This differential risk was consistent in a second sample and predicted use of social work services [Citation8]. The PAT was revised with seven empirically derived theoretically and clinically meaningful subscales with strong psychometric properties ([Citation9]; ) and is the version used in the studies described in this paper. The revised version was called PAT2.0. It is referred to simply as PAT in this paper. In addition to a series of studies from The Children's Hospital of Philadelphia (CHOP) where PAT was developed, independent research on the PAT comes from five other major children's oncology centers in Australia [Citation10], Canada [Citation11], The Netherlands [Citation12] and the US (Mississippi [Citation13], Georgia [Citation14]). PPPHM risk classification is generally stable across the first four months of cancer treatment [Citation15]. About two-thirds of families stay at the same level of risk and there is more stability for families at the Universal than those at the Targeted and Clinical levels. Persistent psychosocial risk, as measured by PAT, was associated with financial difficulties [Citation13].
Table I. PAT items, scales, scoring and summary of psychometric data1.
In order to study the feasibility of screening with PAT and the impact on psychosocial care provided, months where screening with PAT was standard clinical care were compared with months without screening [Citation16]. During months when the PAT was used, a mean of 7.2 risks per family was recorded in the medical record compared to 2.7 during assessment as usual months [Citation17], indicating that screening resulted in more documented risks. Facilitated by the effective identification of risks, families screened with PAT also received more psychosocial services and the services were matched to risk. The details of services in this study (for both groups) were derived only from general medical record data so the impact of screening as an intervention was not evaluated. However, Barrera and associates conducted a randomized clinical trial to examine the impact of providing a summary of risks derived from the PAT to the medical team and found reductions in PPPHM risk levels and in parental anxiety, child behavior, and quality of life associated with this intervention [Citation18].
Although the PAT was initially developed with families of children newly diagnosed with cancer it is also used broadly across the course of cancer treatment, including survivorship [Citation14]. The PAT has also been adapted for use in other pediatric conditions and settings (e.g. NICU [Citation19], bone marrow transplantation, chronic pain [Citation20], obesity, congenital heart disease and CICU, diabetes [Citation21]), with published reports in sickle cell disease [Citation22], kidney transplantation [Citation23], and irritable bowel disease [Citation24].
Across published studies and settings, family uptake of the PAT has been very positive. includes data on participation rates from studies of the PAT, all greater than 60% and most above 70%. In an early study we asked families if they would be comfortable with their completed PAT becoming part of their medical record and 85% indicated that they would be comfortable with it [Citation7].
Table II. Levels of risk in PPPHM.
Across sites and patient groups, the distribution of patients and their families across risk levels for the PPPHM, based on PAT scores, are reassuring in terms of the overall competence of families and are also strikingly consistent across settings and patient populations (). In general, one-half to two-thirds of samples score in the Universal tier on the PAT, one-quarter to one-third in the Targeted tier, and up to 15% fall in the Clinical tier.
Discussion
The data summarized in this paper address the importance of a systematic approach to screening for risks across the child's social ecology in order to initiate an evidence-based process of more detailed assessment and treatment. The PPPHM provides an underlying model that reflects the fact that the majority of families cope quite well with the demands of cancer and its treatment. At the same time, early identification of those families with more significant or persistent risks can be identified early in order to provide evidence-based treatments matched to their specific needs. The PAT is a validated screener of psychosocial risk with uptake across treatment centers internationally and application to a broader range of patient groups. It is a unique approach that is intended to compliment and in some cases augment other screening and assessment methods (e.g. batteries of validated measures, very brief screeners, clinical interviews) and can be integrated in broader research protocols [Citation25].
Using the PPPHM as a guide, assessment and treatment options vary by level. For families that fall in the Universal tier, little to no additional psychosocial assessment is needed. Many of the services currently provided in pediatric settings (e.g. social workers, child life specialists, chaplains, creative arts programs, family centered care programs, financial counselors, etc.) provide a broad undergirding of care that will address many of the treatment needs of Universal families.
Additional specific assessment that is matched to identified risks is indicated when a family scores in the Targeted tier to determine a highly specific treatment plan. There are many evidence-based interventions developed that are appropriate for families at the Targeted level. These include cognitive behavioral therapy for pain and behavioral or multicomponent interventions for adherence to medical regimens (see http://www.apadivisions.org/division-54/evidence-based/).
At the Clinical level, comprehensive assessment by behavioral medicine teams are usually necessary to assess and determine the most appropriate interventions for the patient and family. In addition to Universal services that all families would receive, families in the Clinical tier are likely to benefit from multidisciplinary interventions that address the focal and immediate needs of the family as well as larger more systemic interventions. Notably, the PPPHM provides a “snapshot” of the family's risks and resilience. Therefore, continued monitoring of risk for all families is critical to capture changes in risk over time is warranted.
There are important considerations in the refinement of screening instruments and processes for the future. As with any assessment process, the use and interpretation of data from the PAT must be used thoughtfully and in a clinically astute manner. Our experience has been that families appreciate the fact that we are asking about their psychosocial wellbeing and participation rates in PAT research studies have been high. The PPPHM elicits normative characteristics of families and the data supporting it indicate the inherent competencies of families. It is also possible that some families, particularly those with more difficulties or who are less engaged with the healthcare system, may not complete the PAT or do so honestly. In order to engage families and build collaborative partnerships among patients, families and healthcare teams, it is important to consider how information on scoring can be shared with patients and families and how it can be used to plan interventions collaboratively, consistent with family centered care models [Citation26,Citation27]. It is also important that all staff working with a family treat PAT data with appropriate sensitivity and confidentiality and work creatively to engage families in care and avoiding labeling or stigmatizing families with more difficulties [Citation28]. With regard to the impact of screening on the healthcare team, screening can generate a “task list” for clinicians to address. Although this may generate more responsibilities for clinicians, the feedback that we have received from clinicians is that any additional workload is offset by the value of intervening early and with specific goals.
The role that the child him/herself should or could play in screening is another area worthy of additional consideration. PAT screening is focused on the family, with the underlying assumption that families are an essential and the primary environment in child health. However, including the child's perspective is particularly important for child behavior, school issues, and adjustment to illness and treatment. With respect to the PAT, children (even adolescents) would not be expected to be knowledgeable about many of the items on the PAT because it asks about family problems that youth may not be aware of (e.g. financial problems, parental mental health issues), or may have a different interpretation about based on their perspective and age. Although the PAT has been validated in samples of families of children ranging from birth to young adulthood, assuring that the PAT is responsive to the needs of families at different stages of development is an important future consideration in screening.
While it is reasonable to think that delivering evidence-based treatments in a timely and focused manner will improve overall patient and family outcomes, this remains an area for future initiatives. For example, does screening improve access to appropriate evidence-based care and patient/family satisfaction with the care received? Can we impact quality of life or other outcomes that are important to patients and families? Screening is not intended to replace in-depth assessment or treatment but is the first step in a process of care delivery. How often screening should be repeated, which psychosocial risk factors are most associated with ongoing problems, and how screening data could be used to document clinically relevant changes are all important remaining questions.
The PPPHM also raises interesting questions for the design of psychosocial care at a healthcare setting/system level. There is great variability in psychosocial care across medical settings [Citation29], but concerns about equity in access to care, delivery of optimal interventions, and cost are common across all. In a review of pediatric psycho-oncology care, Wiener and colleagues concluded that existing guidelines and reports were not sufficiently current, comprehensive or evidence-based [Citation30]. The development of psychosocial standards of care is being undertaken by a multidisciplinary workgroup [Citation31]. Based on the PPPHM, care to families at the tip of the pyramid (Clinical) is the most expensive (e.g. psychiatric consultations, additional demands on nursing staff, physician time, patient care meetings focused on behavioral concerns, one-on-one monitoring of patients, involvement of hospital security or administration, more days in the hospital, and more clinic visits). Care at the Targeted tier is likely less intensive, less expensive and has the potential to be valuable over time, by reducing or preventing difficulties that impact health care (e.g. interventions related to pain, adherence to treatment, child behavior). Services at the Universal tier are least expensive (e.g. social work, child life, family resources centers and programs, chaplaincy, etc.) but delivered as part of family-centered care, adds value by impacting family satisfaction with care received.
Risk factors, such as socioeconomic status, child difficulties, parental distress, cultural values and beliefs, may contribute to disparities by limiting engagement in care or adherence to treatment [Citation32]. Many of the areas assessed by the PAT map directly or indirectly, on to areas associated with health disparities, such as income, health insurance, knowledge, sociocultural factors, health behaviors, adherence to treatment, and health access. More effective identification of family risks can foster earlier interventions to address factors that may contribute to health disparities. Similarly, more examination of cultural issues as the PAT is used in broader settings and other countries is also necessary. Beyond some of the more evident differences in healthcare financing, cultural and societal issues may need to be considered in more detail.
Tablet technology is employed by healthcare systems to facilitate medical and psychosocial screening. Although EHR systems were not designed to support psychosocial care, psychosocial risk screening can be introduced when healthcare team members endorse the concept and if screening modalities are easy to use, integrated with clinical care and associated with improvements in care delivery. Providing screeners in user-friendly formats reduces some of the demand on the personnel responsible for conducting the screening. And, the transmission of data into the EHR has the potential to further simplify screening and facilitate integration of the results into patient care and records.
In summary, this is a new and growing area of research. With increasing emphasis on the delivery of healthcare and with the integration of psychosocial and medical care, it will be important to conduct research on larger samples and to link screening results with key clinical outcomes. Screening is the first step in assuring that the psychosocial risks and resiliencies of all families entering pediatric healthcare systems are detected early in the course of care. When linked to a conceptual model for delivering care, such as the PPPHM, clinical pathways can be developed and tested. Ideally screening is a clinical activity supported by all members of the healthcare team, including the patient/family and can be completed in a manner that is consistent with family-centered care and appreciative of the variability in resources available across settings.
Acknowledgments
This paper is derived from a 2014 presentation by the first author at the European Cancer Rehabilitation and Survivorship Symposium (ECRS) in Copenhagen, Denmark. The work discussed in this paper has been supported by the National Cancer Institute (R21CA98039), St. Baldrick's Foundation, the American Cancer Society (RSG-13-015), the Substance Abuse and Mental Health Services Administration (U79SM058139, U79SM54325), and the Nemours Center for Healthcare Delivery Science. The PPPHM and the PAT are copyrighted. For information about its use contact [email protected].
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Institute of Medicine. Cancer care for the whole patient: Meeting psychosocial health needs. Washington, DC: The National Academies Press; 2007.
- Kazak AE, Rourke MT, Navsaria N. Families and other systems in pediatric psychology. In: Roberts MC, Steele RG, editors, Handbook of pediatric psychology, 4th ed. New York: Guilford Press; 2009.
- Kazak A, Brier M, Alderfer M, Reilly A, Fooks-Parker S, Rogerwick S, et al. Review: Screening for psychosocial risk in pediatric cancer. Pediatric Blood Cancer 2012;59:822–7.
- Haverman L, van Oers H, Limperg P, Houtzager B, Huisman J, Darlington A, et al. Development and validation of the distress thermometer for parents of a chronically ill child. J Pediatr 2013;163:1140–6.
- Goldenring J, Rosen D. Getting into adolescent heads: An essential update. Contemp Pediatr 2004;21:64–90.
- Kazak A. Pediatric Psychosocial Preventative Health Model (PPPHM): Research, practice and collaboration in pediatric family systems medicine. Families Systems Health 2006;24:381–95.
- Kazak A, Prusak A, McSherry M, Simms S, Beele D, Rourke M, et al. The Psychosocial Assessment Tool (PAT): Pilot data on a brief screening instrument for identifying high risk families in pediatric oncology. Families Systems Health 2001;19:303–15.
- Kazak A, Cant K, Jensen M, McSherry M, Rourke M, Hwang WT, et al. Identifying psychosocial risk indicative of subsequent resource utilization in families of newly diagnosed pediatric oncology patients. J Clin Oncol 2003;21:3220–5.
- Pai AL, Patino-Fernandez AM, McSherry M, Beele D, Alderfer M, Reilly A, et al. The psychosocial assessment tool (PAT2.0): Psychometric properties of a screener for psychosocial distress in families of children newly diagnosed with cancer. J Pediatr Psychol 2008;33:50–62.
- McCarthy M, Clarke N, Vance A, Ashley D, Heath J, Anderson V. Measuring psychosocial risk in families caring for a child with cancer: The Psychosocial Assessment Tool (PAT2.0). Pediatr Blood Cancer 2009;53:78–83.
- Barrera M, Hancock K, Rokeach A, Catuadella D, Atenafu E, Johnston D, et al. External validity and reliability of the Psychosocial Assessment Tool (PAT) among Canadian parents of children newly diagnosed with cancer. Pediatr Blood Cancer 2014;61:165–70.
- Sint Nicolaas SM, Schepers SA, Grootenhuis MA, Verhaak CM. Reliability, validity, and utility of the Dutch translation of the Psychosocial Assessment Tool. 15th World Congress of the International Psycho-Oncology Society (IPOS); 2013, October; Rotterdam, the Netherlands.
- Karlson CW, Smith ML, Haynes S, Faith MA, Pierce J, Elkin TD, et al. Risk for psychosocial problems in pediatric cancer: Impact on socioeconomics. Children's Health Care 2013;42.
- Gilleland J, Reed-Knight B, Brand S, Griffin A, Wasilewski-Masker K, Meacham L, et al. Assessment of psychosocial functioning in survivors of pediatric cancer using the PAT2.0. Psycho-Oncology 2013;22:2133–9.
- Alderfer M, Mougianis I, Barakat L, Beele D, DiTaranto S, Hwang WT, et al. Family psychosocial risk, distress and service utilization in pediatric cancer: Predictive validity of the Psychosocial Assessment Tool (PAT). Cancer 2009;115:4339–49.
- Kazak A, Barakat L, Ditaranto S, Biros D, Hwang W, Beele D, et al. Screening for psychosocial risk at cancer diagnosis: The Psychosocial Assessment Tool (PAT). J Pediatr Hematol Oncol 2011;33:289–94.
- Kazak A, Barakat L, Hwang W, Ditaranto S, Biros D, Beele D, et al. Association of psychosocial risk screening in pediatric cancer with psychosocial services provided. Psycho-Oncology 2011;20:715–23.
- Barerra M, Hancock K, Rokeach A, Atenafu E, Cataudella D, Punnett A, et al. Does the use of the revised Psychosocial Assessment Tool (PATrev) result in improved quality of life and reduced psychosocial risk in Canadian families with a child newly diagnosed with cancer? Psycho-Oncology 2014;23:165–72.
- Sampilo M, Lassen S, Belmont J, Parimi P. Development and validation of a psychosocial screening tool to identify high-risk families in the neonatal intensive care unit. National Child Health Psychology Conference; 2011, April; San Antonio, Texas, USA.
- Triemstra K, Eisenman E, Woods K. The utility of the PAT-Chronic Pain for use with children of different ages, gender and headache types. Poster presented at the Society of Pediatric Psychology Annual Conference; 2014, March; Philadelphia, Pennsylvania, USA.
- Norfolk J, McNamara K, Browne-Cooper K. Davis E, Mace J. The use of the psychosocial Assessment Tool (PAT2.0): Can it predict outcomes in youth with newly diagnosed Type I diabetes mellitus? World Diabetes Conference; 2013, December; Melbourne, Australia.
- Karlson C, Leist-Haynes S, Smith M, Faith M, Elkin TD, Megason G. Examination of risk and resiliency in a pediatric sickle cell disease population using the Psychosocial Assessment Tool 2.0. J Pediatr Psychol 2012;37:1031–40.
- Pai AL, Tackett A, Ittenbach RF, Goebel J. Psychosocial Assessment Tool 2.0 General: Validity of a psychosocial risk screener in a pediatric kidney transplant sample. Pediatr Transplant 2012;16:92–8.
- Pai ALH, Tackett A, Hente EA, Ernst MM, Denson LA, Hommel KA. Assessing psychosocial risk in pediatric inflammatory bowel disease: Validation of the PAT2.0_GEN. J Pediatr Gastroenterol Nutr 2014;58:51–6.
- Noll RB, Patel SK, Embry L, Hardy KK, Pelletier W, Annett RD, et al. Children's Oncology Group's 2013 blueprint for research: Behavioral science. Pediatr Blood Cancer 2013; 60:1048–54.
- McKay L, Gregory D. Exploring family centered care among pediatric oncology nurses. J Pediatr Oncol Nurs 2011;28: 43–52.
- Kuo D, Houtrow A, Arango P, Kuhlthau K, Simmons J, Neff J. Family-centered care: Current applications and future directions in pediatric health care. Matern Child Health J 2012;16:297–305.
- Blackall GF, Simms S, Green MJ. Breaking the cycle: How to turn conflict into collaboration when you and your patients disagree. Chapter 5. When all you know isn't enough: Dealing with chronic illness; Philadelphia: ACP Press; 2009. p. 59–70.
- Selove R, Kroll T, Coppes M, Cheng Y. Psychosocial services in the first 30 days after diagnosis: Results of a web-based survey of Children's Oncology Group (COG) member institutions. Pediatr Blood Cancer 2012;58:435–40.
- Weiner L, Viola A, Koretski J, Perper ED, Patenaude AF. Pediatric psycho-oncology care: Standards, guidelines, and consensus report. Psycho-Oncology Epub 2014 Jun 6.
- Wiener L, Patenaude A, Noll R, Kazak A, Sardi-Brown V, Brown P. Establishing pediatric psychosocial standards of care. Poster presented at the Children's Oncology Group; 2013, October; Dallas, Texas, USA.
- Bhatia, S. Disparities in cancer outcomes: Lessons learned from children with cancer. Pediatr Blood Cancer 2011;56:994–1002.
- Hearps SJ, McCarthy MC, Muscara F, Hearps SJC, Burke K, Jones B, et al. Psychosocial risk in families of infants undergoing surgery for a serious congenital heart disease. Cardiol Young 2014;24:632–9.
- Kazak A, Alderfer M. Hocking M, Schwartz L, Barakat L. Check-in About Recent Experiences and Strengths (CARES): A web-based table-administered caregiver-report assessment protocol. Poster presented at the Society of Pediatric Psychology Annual Conference; 2013, April; New Orleans, Louisiana, USA.