Abstract
Background. Whole body (WB) magnetic resonance imaging (MRI), including diffusion-weighted imaging (DWI) has become increasingly utilized in cancer imaging, yet the clinical utility of these techniques in follow-up of testicular cancer patients has not been evaluated. The purpose of this study was to evaluate the feasibility of WB MRI with continuous table movement (CTM) technique, including multistep DWI in follow-up of patients with testicular cancer.
Patients and methods. WB MRI including DWI was performed in follow-up of 71 consecutive patients (median age, 37 years; range 19–84) with histologically confirmed testicular cancer. WB MRI protocol included axial T1-Dixon and T2-BLADE sequences using CTM technique. Furthermore, multi-step DWI was performed using b-value 50 and 1000 s/mm2. One criterion for feasibility was patient tolerance and satisfactory image quality. Another criterion was the accuracy in detection of any pathological mass, compared to standard of reference. Signal intensity in DWI was used for evaluation of residual mass activity. Clinical, laboratory and imaging follow-up were applied as standard of reference for the evaluation of WB MRI. Results. WB MRI was tolerated in nearly all patients (69/71 patients, 97%) and the image quality was satisfactory. Metal artifacts deteriorated the image quality in six patients, but it did not influence the overall results. No case of clinical relapse was observed during the follow-up time. There was a good agreement between conventional WB MRI and standard of reference in all patients. Three patients showed residual masses and DWI signal was not restricted in these patients. Furthermore, DWI showed abnormally high signal intensity in a normal-sized retroperitoneal lymph node indicating metastasis. The subsequent 18F-FDG PET/CT could verify the finding.
Conclusion. WB MRI with CTM technique including multi-step DWI is feasible in follow-up of patients with testicular cancer. DWI may contribute to important added-value data to conventional MRI sequences regarding the activity of residual masses.
Testicular germ cell tumor is the most common cancer form in young men [Citation1]. Testicular cancer is divided into two main groups: non-seminoma (60%) and seminoma (40%), and treatment strategies differ between these two groups [Citation2]. Testicular cancer is a curable disease, and the great majority of patients are long-time survivors. Imaging is crucial for evaluation of metastatic spread as well as assessment of treatment response and follow-up [Citation2].
Contrast-enhanced computed tomography (CT) is considered as the standard radiological method for these purposes [Citation3]. Consequently, patients with testicular cancer usually undergo numerous CT studies in diagnostic and routine follow-up procedures. However, frequent CT examinations of testicular cancer patients (especially at young age) increase the risk of radiation-related cancers [Citation4]. Another disadvantage of contrast-enhanced CT is the risk for contrast-induced nephropathy [Citation5]. This is especially applicable for patients with renal failure in whom intravenous contrast agent is contraindicated. Both these downsides can be circumvented with the use of whole body (WB) magnetic resonance imaging (MRI).
WB MRI (from root of the neck to groin), including diffusion-weighted imaging (DWI) as a non-radiation and non-contrast enhanced method may have great potential in follow-up of patients with testicular cancer. DWI reflects the random motion of water molecules in body tissues and can be used in tumor characterization. Diffusion is more restricted in tissues with high cellular densities, such as tumor tissue [Citation6]. Furthermore, the continuous table movement (CTM) technique is a new advancement in WB MRI, and can be used for conventional MR sequences, resulting in a shorter acquisition time [Citation7].
The follow-up protocol was implemented according to earlier versions of the Swedish-Norwegian Testicular Cancer Project, SWENOTECA, included a high number of abdominal CT examinations (> 15) and chest x-rays [Citation8]. The radiation doses seemed arguable in the follow-up of stage I testicular carcinoma, in which all patients are potentially cured. According to the new recommendations from SWENOTECA, version VIII and IX, follow-up CT should be replaced with MRI or ultrasound, especially in patients younger than 35 years old [Citation8]. However, ultrasound is not as reliable as MRI or CT for the evaluation of retroperitoneal lymph nodes [Citation2,Citation8].
The aim of this study was to assess the feasibility of WB MRI with CTM technique, and multi-step DWI for follow-up of patients with testicular cancer. We also wanted to asses if WB DWI could contribute to important added value data to conventional MRI sequences on the activity of residual mass.
Material and methods
Patients
In this prospective study, 71 consecutive testicular cancer patients (median age, 37 years; range 19–84) were referred for imaging follow-up and underwent WB MRI, including DWI between July 2010 and January 2012 (the period refers to the first examination in every patient). In total, 145 WB MRI (range 1–5 scans per patient, median 2) were performed. The MRI examinations substituted the corresponding follow-up CT. In one patient, the WB MRI examination was performed as part of initial staging.
The inclusions criteria consisted of patients in follow-up after orchidectomy for germ cell tumors. The exclusion criteria included the common contraindication for performing MRI, such as metal implants, pacemaker, and claustrophobia. The initial staging imaging was performed by CT chest and abdomen in all but one patient according to recommendations from SWENOTECA; in this one patient initial staging was based on both CT and WB MRI. The follow-up imaging was carried out at different time points with CT, ultrasound, and WB MRI, according to recommendations from SWENOTECA, versions IV-VI [Citation8]. 18F-FDG PET/CT was performed in 10 patients when there were difficulties to differentiate between benign and malignant lesions by other imaging modalities. Initial clinical staging (CS) was classified according to Royal Marsden Hospital (RMH). The clinical data are summarized in . The study was approved by the local ethical committee.
Table I. Patient characteristics of 71 patients with testicular cancer.
WB MRI including DWI
The imaging was performed in a 1.5 T MR system (MAGNETOM Avanto, Siemens, Healthcare sector, Erlangen, Germany) with CTM equipment (Tim CT, Siemens, Healthcare sector). Immediately before start of scanning, either 20 mg butylscopolamin (Buscopan 20 mg/ml, Boehringer Ingelheim, Germany) or 1 mg Glucagon (Glucagon 1 mg/ml, Novo Nordisk A/S Bagsvaerd, Denmark) was injected intramuscularly in the thigh as an antiperistaltic agent. Three body matrix coils (9 elements), a neck coil (2 elements), and the built-in spine coil (36 elements) were used for signal reception. The WB imaging protocol consisted of three sequences: 1) Axial CTM fat-suppressed T2-weighted BLADE sequence during free breathing; 2) Axial CTM T1-weighted DIXON sequence during breath-holding. CTM technique applies a segmented multi-slice acquisition method in which the full k-space data of each slice is collected while the patient moves through the scanner. Simultaneous acquisition of multiple slices is possible by moving the acquisition trajectories of different slices in each time. Hence, the CTM technique allows seamless acquisition of multiple axial slices [Citation9].
3) Axial DWI with background body signal suppression technique (DWIBS) was performed at five acquisition stations during free breathing. DWI was performed in the axial plane using b-value 50 and 1000 s/mm2. Apparent diffusion coefficient (ADC) images were automatically calculated from these two b-values. Axial DW images were used to reconstruct high resolution 3D-maximum intensity projection (MIP) images. All sequences were performed from the root of the neck to the upper part of thighs. The total examination time was measured 45 minutes. No intravenous contrast was used. The imaging parameters are summarized in .
Table II. MRI sequence protocol (MAGNETOM Avanto, Siemens Healthcare).
Analysis of images
The image analysis was aimed to assess the feasibility of the WB MRI with CTM technique for follow-up of testicular cancer. One criterion for feasibility was patient tolerance and satisfactory image quality. The parameter for evaluating image quality was presence of artifacts affecting image interpretation. Another criterion for feasibility was accuracy of WB MRI including DWI in detection of lesions, which was evaluated by comparing the results with standard of reference. We also wanted to asses if WB DWI could contribute to important added value data to conventional MRI sequences on the activity of residual mass. This was done by evaluating the signal intensity in the residual mass on DWI as described below.
First, WB MRI including DWI was reviewed by two experienced radiologists, in consensus, employing a commercially available PACS reviewer (Carestream Health, Rochester, NY, USA). Except for patient's diagnosis, the reviewers were blinded to all clinical information including other imaging findings. Thereafter, the findings on WB MRI and other modalities, such as CT or PET/CT were reviewed together on a lesion-by-lesion basis, and with access to the clinical report.
On conventional MRI, i.e. T1-Dixon and T2-BLADE sequences, and CT, a lymph node was counted as suspicious if its short-axis diameter was greater than 1 cm [Citation10]. A malignant lesion showed high signal intensity on T2-BLADE, and intermediate or low signal intensity on T1-Dixon sequence. The signal intensity of DWI was assessed as malignant or not. On DWI, a lesion was suspected to be malignant if it showed a focal area with equal or higher signal intensity than the organ with the highest signal intensity in the same region, i.e. bone marrow in chest, and bone marrow and kidneys in abdominal region, and a lower or equal signal intensity on the corresponding ADC map [Citation11]. The positive findings on DWI had to be verified by conventional MR sequences to avoid false positive findings [Citation6].
Standard of reference
Clinical, laboratory and imaging follow-up were applied to all patients (range 14–32; median 26 months, i.e. from the time the first WB MRI was performed in every patient) according to the clinical routine of the oncology department.
Results
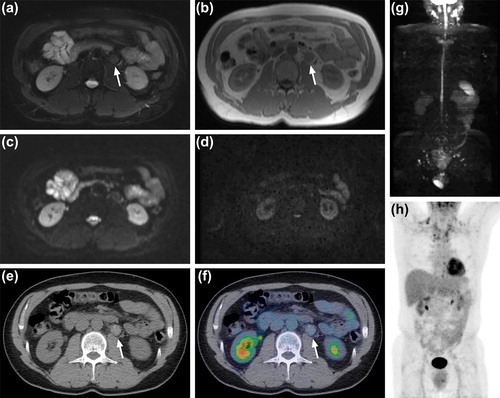
WB MRI including DWI was successfully performed in 69/71 patients (97%). The examination was discontinued in two patients because of claustrophobia. No patient relapsed during the follow-up time. WB MRI uncovered pathological findings in four patients: 1) One patient with CS IV showed a residual lung metastasis measuring 12 mm on the longest diameter, on CT, three years after the initial diagnosis. The lesion was clearly detected on T1-Dixon and T2-BLADE sequences. The lesion was not, however, detectable on DWI. The lung lesion was negative on 18F-FDG PET/CT, performed before WB MRI (). The follow-up investigations showed no signs of progression.
2) One patient with CS II showed four residual retroperitoneal metastases measuring 10–25 mm on the short-axis diameter, on CT, two years after the initial diagnosis. T1-Dixon and T2-BLADE sequences detected all lesions, but the lesions had low signal intensity on DWI. The lesions were negative on 18F-FDG PET/CT performed six months before WB MRI (). The follow-up investigations showed no signs of progression.
3) One patient with CS IV showed two residual lymph nodes, measuring 10 and 15 mm on the shortest diameter, in the retroperitoneum on CT five years after initial diagnosis. T1-Dixon and T2-BLADE sequences detected the lesions, and the DWI signal was not restricted. The follow-up investigations showed no signs of progression.
4) One patient showed no lymph node larger than 1 cm on short-axis diameter, on CT, at time of diagnosis. However, WB MRI performed two months later (as part of initial staging) showed a lymph node measuring 7 mm on short-axis diameter with very high signal intensity, on DWI, in the retroperitoneum. According to size criteria, this lesion could not be considered as metastasis, but because of abnormally high signal intensity, on DWI, the suspicious of metastasis was raised. Subsequent 18F-FDG PET/CT showed an intensive focal tracer uptake in this lesion, suggesting lymph node metastasis (). This patient was considered to have lymph node metastasis at definitive initial staging and classified as CS II, and was therefore treated with chemotherapy.
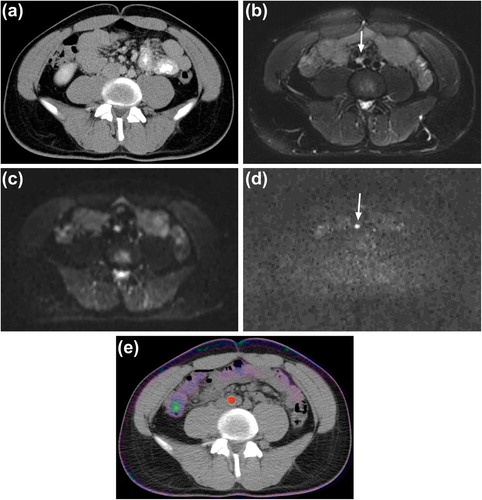
There were some difficulties in identifying/demarcating the residual lesions described above on ADC maps. Therefore, no ADC measurement was performed. Artifacts from metal clips in retroperitoneum deteriorated the image quality in six patients, but it did not influence the image interpretation and the overall results ().
Discussion
The recommended schedule for follow-up CT in patients with testicular cancer differs with stage and treatment given. In general the follow-up is intensive the first two years after diagnosis and treatment and then continue for 5–10 years resulting in 10–15 examinations. The potential advantage of frequent examinations should be weighed against the consequent radiation-related risks and financial costs. The effective dose of diagnostic procedures should be kept to a minimum as the risks of radiation-related malignancies persist throughout life-time. The radiation-related risk is higher if exposure occurs in young ages, like in testicular cancer patients [Citation4]. The EURATOM directive recommends that a radiation-free imaging modality should be used whenever possible [Citation12]. In addition, Cisplatin-induced nephropathy is a known acute and longstanding side effect in testicular cancer patients [Citation13]. In these particular patients, iodinated contrast agents used in CT examinations should be administered with caution, since cisplatin and iodinated contrast agent may have cumulative nephrotoxic effect.
In the present study, CTM technique was used for performing T1-Dixon and T2-BLADE sequences. Recently, this technique has been described as a promising technique in oncological imaging [Citation7,Citation14] and MR angiography [Citation15,Citation16]. It reduces the acquisition time, as no pause is required for patient repositioning. Image-analysis and workflow is also more efficient because all images are available in one seamless stack. The images were acquired in the axial plane throughout the body with the WB CTM technique, instead of coronal images in other WB MRI techniques, thereby facilitating detection of enlarged lymph nodes. Another advantage with the CTM technique is that the slices are acquired at isocenter of the gantry, which reduce the magnetic field inhomogeneities in the periphery of the field of view, and this should theoretically reduce metal artifacts compared to conventional WB MRI sequences. Additionally, scan time is reduced with this technique compared to the multi-step approach.
Our study protocol enabled scanning of the chest and abdominal regions within a short period of time and without exposure to ionizing radiation and intravenous contrast. Earlier studies suggested that MR chest is a reliable technique in detection of lung lesions and is significantly more accurate than chest x-ray [Citation14,Citation17] (). At present, there is a widespread availability of MR scanner and the cost of MR examination is reasonable. Therefore, CT should be avoided in follow-up of patients with testicular cancer and can be replaced by MR examination. In addition, the value of examination of chest region in follow-up of testicular cancer patient has been questionable [Citation18]. The cost and time of MRI examination can be further reduced if only MRI abdomen performs, instead of MRI chest and abdomen in our protocol, for follow-up of selected patients.
We used patient tolerance and image quality as parameters for feasibility of the CTM WB MRI in this patient group. There were some artifacts from metal clips in six patients with retroperitoneal lymph node dissection, but they did not affect the image interpretation. Metal artifacts, reducing sequences, or other modalities such as ultrasound or CT should be factored-in imaging follow-up of these specific patients. However, recurrent lymphadenopathy in close proximity to these metal clips may be difficult to identify by MRI. Imaging follow-up with contrast-enhanced CT may be considered in selected patients with metal clips, especially if tumor recurrence is clinically suspected.
In the present study, three patients showed residual lesions after treatment, on CT; one patient with a lung lesion and two patients with retroperitoneal lymph nodes. All these lesions could be verified by T1-Dixon and T2-BLADE sequences employing CTM technique. DWI signal was not restricted in all these lesions. The lesions were unchanged on clinical and imaging follow-up, and interpreted as residual benign findings. In another patient, DWI showed very high signal intensity in a normal-sized lymph node (less than 1 cm on short-axis diameter) which correlated to pathological 18F-FDG uptake on PET/CT. The patient was considered to have lymph node metastasis and classified as CS II and treated with chemotherapy (follow-up; 32 months). However, we have some reservations because this finding was not histologically confirmed.
The “not-restricted” DWI signal can be explained as; the lesions probably represent residual mass without malignant tissue. Any sort of treatment that induces necrotic cell death will reduce the diffusion signal in high b-values [Citation6]. Additionally, measurement of ADC value has been applied to differentiate between malignant and benign lymph nodes [Citation19,Citation20]. According to our results from the four patients with residual masses, we assume that DWI may provide information about the activity of residual masses as compared to conventional MRI sequences. However, this statement should be taken with caution since it reflects observations in only four patients. Several previous studies have shown that WB DWI is a promising technique in evaluating metastatic disease [Citation11,Citation21]. We found difficulties in the analysis of ADC; in three patients with not-restricted DWI, the lesions could not clearly be delineated on ADC images. In the patient with positive finding, with DWI, the ADC measurement was not possible due to small lesion size. Measurement of ADC in heterogeneous or small lesions is challenging, particularly in areas influenced by motion artifacts. Therefore, breath-hold or respiratory-triggered technique may be optimal for measurement of ADC in these lesions, instead of free breathing technique used in our study [Citation22].
There were some limitations in this study. We could not verify pathological findings through biopsy, because of small lesion size, inaccessible location for image-guided biopsy, or ethical and logistic reasons. In addition, no comparison was made between the standard CT and WB MRI. MR examinations were performed at different follow-up times, with the exception of one examination, performed at initial staging. Further studies using WB MRI in initial staging would be of value. In addition, only four patients in this study cohort had pathological imaging findings, and this reduces statistical interpretation and power.
Conclusion
Our study results demonstrate that WB MRI with CTM technique, including multi-step DWI, is feasible in the follow-up of patients with testicular cancer. DWI may offer important added-value data to conventional MRI sequences on the activity of residual masses.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics,2007. Cancer J Clin 2007;57:43–66.
- Sohaib SA, Koh DM, Husband JE. The role of imaging in the diagnosis, staging and management of testicular cancer. Am J Roentgenol 2008;191:387–95.
- Heidenreich A, Albers P, Classen J, Graefen M, Gschwend J, Kotzerke J, et al. Imaging studies in metastatic urogenital cancer patients undergoing systemic therapy: Recommendations of a multidisciplinary consensus meeting of the Association of Urological Oncology of the German Cancer Society. Urol Int 2010;85:1–10.
- Hricak H, Brenner DJ, Adelstein SJ, Frush DP, Hall EJ, Howell RW, et al. Managing radiation use in medical imaging: A multifaceted challenge. Radiology 2011;258:889–905.
- Mitchell AM, Jones AE, Tumlin J, Kline JA. Incidence of contrast-induced nephropathy after contrast-enhanced computed tomography in the outpatient setting. Clin J Am Soc Nephrol 2010;5:4–9.
- Padhani AR, Koh DM, Collins DJ. Whole-body diffusion-weighted MR imaging in cancer: Current status and research directions. Radiology 2011;261:700–18.
- Weckbach S, Michaely HJ, Stemmer A, Schoenberg SO, Dinter DJ. Comparison of a new whole-body continuous-table-movement protocol versus a standard whole-body MR protocol for the assessment of multiple myeloma. Eur Radiol 2010;20:2907–16.
- Available from URL: http://www.ocsyd.se/patientprocesser/SWENOTECA/vårdprogram.
- Fautz HP, Kannengiesser SA. Sliding multislice (SMS): A new technique for minimum FOV usage in axial continuously moving-table acquisitions. Magn Reson Med 2006; 55:363–70.
- Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47.
- Abdulqadhr G, Molin D, Åström G, Suurküla M, Johansson L, Hagberg H, et al. Whole-body diffusion-weighted imaging compared with FDG-PET/CT in staging of lymphoma patients. Acta Radiol 2011;52:173–80.
- EURATOM. EURATOM Council Directive 97/43/EURATOM of 30 June 1997 on health protection of individuals against the dangers of ionizing radiation in relation to medical exposure. Official J 1997;L180; 09/07/1997:P.0022–0027.
- Haugnes HS, Bosl GJ, Boer H, Gietema JA, Brydøy M, Oldenburg J, et al. Long-term and late effects of germ cell testicular cancer treatment and implications for follow-up. J Clin Oncol 2012;30:3752–63.
- Baumann T, Ludwig U, Pache G, Gall C, Saueressig U, Fisch D, et al. Detection of pulmonary nodules with move-during-scan magnetic resonance imaging using a free-breathing turbo inversion recovery magnitude sequence. Invest Radiol 2008;43:359–67.
- Koziel K, Attenberger UI, Lederle K, Haneder S, Schoenberg SO, Michaely HJ, et al. Peripheral MRA with continuous table movement: Imaging speed and robustness compared to a conventional stepping table technique. Eur J Radiol 2011;80:537–42.
- Voth M, Haneder S, Huck K, Gutfleisch A, Schönberg SO, Michaely HJ. Peripheral magnetic resonance angiography with continuous table movement in combination with high spatial and temporal resolution time-resolved MRA With a total single dose (0.1 mmol/kg) of gadobutrol at 3.0 T. Invest Radiol 2009;44:627–33.
- Vogt FM, Herborn CU, Hunold P, Lauenstein TC, Schröder T, Debatin JF, et al. HASTE MRI versus chest radiography in the detection of pulmonary nodules: Comparison with MDCT. Am J Roentgenol 2004;183:71–8.
- Tolan S, Vesprini D, Jewett MA, Warde PR, O’Malley M, Panzarella T, et al. No role for routine chest radiography in stage I seminoma surveillance. Eur Urol 2010;57:474–9.
- Zhang Y, Chen J, Shen J, Zhong J, Ye R, Liang B. Apparent diffusion coefficient values of necrotic and solid portion of lymph nodes: Differential diagnostic value in cervical lymphadenopathy. Clin Radiol 2013;68:224–31.
- Holzapfel K, Duetsch S, Fauser C, Eiber M, Rummeny EJ, Gaa J. Value of diffusion-weighted MR imaging in the differentiation between benign and malignant cervical lymph nodes. Eur J Radiol 2009;72:381–7.
- Laurent V, Trausch G, Bruot O, Olivier P, Felblinger J, Régent D. Comparative study of two whole-body imaging techniques in the case of melanoma metastases: Advantages of multi-contrast MRI examination including a diffusion-weighted sequence in comparison with PET/CT. Eur J Radiol 2010;75:376–83.
- Kwee TC, Takahara T, Ochiai R, Katahira K, Van Cauteren M, Imai Y, et al. Whole-body diffusion-weighted magnetic resonance imaging. Eur J Radiol 2009;70:409–17.
