Abstract
Background: Concurrent chemotherapy and thoracic radiotherapy (TRT) is recommended for limited disease small cell lung cancer (LD SCLC). Twice daily TRT is well documented, but not universally implemented – probably mainly due to inconvenience and concerns about toxicity. A schedule of three-week hypofractionated TRT is a commonly used alternative. This is the first randomized trial comparing twice daily and hypofractionated TRT in LD SCLC.
Material and methods: Patients received four courses of cisplatin/etoposide (PE) and were randomized to TRT of 42 Gy in 15 fractions (once daily, OD) or 45 Gy in 30 fractions (twice daily, BID) between the second and third PE course. Good responders received prophylactic cranial irradiation of 30 Gy in 15 fractions.
Results: 157 patients were enrolled between May 2005 and January 2011 (OD: n = 84, BID: n = 73). Median age was 63 years, 52% were men, 84% had performance status 0–1, 72% had stage III disease and 11% non-malignant pleural effusion. The treatment arms were well balanced. The response rates were similar (OD: 92%, BID: 88%; p = 0.41), but more BID patients achieved a complete response (OD: 13%, BID: 33%; p = 0.003). There was no difference in one-year progression-free survival (PFS) (OD: 45%, BID: 49%; p = 0.61) or median PFS (OD: 10.2 months, BID: 11.4 months; p = 0.93). The median overall survival in the BID arm was 6.3 months longer (OD: 18.8 months, BID: 25.1 months; p = 0.61). There were no differences in grade 3–4 esophagitis (OD: 31%, BID: 33%, p = 0.80) or pneumonitis (OD: 2%, BID: 3%, p = 1.0). Patients on the BID arm reported slightly more dysphagia at the end of the TRT.
Conclusion: There was no difference in severe toxicity between the two TRT schedules. The twice daily schedule resulted in significantly more complete responses and a numerically longer median overall survival, but no firm conclusions about efficacy could be drawn from this phase II trial.
Small cell lung cancer (SCLC) accounts for up to 16% of lung cancer cases [Citation1]. The main treatment is chemotherapy, and cisplatin plus etoposide is the standard regimen [Citation2,Citation3]. Concurrent thoracic radiotherapy (TRT) improves overall survival (OS) if all lesions can be included in one radiotherapy field (“limited disease” – LD SCLC) [Citation4]. Prophylactic cranial irradiation (PCI) reduces the risk of brain metastases and prolongs survival in those who respond to chemo-radiotherapy [Citation5]. Up to 90% of patients respond to the treatment, but most relapse and die from this disease [Citation2,Citation6].
Several schedules of TRT are being used in LD SCLC, but few comparative trials have been conducted. The most known study, by Turrisi et al., compared twice daily TRT (45 Gy/30 fractions, 3 weeks) with once daily TRT (45 Gy/25 fractions, 5 weeks). Response rates were equal (87%), but twice daily TRT significantly prolonged median OS (23.0 months vs. 19.0 months; p = 0.04) [Citation6]. Thus, twice daily TRT is the most recommended schedule, but not universally adopted [Citation7–11]. Inconvenience of this schedule and concerns about esophagitis are probably the main explanations [Citation10]. Furthermore, the different duration of the schedules (3 vs. 5 weeks) and dissimilar biologically effective doses might have contributed to the OS difference [Citation6]; a systematic overview concluded that shortening the treatment time from start of chemotherapy until completion of TRT was associated with a prolonged OS [Citation12].
A three-week schedule of once daily hypofractionated TRT (40 Gy in 15 fractions) was one of the schedules included in the meta-analysis establishing TRT in LD SCLC [Citation4]. Similar schedules have been used in Norway and other countries [Citation2,Citation9,Citation11,Citation13], but have never been compared with twice daily TRT in a randomized trial. The aims of this study were to compare 45 Gy/30 fractions (twice daily, BID) with 42 Gy/15 fractions (once daily, OD) TRT in LD SCLC with respect to progression-free survival (PFS), OS, toxicity and health-related quality of life (HRQoL). The hypothesis was that the BID regimen would be feasible and improve efficacy without severely increasing toxicity.
Material and methods
Design and approvals
This randomized phase II trial was approved by the Regional Committee for Medical Research Ethics, Central Norway; the Norwegian Social Science Data Services; and the Norwegian Directorate for Health and Social Affairs.
Eligibility criteria and random assignment
A computed tomography (CT) of the chest/upper abdomen, brain magnetic resonance imaging (MRI) and bone scan were conducted within three weeks prior to inclusion. Eligible patients gave written informed consent; were ≥18 years old (no upper limit); had SCLC ineligible for surgery and confined to one hemithorax and the mediastinum, contralateral hilus and supraclavicular regions; measurable disease according to RECIST v1.0 [Citation14]; no other active cancer; no prior chest-radiotherapy; WHO performance status (PS) 0–2; leukocytes ≥3.0 × 109/l, platelets ≥100 × 109/l, bilirubin <1.5 × ULN and creatinine <125 μmol/l. One negative cytology was required if pleural effusion was present.
Patients were randomized to receive TRT of 42 Gy/15 fractions (OD) or 45 Gy/30 fractions (BID) in blocks of eight and stratified for the five Norwegian health care regions.
Chemotherapy
Patients were to receive four courses of cisplatin 75 mg/m2 IV day 1 and etoposide 100 mg/m2 IV days 1–3 every three weeks (PE). A full dose was administered if leukocytes were ≥3.0 × 109/l and platelets ≥100 × 109/l on day 22. Doses were reduced by 25% if leukocytes were 2.5–2.99 × 109/l or platelets 75–99 × 109/l on day 22. At lower leukocyte or platelet counts, courses were postponed. Dose reductions were maintained for subsequent cycles. Use of G-CSF was not recommended. Chemotherapy was discontinued if a course was delayed more than three weeks or a third dose reduction was warranted. Carboplatin was allowed if cisplatin was not tolerated. The use of other agents was not addressed in the protocol.
Radiotherapy
All patients received three-dimensional (3D) conformal TRT five days a week starting between three and four weeks after day 1 of the first PE course. The targets of the TRT were all known pathological lesions plus elective nodal irradiation of lymph node stations 4–7 (bilateral). A planning CT scan was performed within one week prior to TRT. The gross tumor volume (GTV) included all pathological lesions on the baseline scan delineated according to the size on the planning CT scan. The clinical target volume (CTV) included GTV with a 1 cm margin in all directions (CTVtumor) plus the central part of the mediastinum comprising lymph node stations 4–7 (CTVmediastinum). An internal margin (IM) of 1.0 cm was added to the CTVtumor in the transverse plane and 1.0–1.5 cm in the cranio-caudal direction. An IM of 0.5 cm was added to the CTVmediastinum in all directions. Finally, a setup margin was added according to each hospitals routine. Less than 50% of the normal lung tissue should receive more than 20 Gy (V20lung <50%). Other normal tissue constraints were defined and treatment verification was done according to local routines.
A CT response evaluation was conducted three weeks after the last PE course. Patients with a complete or near complete response were offered PCI of 30 Gy/15 fractions starting within six weeks after the CT evaluation.
Endpoints
Primary endpoint was one-year PFS. Secondary endpoints were OS, toxicity and HRQoL (global quality of life, dysphagia and dyspnea).
Evaluation and follow up
All patients were clinically examined and assessed for toxicity before each PE course and weekly during TRT. Response evaluation was performed three weeks after the last PE. Confirmation of response was not required. Post-therapy, patients were followed every eight weeks year 1, every four months year 2–3, and every six months year 4–5. A CT of the chest/upper abdomen was done at each evaluation year 1. Later, a chest x-ray or CT scan (optional) was performed. Progressive disease (PD) was to be confirmed with a CT scan.
Stage of disease was assessed according to TNM v6, response according to RECIST v1.0, and toxicity according to CTCAE v3.0. PFS was defined as time from randomization until PD or death; OS as time from randomization until death.
Patients reported HRQoL using the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire (QLQ) C30 and the lung cancer-specific module LC13. Patients completed the questionnaires at inclusion and at weeks 3, 6, 12, 20, 28 and 52.
Statistical considerations
To detect a 30% improvement in 1 year PFS (from 70% to 91%) from BID TRT with a two-sided alpha of 0.05 and a beta of 0.20, 75 patients were required in each arm. We expected a loss to follow-up of <10% and aimed at enrolling 83 patients in each arm. Patients who received at least one PE course and one fraction of TRT were included in the analyses.
HRQoL scores were calculated according to the QLQ-C30 scoring manual. The clinically relevant minimum difference in mean scores was defined as 10 (on a scale from 0 to 100) [Citation15].
Survival was estimated using the Kaplan-Meier method and compared using the log-rank test. Pearson’s χ2 and Fisher’s exact tests were used for group comparisons. The Cox proportional hazard method was used for multivariate analyses. The level of significance was defined as p < 0.05.
Results
Patients
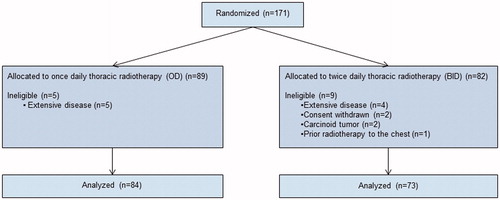
In total 171 patients were enrolled between May 2005 and January 2011 at 18 hospitals in Norway. Fourteen patients were excluded: extensive disease (n = 9), withdrawn consent (n = 2), carcinoid tumor (n = 2), and prior chest radiotherapy (n = 1). Thus, 157 were analyzed (OD: 84 patients, BID: 73) (). The imbalance in number of patients in each arm was due to the block randomization.
Median age was 63 years, 26% were ≥70 years, 52% were men, 84% had PS 0–1, 72% had stage III disease and 11% had cytologically negative pleural fluid. Baseline characteristics were balanced between the arms ().
Table I. Baseline characteristics. Stage of disease was assessed according to TNMv6.
Median follow-up for PFS was 59 months (range 29–97); 34 patients were progression-free when the analyses were performed (July 2013). Median follow-up for OS was 81 months (range 52–119); 34 patients were alive at the time of the analyses (April 2015).
Study therapy
More OD patients completed chemotherapy without delays (OD: 42%, BID: 26%; p = 0.04). There were no other differences in chemotherapy. Fourteen patients received other chemotherapy due to cisplatin toxicity (OD: n = 10, BID: n = 4) ().
Table II. Treatment administered.
The completion rate of TRT was similar (OD: 96%, BID: 97%). Mean doses were OD: 41.8 Gy (range 34–45) and BID: 44.7 Gy (range 30–46). A total of 82% of OD patients and 84% of BID patients received PCI. PCI was omitted in 27 patients due to poor response (n = 21), poor PS (n = 3), patients’ decision (n = 3) and death (n = 1) ().
Response to therapy, PFS and OS
There was no difference in response rates [OD: 92% (95% CI 86–98), BID: 88% (95% CI 80–95); p = 0.41], but more patients on the BID arm achieved a complete response [OD: 13% (95% CI 6–20), BID: 33% (95% CI 22–44); p = 0.003] ().
Table III. Response evaluation three weeks after the last chemotherapy course according to the RECIST-criteria (v 1.0) and toxicity.
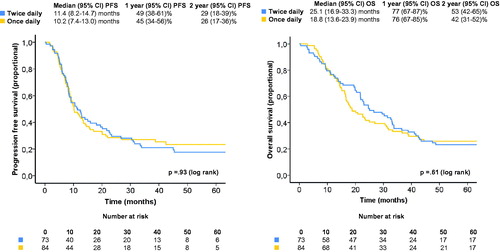
There were no differences in one-year PFS [OD: 45% (95% CI 34–56), BID: 49% (95% CI 38–61); p = 0.61] or median PFS [OD: 10.2 months (95% CI 7.4–13.0), BID: 11.4 months (95% CI 8.2–14.7); p = 0.93] (). There were no significant differences in location of first relapse: distant failures (OD: 47%, BID: 38%; p = 0.33), local failures (OD: 34%, BID: 50%; p = 0.10) or synchronous distant and local failures (OD: 19%, BID: 13%; p = 0.38).
There were no statistically significant differences in one-year OS [OD: 76% (95% CI 67–85), BID: 77% (95% CI 67–87); p = 0.94], two-year OS [OD: 42% (95% CI 31–52), BID: 53% (95% CI 42–65); p = 0.14], four-year OS [OD: 25% (95% CI 16–34), BID: 25% (95% CI 15–35); p = 0.96] or median OS [OD: 18.8 months (95% CI 13.6–23.9), BID: 25.1 months (95% CI 16.9–33.3); p = 0.61] (). The difference in median disease-specific survival was of similar magnitude (OD: 22.6 months, BID: 29.5 months; p = 0.66).
Toxicity
There were no differences in grade 3–4 neutropenic infections (OD: 44%, BID: 37%; p = 0.37), grade 3–4 esophagitis (OD: 31%, BID: 33%; p = 0.80) or grade 3–4 pneumonitis (OD: 2%, BID: 3%; p = 1.0) (). There was no difference in treatment-related deaths (OD: n = 4, BID: n = 3; p = 1.0). Four patients died from radiation pneumonitis (OD: n = 3, BID: n = 1). Three patients died within 30 days of chemo-radiotherapy: hemoptysis (n = 1), coronary disease (n = 1) and respiratory failure (n = 1).
HRQoL
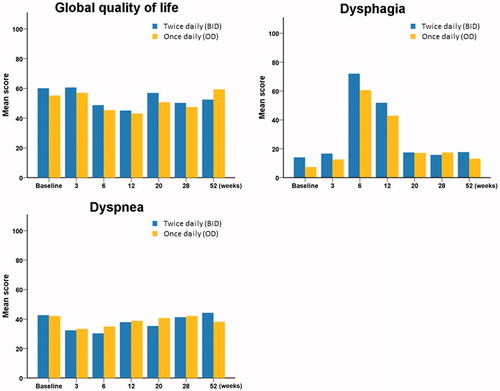
The completion rate of the questionnaires was 85–97% of patients alive at each time point and similar in both arms. Patients in the BID arm experienced more dysphagia at the end of TRT (mean score OD: 61, BID: 72) (). There were no other differences in global QoL, dysphagia, dyspnea or in any other HRQoL domain.
Post-study treatment
Seventy-five patients received second line chemotherapy (OD: 51%, BID: 44%; p = 0.36) (). Re-induction with etoposide plus cisplatin or carboplatin was the most common regimen (37/75 patients; 49%).
PS and stage of disease
All patients were analyzed as one cohort in these explorative analyses. There was no PS-related influence on response rates (PS 0–1: 89%, PS 2: 92%; p = 1.0) or median OS (PS 0–1: 23.0 months, PS 2: 18.8 months; p = 0.32). Patients with stage I–II disease had similar response rates as stage III patients (stage I–II: 86%, stage III: 90%; p = 0.51), but longer median OS (stage I–II: 33.3 months, stage III: 20.4 months; p = 0.024). Elderly patients had similar response rates (<70 years: 91%, ≥70 years: 88%; p = 0.76) and there were no significant differences in median OS (<70 years: 24.6 months, ≥70 years: 14.6 months; p = 0.28). Across genders, there were no differences in response rates (men: 89%, women: 91%; p = 0.69) or median OS (men: 21.7 months, women: 24.7 months; p = 0.53). There were no differences in grade 3–5 esophagitis or pneumonitis across PS, disease stage, age or gender.
The multivariate analysis revealed that stage I–II patients had significantly longer survival than those with stage III (p = 0.026). No other characteristics were significantly associated with PFS or OS.
Discussion
In this RCT comparing two three-week schedules, the twice daily TRT schedule provided significantly more complete responses, but not higher response rates. There were no statistically significant differences in PFS or OS, though the median OS (25.1 vs. 18.8 months) and disease-specific survival (29.5 vs. 22.6 months) were more than six months longer on the BID arm. The BID patients reported slightly more dysphagia immediately after radiotherapy, but a difference in mean score of 10–20 is considered a “moderate change” [Citation15]; they had slightly more dysphagia also before radiotherapy; and patients on both arms regained similar, pre-treatment levels of dysphagia soon after therapy. Thus, there were no differences in severe toxicity or treatment-related deaths. We used a wide definition of limited disease, had no restrictions regarding comorbidity or age and 16% of the patients had PS 2.
We are aware of two other prospective RCTs comparing one and two daily fractions of TRT in LD-SCLC. The split course used by Schild et al. [Citation16] causes longer treatment duration and might enhance repopulation of cancer cells [Citation12]. Thus, it is most relevant to compare our results with the study by Turrisi et al. In this study, TRT of 45 Gy in 30 fractions (BID) was compared with 45 Gy in 25 fractions (OD). All patients received cisplatin plus etoposide. Patients on the BID arm had significantly longer median OS (23.0 vs. 19.0 months; p = 0.04) [Citation6]. The survival difference is of similar magnitude in our smaller study, though not statistically significant. Furthermore, the difference in median OS in our study did not result in a higher proportion of long-term survivors.
Results from other studies might indicate that twice daily regimens are superior to hypofractionated three-week schedules. In two studies, patients on the control arms receiving four courses of cisplatin plus etoposide and TRT of 45 Gy/30 fractions achieved response rates of 95–97%, median PFS of approximately 13 months, and median OS of 25–38 months [Citation17,Citation18]. In studies administering TRT with 40–42 Gy/15 fractions, response rates were 81–85%, median PFS 10.6 months and median OS 13.7–21.2 months [Citation2,Citation11,Citation13]. However, these studies are not necessarily comparable due to differences in patient selection, staging procedures, chemotherapy, timing and schedules of TRT, response evaluation and follow-up.
Turrisi et al. reported more esophagitis grade 3 (27% vs. 11%) but not more grade 4 (5% both arms) in the BID group. We found a similar proportion of grade 3–4 esophagitis in the BID arm (33%), but a higher proportion in our OD arm (31%) – probably due to the higher daily dose. The percentage of deaths from radiation pneumonitis (4%) in the OD arm is higher than in other reports [Citation6,Citation13], but the number was low (n = 3).
PFS was chosen as the primary endpoint since it correlates well with OS in several studies of SCLC and is less influenced by relapse treatment and death of other causes [Citation6,Citation19]. However, using PFS as the primary endpoint can be debated. Distinguishing between relapse and radiation fibrosis in lung tissue is challenging, there was a large number of radiologists involved in this study, and no central review of CT images. However, assessment of progression was done equally in both arms. The delta value in the sample size calculation was rather large, but we considered the sample size adequate to guide directions for future research. Other reasons for limiting the sample size were concerns about toxicity of the BID schedule, as well as concerns about inferiority of the OD schedule.
A limitation of the study is the lack of positron emission tomography (PET)/CT for staging of disease. PET/CT identifies pathological lesions better than CT- and bone-scans [Citation20], allowing for more accurate staging and definition of radiotherapy fields for TRT [Citation21]. These data suggest that elective nodal irradiation can be replaced by irradiation of PET CT positive lesions alone. However, PET/CT was not generally available in Norway at the time when this study was conducted.
Approximately 17% of all patients diagnosed with LD SCLC in Norway during the enrolment period were enrolled in our trial. The enrolment period was still long (six years) and the number of patients enrolled at each hospital was in many cases low (range 1–29, less than one patient per year at 11 of the 18 participating hospitals). We did enroll a higher proportion of PS two patients and the median age was similar as in other LD SCLC studies [Citation6,Citation16,Citation18], but did not record clinical data on patients not enrolled and cannot rule out a selection bias. Furthermore, there are potential quality assurance concerns about the radiotherapy plans at the hospitals with the lowest number of participants, and there might have been changes in radiotherapy techniques applied during the study treatment period.
It is difficult to draw any firm conclusions about efficacy from this phase II trial. The higher rate of complete responses and the longer median OS may indicate superiority of the BID schedule. However, no corresponding difference in PFS was observed, and there was a trend towards more local relapses at first recurrence in the BID arm. Besides, the difference in median OS was not statistically significant, and there were no differences in four-year survival rates. Thus, a phase III study is needed before one can conclude whether the BID schedule is more effective than the OD schedule. Considering the results of the present study, the hypothesis of such a trial should be that BID is superior to OD. A large number of patients would be required, and by conducting such a study, many patients might receive an inferior treatment – which would probably be equally toxic as the BID schedule. Thus, we assume that the relevance of such a trial is limited.
By using PET/CT for target volume definition and advanced radiotherapy techniques, higher TRT doses can be delivered and there are indications that 60–70 Gy in 6–7 weeks may be superior to 45 Gy/30 fractions [Citation22–24]. In line with this, we have initiated a Nordic, randomized phase II trial comparing 45 Gy/30 fractions with 60 Gy/40 fractions. All patients receive two fractions per day. The primary endpoint is two-year survival.
Despite improvements in radiotherapy techniques it may not be possible to deliver 60–70 Gy to all patients with disseminated intra-thoracic disease, severe comorbidity or poor PS. Thus, some patients might receive TRT doses of 40–45 Gy also in the future. Our study indicates that concerns about toxicity should not be a reason for choosing hypofractionated instead of twice daily TRT.
In conclusion, there was no difference in toxicity between the two TRT schedules. The twice daily schedule was feasible and resulted in more complete responses and a numerically longer median OS. There was no difference in PFS, and the survival difference was not statistically significant. Thus, no firm conclusions about efficacy could be drawn from this phase II trial.
Acknowledgments
The study was supported by the Central Norway Regional Health Authority (RHA), the Norwegian University of Science and Technology (NTNU) and the Norwegian Cancer Society. The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Sagerup CM, Smastuen M, Johannesen TB, Helland A, Brustugun OT. Sex-specific trends in lung cancer incidence and survival: A population study of 40,118 cases. Thorax 2011;66:301–7.
- Sundstrom S, Bremnes RM, Kaasa S, Aasebo U, Hatlevoll R, Dahle R, et al. Cisplatin and etoposide regimen is superior to cyclophosphamide, epirubicin, and vincristine regimen in small-cell lung cancer: Results from a randomized phase III trial with 5 years’ follow-up. J Clin Oncol 2002;20:4665–72.
- Murray N, Turrisi III AT. A review of first-line treatment for small-cell lung cancer. J Thorac Oncol 2006;1:270–8.
- Pignon JP, Arriagada R, Ihde DC, Johnson DH, Perry MC, Souhami RL, et al. A meta-analysis of thoracic radiotherapy for small-cell lung cancer. New Engl J Med 1992;327:1618–24.
- Auperin A, Arriagada R, Pignon JP, Le Pechoux C, Gregor A, Stephens RJ, et al. Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic Cranial Irradiation Overview Collaborative Group. New Engl J Med 1999;341:476–84.
- Turrisi III AT, Kim K, Blum R, Sause WT, Livingston RB, Komaki R, et al. Twice-daily compared with once-daily thoracic radiotherapy in limited small-cell lung cancer treated concurrently with cisplatin and etoposide. New Engl J Med 1999;340:265–71.
- Komaki R, Khalid N, Langer CJ, Kong FM, Owen JB, Crozier CL, et al. Penetration of recommended procedures for lung cancer staging and management in the United States over 10 years: A quality research in radiation oncology survey. Int J Radiat Oncol Biol Phys 2013;85:1082–9.
- Uno T, Sumi M, Ishihara Y, Numasaki H, Mitsumori M, Teshima T, et al. Changes in patterns of care for limited-stage small-cell lung cancer: Results of the 99-01 patterns of care study – a nationwide survey in Japan. Int J Radiat Oncol Biol Phys 2008;71:414–9.
- Wzietek I, Suwinski R, Nowara E, Bialas M, Bentzen S, Tukiendorf A. Does routine clinical practice reproduce the outcome of large prospective trials? The analysis of institutional database on patients with limited-disease small-cell lung cancer. Cancer Invest 2014;32:1–7.
- Fruh M, De Ruysscher D, Popat S, Crino L, Peters S, Felip E, et al. Small-cell lung cancer (SCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2013;24(Suppl 6):vi99–105.
- Spiro SG, James LE, Rudd RM, Trask CW, Tobias JS, Snee M, et al. Early compared with late radiotherapy in combined modality treatment for limited disease small-cell lung cancer: A London Lung Cancer Group multicenter randomized clinical trial and meta-analysis. J Clin Oncol 2006;24:3823–30.
- De Ruysscher D, Pijls-Johannesma M, Bentzen SM, Minken A, Wanders R, Lutgens L, et al. Time between the first day of chemotherapy and the last day of chest radiation is the most important predictor of survival in limited-disease small-cell lung cancer. J Clin Oncol 2006;24:1057–63.
- Murray N, Coy P, Pater JL, Hodson I, Arnold A, Zee BC, et al. Importance of timing for thoracic irradiation in the combined modality treatment of limited-stage small-cell lung cancer. The National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 1993;11:336–44.
- Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Instit 2000;92:205–16.
- Osoba D, Rodrigues G, Myles J, Zee B, Pater J. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 1998;16:139–44.
- Schild SE, Bonner JA, Shanahan TG, Brooks BJ, Marks RS, Geyer SM, et al. Long-term results of a phase III trial comparing once-daily radiotherapy with twice-daily radiotherapy in limited-stage small-cell lung cancer. Int J Radiat Oncol Biol Phys 2004;59:943–51.
- Takada M, Fukuoka M, Kawahara M, Sugiura T, Yokoyama A, Yokota S, et al. Phase III study of concurrent versus sequential thoracic radiotherapy in combination with cisplatin and etoposide for limited-stage small-cell lung cancer: Results of the Japan Clinical Oncology Group Study 9104. J Clin Oncol 2002;20:3054–60.
- Kubota K, Hida T, Ishikura S, Mizusawa J, Nishio M, Kawahara M, et al. Etoposide and cisplatin versus irinotecan and cisplatin in patients with limited-stage small-cell lung cancer treated with etoposide and cisplatin plus concurrent accelerated hyperfractionated thoracic radiotherapy (JCOG0202): A randomised phase 3 study. Lancet Oncol 2014;15:106–13.
- Foster NR, Qi Y, Shi Q, Krook JE, Kugler JW, Jett JR, et al. Tumor response and progression-free survival as potential surrogate endpoints for overall survival in extensive stage small-cell lung cancer: Findings on the basis of North Central Cancer Treatment Group trials. Cancer 2011;117:1262–71.
- Brink I, Schumacher T, Mix M, Ruhland S, Stoelben E, Digel W, et al. Impact of [18F]FDG-PET on the primary staging of small-cell lung cancer. Eur J Nucl Med Mol Imaging 2004;31:1614–20.
- Shirvani SM, Komaki R, Heymach JV, Fossella FV, Chang JY. Positron emission tomography/computed tomography-guided intensity-modulated radiotherapy for limited-stage small-cell lung cancer. Int J Radiat Oncol Biol Phys 2012;82:e91–7.
- Salama JK, Hodgson L, Pang H, Urbanic JJ, Blackstock AW, Schild SE, et al. A pooled analysis of limited-stage small-cell lung cancer patients treated with induction chemotherapy followed by concurrent platinum-based chemotherapy and 70 Gy daily radiotherapy: CALGB 30904. J Thorac Oncol 2013;8:1043–9.
- Kalemkerian GP, Akerley W, Bogner P, Borghaei H, Chow LQ, Downey RJ, et al. Small cell lung cancer. J Natl Compr Canc Netw 2013;11:78–98.
- Jett JR, Schild SE, Kesler KA, Kalemkerian GP. Treatment of small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed. American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143(5 Suppl):e400S–19S.