Abstract
Purpose The aim of the study was to test the hypothesis that head and neck cancer (HNC) patients benefit from specialized follow-up (FU), as this strategy ensures timely detection of relapses for successful salvage treatment. This was done by evaluation of the pattern of failure, the temporal distribution of recurrences, and the outcome of salvage treatment in a contemporary cohort of HNC patients.
Methods The study evaluated a cohort of 2062 consecutive patients treated with curative intent at Aarhus University Hospital from 1 January 2000 to 31 December 2013. The database of DAHANCA contained recordings of recurrent disease in 567 patients with primary tumors of the larynx, pharynx, oral cavity, nasal cavity, paranasal sinuses and salivary glands. A review of medical records was performed in order to update and supplement the database.
Results Failures of the 567 patients were primarily in T-site (65%) followed by N-site (36%) and M-site (22%). The vast majority of the first recurrences occurred within the first years after primary treatment; 62%, 82%, and 91% within the first, second and third year, respectively. Totally, 51% were amenable for salvage treatment, and 44% benefited from salvage in terms of a complete response. Permanent tumor control was observed in 128 patients (23%) after one or two salvage attempts. The highest salvage rate was recorded in patients with primary glottic carcinoma (41%) and the lowest among hypopharyngeal cancers (2%). Asymptomatic recurrence was recorded in 12% of all recurrences and this was found to be a positive prognostic factor for disease-specific survival, as they had significantly better outcome after salvage.
Conclusion Our data support the usefulness of specialized FU in terms of early detection of recurrent disease. In particular patients with silent recurrences benefited from early detection, as they had a significantly lower risk ratio of death from primary HNC.
Head and neck cancer (HNC) is a loco-regional disease, primarily managed by surgery or radiotherapy (RT), either alone or in combination. Despite improvements in loco-regional control, a significant proportion of patients will still experience treatment failure. Recurrence rates after potential curative treatment differs considerably depending on the stage and sub-site of the primary tumor. Patients with tumors of the glottic larynx have the best prognosis [Citation1], contrary to hypopharyngeal cancers with high recurrence rates and poor chance of successful salvage [Citation2]. Overall, salvage therapy with curative intent have been shown to be feasible only in about half of the patients with a recurrence, and tumor control obtained in approximately half of the patients undergoing salvage [Citation3–5]. This relatively high success rate is the main argument for an active approach towards early detection of recurrence and an aggressive salvage strategy. Based on the premise that detection of the recurrence in an early stage provides a better outcome and the fact that 80% of all failures appear within three years after initial treatment [Citation6], Danish patients had traditionally been offered a five-year follow-up (FU) according to DAHANCA guidelines. This involves visits with a high frequency during the first couple of years and thereafter a declining number of visits. We have previously evaluated the Danish FU-strategy in two separate studies [Citation7,Citation8]. Few recurrences were found in asymptomatic patients (1 in 99 visits), but patients in general were in need of rehabilitation and management of late effects.
We now hypothesize that in addition to management of sequelae, curatively treated HNC patients benefit from scheduled FU visits, as this strategy ensure timely detection of recurrences for successful salvage. The current study aims to test this hypothesis by describing the pattern of failure, the temporal distribution of recurrences and the outcome of salvage treatment in a contemporary population-based cohort of HNC patients initially treated with curative intent.
Patients and methods
The study evaluated a cohort of 2062 consecutive patients with carcinoma of the head and neck treated with curative intend at Aarhus University Hospital. Patients diagnosed with laryngeal, pharyngeal and oral cavity (OC) tumors were prospectively recorded in the DAHANCA database since 2000, and patients diagnosed with tumors of nasal cavity, paranasal sinuses and salivary glands since 2006 and 2008, respectively. Tumors of thyroid, lip and skin were excluded. Overall, all patients evaluated were treated with curative intention in the period from 1 January 2000 to 31 December 2013. This database contained a wide range of information regarding patient and tumor characteristics, treatment and outcome. Furthermore, the database contained information about all failures (date of recurrence, site, salvage therapy and complications). Multiple recurrences were recorded if present.
Any recurrence of disease recorded in the database was included in the analysis. A review of medical records was performed when needed in order to update and supplement the database, and vital status for all patients was updated on 21 May 2015.
A recurrence of disease was defined as histologically verified malignant tumor cells of same type as the primary tumor found at the site of the primary tumor (T-site), in a regional lymph node (N-site) or as distant metastasis (M-site). In the latter, a histological diagnosis was pursued, but in few cases, only a radiologic diagnosis existed. A re-recurrence was defined as a new recurrence after earlier radical salvage.
The primary treatment of patients was according to DAHANCAs guidelines [Citation6,Citation9]. Overall, pharyngeal and laryngeal tumors were treated with primary accelerated RT and the hypoxic radiosensitizer nimorazole (REF), in addition concomitant chemotherapy with weekly cisplatin was given patients with stage 3 and 4 disease [Citation10]. The treatment of tumors of the OC, nasal cavity, paranasal sinuses and salivary glands were primary surgery for all patients with operable disease. Post-operative irradiation is frequently offered to patients with sino-nasal cancer (except T1 disease) and for OC and salivary gland in the cases of non-radical surgery and/or in cases of highly malignant histology. All patients with inoperable disease were considered for primary curative RT with or without concomitant chemotherapy and nimorazole (to squamous cell carcinomas). Primary neck dissection was in general not part of the planned treatment.
Patients were followed for five years with scheduled visits. First FU attendance was within two months after end of primary therapy and acted as an evaluation of treatment effect. It involved a clinical examination and typically imaging consisting either of computed tomography, positron emission tomography or magnetic resonance scans of the head and neck. Patients with identified residual tumor were offered salvage treatment if judged feasible. The second planned attendance was scheduled five months after ended primary treatment and thereafter regularly for five years. More precisely, every third month within the first year, every fourth month in the second year and twice a year in the third and fourth year and once after completed five years of FU. Earlier FU visits were arranged in case of appearance of new symptoms.
Statistical considerations
Actuarial analysis was done using cumulative incidence curves to outline the distribution of the recurrences in relation to end of primary treatment. Time to death from primary HNC was calculated from the time of first failure to death or censuring. Cumulative estimates were adjusted for competing risk, i.e. death from causes other than primary HNC. The Cox proportional hazards model was used to assess hazard ratios (HR) to estimate the effect of clinical prognostic factors (univariate and multivariate analysis) on disease-specific death (DSD). Censoring occurred at death of other causes or end of the observation period. In the model, we corrected for the following co-variates: age, gender, stage, site and primary treatment of primary tumor and site of failure.
For comparison among groups with respect to dichotomous endpoints (e.g. salvage rates), the χ2-test was used. All tests were two-sided and all p-values below 0.05 were considered significant. All analysis was performed using the STATA 12 software package.
The study was approved by the Danish Data Protection Agency 1-16-02-249-14, and The Regional Ethics Committee concluded that the study was a quality assurance project, and as such did not need formal approval.
Results
The median FU time was 4.7 (range 0.2; 15.3) years calculated from the end of primary treatment. At the time of analysis, 122 patients were alive, of which 89 were without evident disease. Death of primary tumor was recorded in 398 and death of other causes in 47 (other cancers in 17).
Treatment failures were recorded in 567 of the 2062 patients (28%). shows the patient, tumor and failure characteristics. Recurrence rates varied between primary tumor sites from 13% (salivary glands) to 48% (hypopharynx) and among the different primary treatment modalities, with the lowest found in the group treated with primary surgery (22%). Recurrence rates were also higher after primary treatment of stage III–IV tumors, corresponding to 70% of all recorded failures. The failure pattern of the first recurrence is demonstrated in Supplementary Figure 1 (available online at http://www.informahealthcare.com). Recurrences in the site of the primary (T-recurrences) or in the neck (N-recurrences) were dominant and often in combination.
Table I. Patients, tumor and failure characteristics.
Overall clinical course
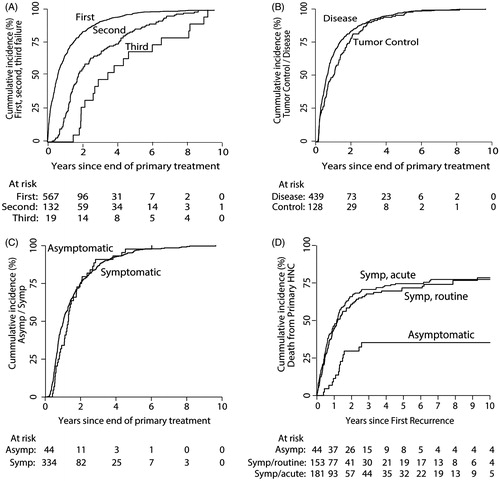
The clinical course of the 2062 patients from radical treatment to either tumor control or failure is illustrated in , with more details given in Supplementary Figures 2–5 (available online at http://www.informahealthcare.com). Of the 567 first recurrences a total of 290 patients underwent salvage. Of these, 248 were completely resected or obtained complete response after salvage RT. Permanent tumor control was achieved in 116 patients (40%). The vast majority of the first recurrence occurred within the first years after primary treatment; 62%, 82% and 91% within the first, second and third year, respectively [ (curve 1)]. A second recurrence was observed in 132 patients, with salvage being attempted in 36 cases and successful in 12 cases. Overall, 128 patients (23%) of all included patients with recurrence achieved permanent tumor control after either the first, second or third recurrence. Palliative treatment or supportive care was offered to 255 and 163 patients, respectively.
Figure 1. Flow chart of the clinical course of the complete cohort of patients treated with curative intent for carcinoma of the head and neck. CR; complete response.
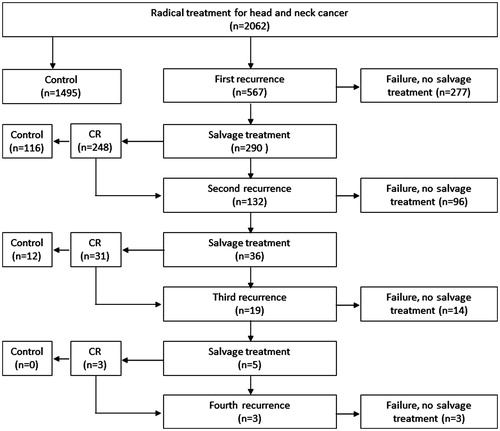
Figure 2. A: Cumulative incidence curves of first, second and third recurrences. B: Cumulative incidence curves illustrating the appearance of recurrences achieving tumor control compared to the recurrences with uncontrolled disease. C: Showing the appearance of asymptomatic recurrences compared to symptomatic recurrences in relation to time since end of primary treatment. D: Showing the cumulative incidence curves (corrected for competing risk) of disease-specific death for symptomatic and asymptomatic recurrences.
Salvage treatment modalities
The salvage treatments consisted mainly of surgery alone (n = 230) or surgery combined with RT in 30 cases. The recorded surgical procedures were mainly laryngectomies and neck dissections (53%). Laryngectomies were primarily performed in laryngeal cancer patients, and surgery of the neck was most often performed in patients with oropharyngeal or OC cancer (Supplementary Table I, available online at http://www.informahealthcare.com). RT as monotherapy was assigned to 30 patients, and these patients had primarily had surgery as their initial treatment (90%) and the main part was previous tumors of the OC.
Pattern of failure after first recurrence
The site of the recurrence was related to the chance of successful salvage. Isolated T-site failures were seen in 271 cases predominantly in glottic larynx and OC. Salvage attempts were initiated in 170 patients (63%) and 78 obtained tumor control, leading to a salvage ratio of 29%. A significantly larger part of initial stage I–II primary tumors gained tumor control after failure compared to failure of initial larger stage tumors (41% vs. 20%) (p < 0.001).
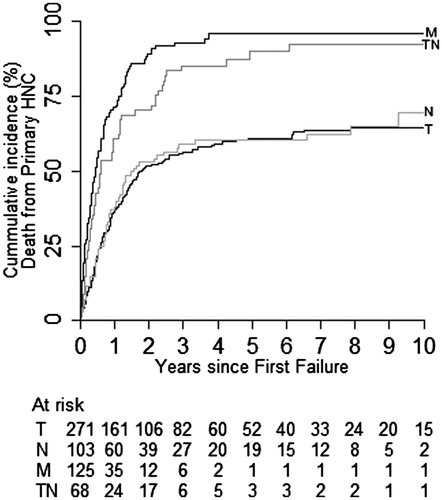
Isolated N-failures were recorded in 103 cases, of which most were from carcinomas of the oropharynx followed by nasal cavity and paranasal sinuses and OC. Curative salvage was offered to 85 patients (83%) and successful in 32 patients (salvage ratio = 31%). A significantly higher proportion of early isolated N-site recurrences (less than three months after end of primary therapy) were successfully salvaged compared to the later ones (50% vs. 26%, p = 0.04). Isolated N-site failure occurred in 28% from primary N0 patients, predominantly primary OC tumors. No difference in salvage ratio was found between failures of initial N0 versus N + tumors. Loco-regional failures (combined T and N) were recorded in 68 cases and 47% of them had originally been treated for a carcinoma of the OC. Curative treatment was feasible in 28 patients, and five patients obtained tumor control (salvage ratio = 7%). In 27%, loco-regional failure occurred in initially N0 patients (72% OC). Combinations involving M-site recurrences (M, TM, NM, TNM) were recorded in 125 patients, seven of them received salvage therapy with curative intent (6%). One patient with a solitary lung metastasis was alive and disease-free at the end of the observation period (SR < 1%).
shows details of the relationship between salvaged recurrences versus the total first-time recurrences. The most successful salvage ratios were found in patients with local failure after treatment of a glottic larynx cancer (48%) and the poorest outcome was in tumors of the hypopharynx and nasopharynx (0%). Among isolated N-site failures, the most successful salvage was after primary oropharyngeal tumors (43%). The stage of the primary tumor was inversely correlated to the probability of successful salvage. This was most pronounced in isolated T-site failures. Finally, patients primarily treated with surgery alone as initial treatment were more likely to obtain tumor control after salvage as opposed to patients treated with surgery and post-operative RT.
Table II. First-time recurrences.
Time after initial treatment
The time of diagnosis of first, second and third recurrence in relation to end of primary treatment is illustrated in . Three years after end of primary treatment 91%, 67% and 47% of the first, second and third recurrences had occurred, respectively. The majority of the first-time recurrences occurred during the first years after primary treatment; 62%, 82% and 91% within first, second and third year, respectively. As mentioned, a significantly higher proportion of early isolated N-site recurrences were successfully salvaged compared to the later ones. illustrates the incidence of recurrences in which tumor control is obtained compared to the ones with uncontrolled disease [HR = 1.2 (1.0; 1.5, p = 0.05)]. The HPV/p16 status of the primary tumor was known in 120 of the 161 patients with oropharyngeal cancer who developed recurrence. The recurrence of 64 HPV/p16 negative oropharyngeal tumors occurred earlier [HR = 1.8 (1.1;2.5), p = 0.01] within the first three years of FU, but no statistical significant difference was found beyond the three years. Neither was there any difference in the frequency of distant metastases between patients with HPV/p16 positive and HPV/p16 negative tumors, respectively. Additionally, we found a significantly higher rate of successful salvage in the HPV/P16 positive group (p = 0.03).
Symptoms and diagnosis of recurrence
Information was available about the clinical course prior to the diagnosis of the first recurrence in 378 patients. Of these, 88% had identified new symptoms prior to the FU visit. For that reason, about half of the symptomatic patients had requested an earlier FU appointment. As seen in , there was no difference in the appearance of the symptomatic and asymptomatic recurrences throughout the FU course. shows a significant difference in DSD between symptomatic and asymptomatic patients [HR = 3.0 (1.9;5.0), p < 0.001]. Multivariate testing revealed that being asymptomatic was a positive prognostic factor for DSD. No significant benefit in terms of DSD was found for patients, who had requested an earlier visit.
The characteristics of asymptomatic cases did not differ significantly from the symptomatic. Thus, we found no significant difference the distribution of patient age, primary tumor, sites of recurrence, primary treatment or the appearance of the recurrences related to end of primary treatment. A significant difference was found in the distribution of the stage of primary tumor; hence, a higher proportion of lower stage primary tumors were found among the group of asymptomatic patients. Furthermore, a significant higher part was amenable for salvage with surgery and a higher proportion had successful salvage.
Pattern of failure after subsequent recurrences
A second recurrence was verified in 132 patients of the 290 patients who underwent successful salvage treatment (46%). Recurrences in T-site were predominant (57%), followed by N-site (36%) and failure combinations involving M-site was recorded in 32%. The second failures in T- and N-site it were re-recurrence in 72% (63/88) and 42% (22/52), respectively. At the time of third recurrence, all the recurrences were in previously involved sites.
The ultimate salvage control for T-site was 26% (120/455) and the corresponding percentage for N-site was 31% (82/267). Those figures were calculated as the part of all obtaining complete response after salvage (first, second and third time) in the site of question and in whom a re-recurrence did not take place divided by the total number of recordings in the particular site.
illustrates DSD after the first recurrence depending on site of failure. A significant different DSD was seen among patients with isolated T- or N-recurrences compared to TN- and M-recurrences. The HRs for TN and M of DSD were increased to 2.1 (1.6; 2.9) and 3.1 (2.5; 4.0), respectively (p < 0.001) compared to DSD of isolated T-site failure. No difference in survival between isolated T- or N-site failures was observed.
Figure 3. The cumulative incidence curves (corrected for competing risk) of disease-specific death for the different failure sites; T: Isolated T-site recurrences, N; Isolated N-site recurrences, TN: Combined loco-regional disease and M: Including all combinations involving distant metastases (M, TM, TNM, NM).
Discussion
The study was undertaken to test the hypothesis that curatively treated HNC patients benefit from scheduled FU visits as this strategy ensure timely detection of relapses and successful salvage. To do so we described the pattern of failures, the temporal distribution of recurrences and the outcome of salvage treatment in a contemporary cohort of HNC patients initially treated with curative intent. We showed that first-time failures predominantly occurred at the site of the primary tumor (65%) whereas this area constituted a lower share in later recurrences where the disease tended to be more disseminated. Furthermore, in tune with existing literature, we found that the vast majority (91%) of the 567 first-time recurrences appeared within three years after primary treatment. These numbers are somewhat higher than earlier reports [Citation5,Citation6,Citation11,Citation12], but confirm that the risk of experiencing a relapse of disease declines considerably after three years. In fact, 62% and 82% appeared after one and two years, respectively.
The earliest recurrences (residual tumor) were predominantly residuals after initial high stage pharyngeal tumors and had a significantly worse survival compared to the later ones, in accordance with other studies [Citation13–17]. In contrast to Huang et al. [Citation18], who found HPV/p16 positive oropharyngeal tumors to develop more frequent (and late) distant metastases, were our findings in agreement with an earlier study of a DAHANCA cohort [Citation19], as we did not find any significant difference in the frequency and pattern of distant metastasis as a function of HPV/p16 status.
The lack of a disease-free interval has been suggested to be a proxy for aggressive disease with a faster growth of tumor or a greater resistance to treatment [Citation20–22]. In addition, treatment options in the cases of recurrent disease are often limited due to extensive primary treatment and patient-related factors, such as performance status and comorbidities. An exception was the earliest isolated N-failures, which had a significantly better salvage ratio compared to the later ones, a finding more extensively investigated in a subset of patients (also included in this series) by Lilja-Fischer et al. [Citation23], and suggesting that a substantial effort should be made in diagnosing these.
Several earlier studies have concluded that FU are incapable of improving survival in HNC by early detection of recurrent disease [Citation16,Citation17]. The results of the current study suggest that a group of patients may have a survival benefit from following a routine FU program. Similar, was also found by de Visscher et al. [Citation24]. The survival is better for asymptomatic compared to symptomatic recurrences, and this group of patients profits from the FU-strategy. These findings do not support the resent speculations of implementing a more symptom-directed FU [Citation25] and the fact that the temporary distribution of the asymptomatic recurrences was widely scattered within the FU period argues against a shortening of the FU period. The fact, that all new recordings of DSD occurred within three years after diagnoses of first recurrence of an asymptomatic recurrence (2D), indicate that the survival benefits is not due to potential lead-time bias.
One of the main objectives of patient education is to enable patients to react on alarm symptoms [Citation8]. In the present study, we investigated whether a survival benefit was found in symptomatic patients bringing their visit forward due to symptoms and found no difference. No data on the time span from the appearance of symptoms to FU visit was available. Thus, no firm conclusion on whether patient education will lead to earlier diagnosis and higher salvage rates can be drawn from this. Interestingly, 54% of the symptomatic patients requested an earlier visit, due to appearance of new symptoms. This was significantly higher than in our previous study, where 35% of symptomatic patients called in for an earlier visit [Citation8].
Surgical salvage is generally regarded as the preferred option for disease control of loco-regional recurrences in patients with a favorable performance status [Citation13], and especially if the patients already had received RT. In this study, the best results were obtained in recurrences after primary glottic larynx cancer and the worst in hypopharyngeal cancer. Successful salvage rates ranged from 8% to 66% (complete response rate) and from 2% to 44% in the group with sustained tumor control, respectively. These figures correlate well with other reports [Citation2,Citation6,Citation13,Citation26,Citation27]. The highest salvage rates were found after recurrence of low stage cancer, tumors treated with primary surgery alone, T-site recurrences appearing later than one year after primary treatment and residual/early nodal tumors. Although tumor control was only temporary in 120 patients, these patients had a significant survival benefit compared to the patients not amenable to salvage after first recurrence.
Despite careful FU, many patients with recurrences are not amenable to surgical salvage, due to previous treatment, the close proximity to vital structures or patient-related factors, such as performance status and comorbidity [Citation13,Citation28]. Extensive salvage surgery can lead to irreversible functional changes (dysphagia, aspiration, dysarthria/loss of voice and change in appearance) and furthermore increases the risk of peri-operative complications, such as reduced wound healing, fistulae and mortality. When salvage treatment is considered, the possible morbidity of the treatments versus the chance of tumor control should be taken into account [Citation21,Citation29].
Re-recurrence in the site of first recurrence was common as 72% of all second T-site failures were re-recurrences and 42% in the N-site, indicating that the salvage treatment was not radical despite negative surgical margins or judgement of complete response to salvage RT. An explanation may be the more infiltrative and multifocal growth pattern of recurrent disease leading to treatment failure, as these small foci were not detectable on imaging or clinical exam [Citation13]. At the end of observation, 128 patients had tumor control corresponding to a successful salvage rate of 23%. The results advocates for an aggressive treatment strategy towards first recurrence of disease in a selected group of patients.
RT alone had limited value in the curatively intended salvage treatment. This may due to the fact that, the majority of the patients initially were treated with RT. Re-irradiation with curative intent increases the degree of toxicity [Citation30]. RT as monotherapy was applied in 10% and additional 10% had surgery combined with RT. In total, 60 patients had curative intended salvage treatment involving RT and the vast majority had OC cancer initially treated with surgery as monotherapy. In 20 patients, RT was a part of both primary and salvage treatment either alone or as post-operative RT. Re-irradiation alone or with concomitant chemotherapy is indicated if the recurrence is inoperable or in case of positive surgical margins. Post-operative re-irradiation has been shown to increase LRC, but no benefit in OS [Citation4,Citation13]. In our study, 7% of all patients undergoing salvage treatment with curative intent after first recurrence had re-irradiation (n = 20), and six were alive and disease-free at the end of analysis period [median FU = 1.7 (0.5; 5.4) years)].
For patients surviving the first three years after therapy without failures there may also be a concern of development of a new primary tumor. We have previously shown that the FU-strategy does not capture new primary tumors, especially not the tumors outside the area of the head and neck [Citation8], as also found by Boysen et al. [Citation11]. This may be due to the fact, that the visit only included a clinical examination of the head and neck region and only imaging and panendoscopy in symptomatic cases.
The study confirmed the hypothesis that patients benefit from FU as more than half of the patients are amenable to salvage treatment and the vast majority of the recurrences appear within three years. On the basis of this and our former studies [Citation7,Citation8], one could consider limiting the FU period to a total of three and a half years, since thereafter less than 10% of new recurrences are expected and as few not previously identified problems occur. A risk assessment prior to terminating of FU may identify the smaller group of patients with problems that needs continued management, but the majority of patients seem to be safely terminated after three and a half years [Citation8,Citation11].
Conclusion
Our data support the usefulness of specialized FU in terms of early detection of recurrent disease. In particular, patients with silent recurrences benefited from early detection as they had a significantly lower risk ratio of death from primary HNC.
Artikel_Supplementary_Material.docx
Download MS Word (967.8 KB)Acknowledgments
Supported by CIRRO – The Lundbeck Foundation Center for Interventional Research in Radiation Oncology and The Danish Council for Strategic Research, Aarhus University and Danish Cancer Society.
Declaration of interest
The authors have declared no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Johansen LV, Grau C, Overgaard J. Glottic carcinoma-patterns of failure and salvage treatment after curative radiotherapy in 861 consecutive patients. Radiother Oncol 2002;63:257–267.
- Johansen LV, Grau C, Overgaard J. Hypopharyngeal squamous cell carcinoma-treatment results in 138 consecutively admitted patients.. Acta Oncol 2000;39:529–536.
- Goodwin WJ. Jr., Salvage surgery for patients with recurrent squamous cell carcinoma of the upper aerodigestive tract: when do the ends justify the means? Laryngoscope 2000;110:1–18.
- Janot F, de Raucourt D, Benhamou E, Ferron C, Dolivet G, Bensadoun RJ, et al. Randomized trial of postoperative reirradiation combined with chemotherapy after salvage surgery compared with salvage surgery alone in head and neck carcinoma. J Clin Oncol 2008;26:5518–5523.
- Jung YH, Song CM, Park JH, Kim H, Cha W, Hah JH, et al. Efficacy of current regular follow-up policy after treatment for head and neck cancer: need for individualized and obligatory follow-up strategy. Head Neck 2014;36:715–721.
- Overgaard J, Hansen HS, Specht L, Overgaard M, Grau C, Andersen E, et al. Five compared with six fractions per week of conventional radiotherapy of squamous-cell carcinoma of head and neck: DAHANCA 6 and 7 randomised controlled trial. Lancet 2003;362:933–940.
- Pagh A, Vedtofte T, Lynggaard CD, Rubek N, Lonka M, Johansen J, et al. The value of routine follow-up after treatment for head and neck cancer. A national survey from DAHANCA. Acta Oncol 2013;52:277–284.
- Pagh A, Grau C, Overgaard J. A longitudinal study of follow-up activities after curative treatment for head and neck cancer. Acta Oncol 2015;54:813–819.
- Bjørndal K, Krogdahl A, Therkildsen MH, Overgaard J, Johansen J, Kristensen CA, et al. Salivary gland carcinoma in Denmark 1990-2005: a national study of incidence, site and histology. Results of the Danish Head and Neck Cancer Group (DAHANCA). Oral Oncol 2011;47:677–682.
- Bentzen J, Toustrup K, Eriksen JG, Primdahl H, Andersen LJ, Overgaard J. Locally advanced Head and Neck cancer treated with accelerated radiotherapy, the hypoxic modifier nimorazole and weekly cisplatinum. Results from the Dahanca 18 phase II study. Acta Oncol 2015;54:1001–1007.
- Boysen M, Lovdal O, Tausjo J, Winther F. The value of follow-up in patients treated for squamous cell carcinoma of the head and neck. Eur J Cancer 1992;28:426–430.
- Haas I, Hauser U, Ganzer U. The dilemma of follow-up in head and neck cancer patients. Eur Arch Otorhinolaryngol 2001;258:177–183.
- Ho AS, Kraus DH, Ganly I, Lee NY, Shah JP, Morris LG. Decision making in the management of recurrent head and neck cancer. Head Neck 2014;36:144–151.
- Gleich LL, Ryzenman J, Gluckman JL, Wilson KM, Barrett WL, Redmond KP. Recurrent advanced (T3 or T4) head and neck squamous cell carcinoma: is salvage possible? Arch Otolaryngol Head Neck Surg 2004;130:35–38.
- Omura G, Saito Y, Ando M, Kobayashi K, Ebihara Y, Yamasoba T, et al. Salvage surgery for local residual or recurrent pharyngeal cancer after radiotherapy or chemoradiotherapy. Laryngoscope 2014;124: 2075–2080.
- Flynn CJ, Khaouam N, Gardner S, Higgins K, Enepekides D, Balogh J, et al. The value of periodic follow-up in the detection of recurrences after radical treatment in locally advanced head and neck cancer. Clin Oncol (R Coll Radiol) 2010;22:868–873.
- Cooney TR, Poulsen MG. Is routine follow-up useful after combined-modality therapy for advanced head and neck cancer? Arch Otolaryngol Head Neck Surg 1999;125:379–382.
- Huang SH, Perez-Ordonez B, Weinreb I, Hope A, Massey C, Waldron JN, et al. Natural course of distant metastases following radiotherapy or chemoradiotherapy in HPV-related oropharyngeal cancer. Oral Oncol 2013;49:79–85.
- Lassen P, Primdahl H, Johansen J, Kristensen CA, Andersen E, Andersen LJ, et al. Impact of HPV-associated p16-expression on radiotherapy outcome in advanced orophaynx and non-oropharynx cancer. Radiother Oncol 2014;113:310–316.
- Pivot X, Niyikiza C, Poissonnet G, Dassonville O, Bensadoun RJ, Guardiola E, et al. Clinical prognostic factors for patients with recurrent head and neck cancer: implications for randomized trials. Oncology 2001;61:197–204.
- Zafereo M. Surgical salvage of recurrent cancer of the head and neck. Curr Oncol Rep 2014;16:386–014. 0386-0.
- Zafereo ME, Hanasono MM, Rosenthal DI, Sturgis EM, Lewin JS, Roberts DB, et al. The role of salvage surgery in patients with recurrent squamous cell carcinoma of the oropharynx. Cancer 2009;115:5723–5733.
- Lilja-Fischer JK, Jensen K, Eskildsen HW, Fink-Jensen V, Nielsen VE. Response evaluation of the neck in oropharyngeal cancer: value of magnetic resonance imaging and influence of p16 in selecting patients for post-radiotherapy neck dissection. Acta Oncol 2015;54:1599–1606.
- de Visscher AV, Manni JJ. Routine long-term follow-up in patients treated with curative intent for squamous cell carcinoma of the larynx, pharynx, and oral cavity. Does it make sense? Arch Otolaryngol Head Neck Surg 1994;120:934–939.
- Manikantan K, Dwivedi RC, Sayed SI, Pathak KA, Kazi R. Current concepts of surveillance and its significance in head and neck cancer. Ann R Coll Surg Engl 2011;93:576–582.
- Lyhne NM, Primdahl H, Kristensen CA, Andersen E, Johansen J, Andersen LJ, et al. The DAHANCA 6 randomized trial: effect of 6 vs 5 weekly fractions of radiotherapy in patients with glottic squamous cell carcinoma. Radiother Oncol 2015;117:91–98.
- Taki S, Homma A, Oridate N, Suzuki S, Suzuki F, Sakashita T, et al. Salvage surgery for local recurrence after chemoradiotherapy or radiotherapy in hypopharyngeal cancer patients. Eur Arch Otorhinolaryngol 2010;267:1765–1769.
- Patel SN, Cohen MA, Givi B, Dixon BJ, Gilbert RW, Gullane PJ, et al. Salvage surgery for locally recurrent oropharyngeal cancer. Head Neck 2015; (E-pub ahead of print) doi: 10.1002/hed.24065.
- Arnold DJ, Goodwin WJ, Weed DT, Civantos FJ. Treatment of recurrent and advanced stage squamous cell carcinoma of the head and neck. Semin Radiat Oncol 2004;14:190–195.
- Wong SJ, Machtay M, Li Y. Locally recurrent, previously irradiated head and neck cancer: concurrent re-irradiation and chemotherapy, or chemotherapy alone? J Clin Oncol 2006;24:2653–2658.
