Abstract
Background This study aims to investigate the long-term effects of structured trismus intervention in patients with head and neck cancer (HNC) and trismus in terms of mouth opening, trismus-related symptoms and health-related quality of life (HRQL).
Material and methods Fifty patients with HNC to receive radiotherapy ± chemotherapy were included in this prospective study along with a matched control group. The intervention group received a 10-week structured exercise with a jaw mobilizing device (TheraBite® jaw device or Engström device). Patients were assessed before and after trismus exercise intervention and at a two-year follow-up. Primary endpoint was maximum interincisal opening (MIO) and secondary endpoints included trismus-related symptoms and HRQL assessed with patient-reported outcome (PRO)-instruments [Gothenburg Trismus Questionnaire (GTQ), European Organization for Research and Treatment of Cancer Core Questionnaire (EORTC QLQ-C30) and the related HNC-specific module the EORTC Head & Neck Questionnaire (EORTC QLQ-H&N35)].
Results The intervention group had a higher MIO at the two-year follow-up compared to the control group (40.5 mm and 34.3 mm, respectively), which was statistically significant. The intervention group also reported less jaw-related problems according to the GTQ and higher functioning as measured by EORTC QLQ-C30 and QLQ-H&N35 compared to the control group.
Conclusion A positive persistent effect of exercise intervention for trismus in HNC patients was found with regard to MIO, trismus-related symptoms and HRQL. Exercise intervention is important in long-term treatment of radiation-induced trismus in HNC patients. The trismus-specific questionnaire, GTQ, is a valuable tool for observing and evaluating trismus over time.
Trismus (restricted mouth opening) is a symptom that affects more than one third (38–45%) of patients treated with radiotherapy for head and neck cancer (HNC) [Citation1–3]. Trismus most often evolves during the first year following completion of radiotherapy [Citation4]. Along with dry mouth, it is one of the symptoms and oral health problems that can be persistent and from which patients suffer many years after treatment [Citation5,Citation6]. Trismus leads to difficulties with chewing, swallowing, pain and poor oral hygiene. Furthermore, trismus can have a negative impact on health-related quality of life (HRQL) especially with regards to social function and social contact [Citation1,Citation5,Citation7].
To date, there is no standardized treatment for radiation-induced trismus. Nevertheless, several methods for the treatment of trismus have been assessed and even though most studies are based on small study populations, current clinical evidence suggests that exercise intervention with a jaw mobilizing device is superior to unassisted exercise or no exercise at all [Citation8–10].
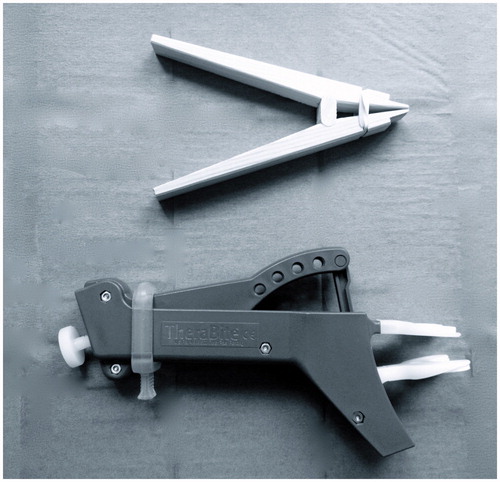
Recent studies have, however, reported that structured exercise intervention with jaw mobilizing devices is efficient and improves mouth opening significantly resulting in improvements in HRQL and less trismus-related symptoms [Citation9,Citation11]. Examples of jaw mobilizing devices are the TheraBite® jaw device, Engström wooden clothespin and the Dynasplint system [Citation11,Citation12].
It is well established that trismus as well as other radiation-induced side effects have a chronic nature, due to the progressive development of tissue fibrosis affecting the temporomandibular joint (TMJ), the muscles of mastication and surrounding tissues. However, up to date, the long-term effect of rehabilitative intervention for radiation-induced trismus has not been studied. Hence, this study aims to investigate the effects of structured trismus intervention in patients with HNC and trismus after two-year follow-up with regard to mouth opening, trismus-related symptoms and HRQL.
Materials and methods
Subjects
Patients with newly diagnosed HNC between 2007 and 2012, from five medical centers serving the region of Western Sweden, were identified at the weekly multidisciplinary tumor board meeting at the Sahlgrenska University Hospital. Inclusion criteria were radiation therapy with or without chemotherapy and no surgical treatment. Tumor locations expected to develop trismus were included, i.e. the oropharynx, oral cavity, the nasopharynx and patients with tumor colli. Patients with poor general health, difficulties in filling out questionnaires and edentulous patients were excluded. Patients residing in Gothenburg underwent regular clinical evaluation by one single oral surgeon and those who developed trismus were invited to participate in a 10-week intervention program.
The control group was comprised of patients living outside the Gothenburg catchment area and was matched according to gender, tumor location, and were comparable for tumor stage, comorbidity, radiation dose and were comparable for age. The control group followed the standard regional hospital schedule for follow-up visits according to the local guidelines, which included regular maximum interincisal opening (MIO) measurements by the local hospital dentist. No structured exercise program addressing trismus existed in the region during the time period but any attempt of improving the mouth opening, structured or otherwise, was registered by the study coordinator.
Endpoints and assessment
The primary endpoint in this study was MIO (measured in millimeters) and secondary endpoints were trismus-related symptoms and HRQL assessed by patient-reported outcome (PRO)-instruments [Gothenburg Trismus Questionnaire (GTQ), the European Organization for Research and Treatment of Cancer Core Questionnaire (EORTC QLQ C30) and the related HNC-specific module the EORTC Head and Neck Questionnaire (EORTC QLQ H&N35)]. Patients were assessed before and after trismus exercise intervention and at a two-year follow-up. The patients’ comorbidity was assessed according to the Adult Comorbidity Evaluation 27 (ACE-27) [Citation13]. Tumors were classified and staged according to the TNM system of classification of malignant tumors determined by the Union for International Cancer Control [Citation14].
Maximum interincisal opening
The criterion for trismus being a MIO ≤35 mm as suggested by Dijsktra et al. was used in this study [Citation15]. MIO was measured using a ruler with the patient sitting in an upright position. MIO was measured as the maximal distance between the edges of the incisors of the mandible and the maxilla, expressed in millimeters.
Trismus intervention
The trismus intervention consisted of structured exercise with a jaw mobilizing device. The devices used in this study were the TheraBite® jaw device (Atos Medical AB) and the Engström device (). All patients in the intervention group received written and oral instructions as well as a demonstration of the device. The patients were instructed to start the exercise with warm up movements and stretch 30 seconds (if possible) using a jaw mobilizing device, five times daily. The exercise consisted of active, (bite towards resistance) and passive, (stretch) movements of the jaw. During the program an oral surgeon evaluated the patients with measurement of MIO after four weeks, 10 weeks, and three months after intervention commencement and additionally after two years.
The exercises were initiated by the oral surgeon and patients carried out the exercise at home. All patients filled out exercise diaries with information on exercise frequency, any adverse effect of exercise or other reasons for exercise cancelation or divergence from the original program. Patients were instructed to gradually increase the intensity of exercise. All measurements in the intervention group were performed by the same oral surgeon. The detailed steps of this exercise program have been described previously [Citation9,Citation11].
Patient-reported outcome
Gothenburg trismus questionnaire
The GTQ is a trismus-specific self-administered questionnaire, which is well accepted by patients and has shown good validity and reliability [Citation16]. It is composed of three domains containing 13 items: jaw-related problems (six items), eating limitations (four items) and muscular tension (three items). The remaining eight items are retained as single items. The domains and single items range from 0 to 100, where 100 equates to maximum symptomatology and 0 represents no symptoms [Citation16].
EORTC QLQ C30 and EORTC QLQ H&N35
The EORTC QLQ C30 is a cancer-specific questionnaire that assesses HRQL in cancer patients. For functional domains and the global quality of life domain, scores range from 0 to 100 where a high score is equal to a high level of functioning or a high level of global quality of life. For single items, the scores also range from 0 to 100, but a higher score is indicative of a higher symptom burden [Citation17]. The EORTC QLQ H&N35 is a head and neck-specific questionnaire designed to assess the quality of life in HNC patients in conjunction with the general cancer-specific EORTC QLQ C30. It consists of 35 items. Scores range from 0 to 100 where high scores equal a high level of symptoms [Citation18].
Statistical methods
For comparison between groups Fisher’s exact test was used for dichotomous variables and the Mantel-Haenszel χ2 exact test was used for ordered categorical variables and χ2 exact test was used for non-ordered categorical variables. For comparison between groups the Mann-Whitney U-test was used for continuous variables. Continuous variables are reported using mean and confidence intervals. All tests are two-tailed and conducted at 5% significance level. The study dimension was established based on a sample size calculation with a significance level of 5% and a power of 80%. In order to detect at difference of 5 mm in MIO between the groups a total of 46 patients was needed.
Ethics
The study was approved by the Regional Ethical Review Board at Gothenburg University (Dnr 287-04, 721-07) and performed in accordance with the Declaration of Helsinki. All participants gave their informed consent to participate in the study.
Results
Patient characteristics
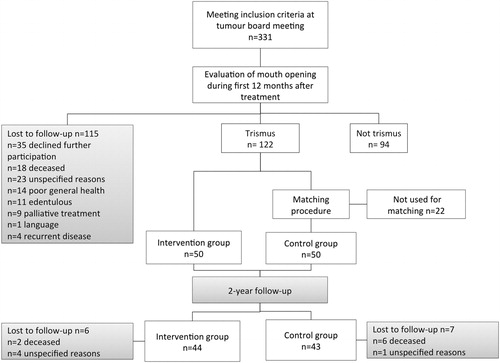
Patient characteristics are presented in . Patients were included as soon as they developed trismus (MIO ≤35 mm), i.e. 3–6 months from radiotherapy completion for both the intervention group and control groups. At the two-year follow-up, six patients in the intervention group (n = 2 deceased, n = 4 unspecified) and seven patients in the control group (n = 6 deceased, n = 1 unspecified) were lost to follow-up (). In the intervention group 9% (four) were unemployed, 28% (13) retired and, 63% (29) in active work. Corresponding figures for the control group were 4% (two) unemployed, 40% (19) retired and, 56% (26) in active work.
Table 1. Patient characteristics in the intervention group and the control group at start of study.
A majority of the patients in the intervention group, 88% (32/44), reported continued exercise at the two-year follow-up. In the control group 16% (7/43) reported some type of jaw exercise at the two-year follow-up. Amongst the patient that exercised, the mean amount of exercise was twice daily in the intervention group and 1.3 times/day in the control group (data not shown).
Maximum interincisal opening
The intervention group had a higher MIO at the two-year follow-up compared to the control group (40.5 mm and 34.3 mm, respectively). This difference was statistically significant as seen in . There were no statistically significant differences in MIO between the patients that had used the Engström jaw device (40.4 mm) and the TheraBite jaw device (40.7 mm).
Table 2. MIO, mean value, 95% confidence interval (CI) for HNC patients before and after intervention and at 2-year follow-up.
Patient-reported outcome
Gothenburg trismus questionnaire
At the two-year follow-up, the intervention group reported less jaw-related problems, eating limitations, muscular tension and facial pain compared to the control group, which was statistically significant (). When analyzing the mean change in score between the groups from baseline to after intervention and from baseline to the two-year follow-up the intervention group reported statistical significant improvement in all main domains and single items (Supplementary Table 1, available online at http://www.informahealthcare.com).
Table 3. GTQ-score for HNC patients before and after trismus intervention and at 2-year follow-up.
EORTC QLQ C30 and H&N35
At the two-year follow-up, the patients in the intervention group had significantly higher scores and thus better functioning levels in three of the domains (role functioning, social functioning, global quality of life) compared to the control group (). Furthermore, the intervention group reported statistically fewer problems with speech, teeth and opening mouth compared to the control group at the two-year follow-up. Both groups reported reduced pain problems at the two-year follow-up compared to the intervention start. However, the control group reported clinically significantly more problems with pain than the intervention group (). When analyzing the mean change in score between the groups from baseline to after intervention and from baseline to the two-year follow-up the intervention group reported statistical significant improvements in all functional scales of the EORTC QLQ C30 and fewer problems with pain, swallowing, social eating, social contact, teeth, opening mouth and, feeling ill according to the EORTC QLQ HN 35 (Supplementary Table 2 and III, available online at http://www.informahealthcare.com).
Table 4. EORTC QLQ C30-score for HNC patients before and after intervention and at 2-year follow-up.
Table 5. EORTC QLQ H&N35-score for HNC patients before and after intervention and at 2-year follow-up.
Discussion
In this prospective study on the treatment of radiation-induced trismus in HNC it was shown that the positive effect of structured exercise intervention was persistent at the two-year follow-up both with regard to improved mouth opening (MIO), less trismus-related symptoms and improved HRQL.
Trismus is undoubtedly an important problem for HNC patients treated with radiotherapy. A recent study demonstrated that more than 10 years after receiving radiotherapy, patients with HNC had substantial problems both with mouth opening and swallowing [Citation6]. It is well known that trismus results in functional interference with oral hygiene, speech and nutritional intake. This subsequently contributes to difficulties in obtaining adequate dental treatment, potential weight loss and malnutrition. These factors may have a negative impact on the quality of life and may increase the risk of depression [Citation3,Citation19,Citation20]. Furthermore, a limitation in mouth opening can interfere with social activities and the ability to work [Citation1,Citation21].
Our data reveals that an improvement in mean mouth opening of 6.2 mm seem to be of clinical importance for the patients given the clear connection to improved functioning as described in the PROs. Earlier studies supports that a difference in mouth opening of at least 5 mm can be interpreted as clinical relevant and not the result of inter-rater differences in measurement technique or normal variation [Citation22].
Even though 6 mm might seem like a small improvement our data suggests the opposite. In an everyday context an improvement of 6 mm in mouth opening can for some patients be the difference between being able to use a spoon instead of a straw to eat soup or being able to brush the teeth.
In this study it was demonstrated that aside from improved mouth opening, the intervention group consistently reported less problems with pain, eating limitation, jaw-related problems, problems with teeth, and a better physical functioning and global quality of life than the control group.
One could argue that some of these improvement in HRQL could be attributed the natural course of gradual recovery during the first two years after oncological treatment. However, neither could we find that pattern in the control group nor detect any other factors, such as socioeconomic status or comorbidity, that could explain the differences between the two groups. Hence, the results indicate that structured exercise therapy has a long-term positive effect on both social and work-related functioning, as well as on the patients’ global health status. Furthermore, the results suggest that trismus and trismus-related symptoms can be treated or at least substantially ameliorated with structured exercise intervention using jaw mobilizing devices. Nevertheless, as can be expected from earlier studies, our data reveals that the HNC patients suffer substantially from problems with dry mouth, sticky saliva, and swallowing at the two-year follow-up.
It is clear that rehabilitative and prophylactic interventions’ focusing on swallowing and oral health needs further studying and developing to improve the situation for HNC patients in the long-term perspective.
Earlier research has shown that compliance to exercise can be a problem especially when it comes to prophylactic interventions, i.e. exercise interventions that are initiated prior to radiotherapy start and onset of symptoms [Citation23]. In a previous report on exercise intervention in patients with radiation-induced trismus, it was found that most patients exercised three times per day as opposed to the suggested five times per day in that study protocol [Citation11]. At the two-year follow-up, data showed that a majority (88%) of the patients in the intervention group continued to exercise after the end of the intervention program. The fact that many patients still exercised as frequently was somewhat unexpected and could be interpreted as depending on the patients experiencing a positive effect of exercise. This has previously been highlighted as one of the factors, together with support and encouragement which is of great importance for the adherence to exercise for the treatment of trismus with jaw mobilizing devices [Citation24].
The natural course of radiation-induced side effects in HNC often includes a progressive loss of normal tissue and the gradual development of fibrosis [Citation25].
In the case of trismus there is a risk of mastication muscle contracture and atrophy, and TMJ fibrosis resulting in reduced mandibular range of motion. A rational to why exercise intervention for trismus have a positive effect if performed on a regular basis is that activation of the muscles of mastication and stretching of the TMJ can counteract shortening of muscles, maintain circulation and increase the range of motion of the TMJ.
Hence, this suggests that regular exercise is important in order to maintain mouth opening capacity and also that regular follow-up and MIO assessment is important to maintain patient motivation for continued exercise, thereby further reducing trismus-related symptoms and improving HRQL.
The GTQ has previously proved useful as an endpoint for trismus and trismus-related symptoms in clinical trials [Citation1,Citation16]. The use of both an objective endpoint for trismus (MIO) and a subjective, PRO (GTQ) is valuable in order to detect both patients in need of, and the perceived effect of rehabilitative measures, such as exercise intervention.
The strengths of this study were its prospective design as well as the use of both objective measurement of mouth opening (MIO) and PRO assessing HRQL. This is to our knowledge the first prospective, long-term study including both entities. Furthermore, few patients were lost to follow-up despite this being a common problem in HNC studies. The patients’ demographic data correspond seemingly well to other studies in this field. A study limitation is the risk of selection bias due to the non-randomised controlled trial design. However, this potential risk was limited by the matching procedure for the control group.
Future implications
In order to improve HRQL in HNC patients with radiation-induced trismus, early identification is of great importance in order to treat and minimize the effect of trismus. Following the results from this study, the authors propose that structured exercise therapy may counteract the negative effects of radiation-induced trismus also in the long-term perspective.
Conclusion
In this prospective, two-year follow-up intervention study on trismus in a HNC population, the positive effect of exercise intervention was found to be persistent both in terms of mouth opening, trismus-related symptoms and HRQL. It is clear that exercise intervention is important in the long-term treatment of radiation-induced trismus in patients with HNC. The trismus-specific questionnaire, GTQ, is a valuable tool for observing and evaluating trismus over time.
Acknowledgements
This study was supported by the Swedish Cancer Society, the Research and Development Council (FoU), Västra Götaland County, Sweden, the Assar Gabrielsson Foundation Göteborg and the Medical Faculty of Gothenburg University Sweden.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Pauli N, Johnson J, Finizia C, Andrell P. The incidence of trismus and long-term impact on health-related quality of life in patients with head and neck cancer. Acta Oncol 2013;52:1137–45.
- Johnson J, van As-Brooks CJ, Fagerberg-Mohlin B, Finizia C. Trismus in head and neck cancer patients in Sweden: incidence and risk factors. Med Sci Monitor Int Med J Exp Clin Res 2010;16:CR278–82.
- Louise Kent M, Brennan MT, Noll JL, Fox PC, Burri SH, Hunter JC, et al. Radiation-induced trismus in head and neck cancer patients. Support Care Cancer 2008;16:305–9.
- Wang C-J, Huang E-Y, Hsu H-C, Chen H-C, Fang F-M, Hsiung C-Y. The degree and time-course assessment of radiation-induced trismus occurring after radiotherapy for nasopharyngeal cancer. Laryngoscope 2005;115:1458–60.
- Abendstein H, Nordgren M, Boysen M, Jannert M, Silander E, Ahlner-Elmqvist M, et al. Quality of life and head and neck cancer: a 5 year prospective study. Laryngoscope 2005;115:2183–92.
- Kraaijenga SA, Oskam IM, van der Molen L, Hamming-Vrieze O, Hilgers FJ, van den Brekel MW. Evaluation of long term (10-years+) dysphagia and trismus in patients treated with concurrent chemo-radiotherapy for advanced head and neck cancer. Oral Oncol 2015;51:787–94.
- Weber C, Dommerich S, Pau HW, Kramp B. Limited mouth opening after primary therapy of head and neck cancer. Oral Maxillofac Surg 2010;14:169–73.
- Buchbinder D, Currivan RB, Kaplan AJ, Urken ML. Mobilization regimens for the prevention of jaw hypomobility in the radiated patient: a comparison of three techniques. J Oral Maxillofac Surg 1993;51:863–7.
- Pauli N, Fagerberg-Mohlin B, Andrell P, Finizia C. Exercise intervention for the treatment of trismus in head and neck cancer. Acta Oncol 2014;53:502–9.
- Kamstra JI, Roodenburg JL, Beurskens CH, Reintsema H, Dijkstra PU. TheraBite exercises to treat trismus secondary to head and neck cancer. Support Care Cancer 2013;21:951–7.
- Pauli N, Andréll P, Johansson M, Fagerberg-Mohlin B, Finizia C. Treating trismus - a prospective study on effect and compliance to jaw exercise therapy in head and neck cancer. Head Neck 2015;37:1738–1744
- Stubblefield MD, Manfield L, Riedel ER. A preliminary report on the efficacy of a dynamic jaw opening device (dynasplint trismus system) as part of the multimodal treatment of trismus in patients with head and neck cancer. Arch Phys Med Rehabil 2010;91:1278–82.
- Piccirillo JF, Tierney RM, Costas I, Grove L, Spitznagel EL. Prognostic importance of comorbidity in a hospital-based cancer registry. JAMA 2004;291:2441–7.
- International Union Against Cancer (UICC) TNM Classification of Malignant Tumors. 7th ed., G.M. Sobin LH, Wittekind Ch, eds. Wiley-Blackwell: Oxford UK, 2009.
- Dijkstra PU, Huisman PM, Roodenburg JL. Criteria for trismus in head and neck oncology. Int J Oral Maxillofac Surg 2006;35:337–42.
- Johnson J, Carlsson S, Johansson M, Pauli N, Ryden A, Fagerberg-Mohlin B, et al. Development and validation of the Gothenburg Trismus Questionnaire (GAQ). Oral Oncol 2012;48:730–6.
- Bjordal K, de Graeff A, Fayers PM, Hammerlid E, van Pottelsberghe C, Curran D, et al. A 12 country field study of the EORTC QLQ-C30 (version 3.0) and the head and neck cancer specific module (EORTC QLQ-H&N35) in head and neck patients. EORTC Quality of Life Group. Eur J Cancer 2000;36:1796–807.
- Bjordal K, Hammerlid E, Ahlner-Elmqvist M, de Graeff A, Boysen M, Evensen JF, et al. Quality of life in head and neck cancer patients: validation of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-H&N35. J Clin Oncol 1999;17:1008–19.
- Johnson J, Johansson M, Rydén A, Houltz E, Finizia C. The impact of trismus on health-related quality of life and mental health. Head Neck 2015;37:1672–1679.
- Steiner F, Evans J, Marsh R, Rigby P, James S, Sutherland K, et al. Mouth opening and trismus in patients undergoing curative treatment for head and neck cancer. Int J Oral Maxillofac Surg 2015;44:292–6.
- Lee R, Slevin N, Musgrove B, Swindell R, Molassiotis A. Prediction of post-treatment trismus in head and neck cancer patients. Br J Oral Maxillofac Surg 2012;50:328–32.
- Jager-Wittenaar H, Dijkstra PU, Vissink A, van Oort RP, Roodenburg JL. Variation in repeated mouth-opening measurements in head and neck cancer patients with and without trismus. Int J Oral Maxillofac Surg. 2009;38:26–30.
- Høgdal N, Juhl C, Aadahl M, Gluud C. Early preventive exercises versus usual care does not seem to reduce trismus in patients treated with radiotherapy for cancer in the oral cavity or oropharynx: A randomised clinical trial. Acta Oncol 2015;54:80–87.
- Melchers LJ, Van Weert E, Beurskens CH, Reintsema H, Slagter AP, Roodenburg JL, et al. Exercise adherence in patients with trismus due to head and neck oncology: a qualitative study into the use of the Therabite. Int J Oral Maxillofac Surg 2009;38:947–54.
- Stubblefield MD. Radiation fibrosis syndrome: neuromuscular and musculoskeletal complications in cancer survivors. J Injury Funct Rehabilitat 2011;3:1041–54.