To the Editor,
Concomitant radio-chemotherapy is the standard treatment for locally advanced non-small cell lung cancer (NSCLC), with a five-year survival of only approximately 15–20% [Citation1]. Several clinical studies have indicated a positive dose-response relationship with an improved survival with higher dose [Citation2,Citation3]. However, evidence of mediastinal toxicity is accumulating: The phase III dose escalation trial RTOG 0617 [Citation4] showed that heart dose parameters were correlated to death in a multivariate analysis and in a dose escalation trial by Cannon et al. [Citation5] serious late toxicity from central and perihilar structures was encountered. In breast cancer radiotherapy a large population-based case-control study showed an increased risk of major cardiac events with increasing heart dose [Citation6].
During deep inspiration breath-hold (DIBH), the lungs are inflated and the heart displaced caudally and these anatomical changes can be exploited to achieve a lower radiation dose to the intra-thoracic normal tissue. Several reports have shown that DIBH radiotherapy (RT) is a feasible alternative and has the potential of decreasing the lung dose in conventional three-dimensional conformal radiotherapy (3D-CRT) [Citation7–9] and also with volumetric modulated arc therapy (VMAT) [Citation10]. Furthermore, DIBH RT does not acquire a lot of time [Citation11] or economical resources for implementation.
We previously reported preliminary results from the first 10 patients included in this study and found a statistically significant reduction of mean lung dose with DIBH 3D-CRT as well as with VMAT in patients with locally advanced NSCLC [Citation12]. The combination of DIBH and VMAT reduced these parameters further and DIBH mitigated the low dose bath induced by VMAT.
Most previous studies have focused on dose to the lungs and none of them have reported on dose to bronchi and trachea. In this final report, we examine if DIBH-VMAT holds potential to decrease doses to mediastinal organs at risk (OAR) compared to free breathing (FB) VMAT.
Material and methods
Seventeen patients with locally advanced NSCLC were included prospectively from April 2012 to September 2013. Inclusion criteria were ability to perform a voluntary breath-hold for 20 seconds and to follow the audio-visual coaching instructions. All patients were treated in FB. The delineations and treatment planning was performed retrospectively. The study was approved by the local ethical committee (H-2-2011-153). Patient characteristics are listed in Supplementary Table 1S (available online at http://www.informahealthcare.com).
The patients were audio visually coached to hold their breath at a comfortable level of deep inspiration for 20 seconds at a time during a 15-minute session. The Real-time Position ManagementTM system (Varian® Medical Systems) was used to track and record the respiratory signal. The planning procedure included a FB positron emission tomography (PET)/computed tomography (CT) (with 18-Fluorodeoxyglucose tracer), a respiration correlated CT (4D-CT) and three consecutive audio-visual coached DIBH-CT scans (for registration of intra-fraction variation). The mid-ventilation phase (MidV) [Citation13] of the 4D-CT was selected for the FB plan and the first acquired DIBH-CT for the DIBH plan.
To minimize observer variations, the gross tumor volume (GTV) delineations were performed after a strict protocol, with the same radiologist contouring on both the MidV and the DIBH-CT for each patient within the same contouring session. The full PET/CT and the pathology report were available to help decision making on which lymph nodes to include in the GTV. The clinical target volumes (CTV) were delineated by an oncologist adding a 0.5 cm margin to the GTV and adjusted to natural anatomical boundaries. The heart, lungs, esophagus, trachea, large bronchi and spinal cord were defined as OAR and delineated for each patient on both scans within the same session. Planning target volume (PTV) margins were calculated as described by Josipovic et al. For FB they ranged from 5–9 mm, depending on tumor motion [Citation14]. For DIBH they were population-based [Citation15]: 5 mm in cranio-caudal, 6 mm in anterio-posterior and 4 mm in left-right direction.
The prescribed dose was 66 Gy in 33 fractions. All treatment planning was performed by the same physicist in Eclipse™ using RapidArc™ VMAT, calculated with the Analytical Anisotropic Algorithm (AAA) version 11 (all Varian Medical Systems). For each patient a FB plan (FB-VMAT) and a DIBH plan (DIBH-VMAT) were created. The plans consisted of two arcs and were optimized with respect to the spinal cord, PTV coverage, lungs and heart constraints (in decreasing order of priority). The optimization and mechanical criteria for each patient’s two plans were kept identical. Dose constraints were: spinal cord <45 Gy, PRV spinal cord <50 Gy, lung mean dose (MD) <20 Gy, lung volume minus GTV receiving more than 20 Gy (lung V20) <35%, esophagus <66 Gy (allowing 1 cm3 to receive up to 70 Gy), heart volume receiving more than 50 Gy (heart V50) <20% and heart MD <45 Gy. A senior oncologist and a senior medical physicist reviewed all plans. Statistical analyses were performed with SPSS, version 19.0 (IBM). Median (range) are given unless otherwise stated. Wilcoxon signed-rank test was used for comparison of group medians and simple linear regression was used for correlation tests. A two-sided significance level of p < 0.05 was applied.
Results
Median lung volume increased in DIBH by 60% (35–108%) compared with FB (p < 0.001). There was a significant difference in median GTV, CTV and PTV size between FB and DIBH plans (). There were no significant differences in PTV, CTV or GTV coverage between DIBH-VMAT and FB-VMAT and all plans fulfilled the dose coverage criteria.
Table 1. Target sizes and estimated doses to organs at risk.
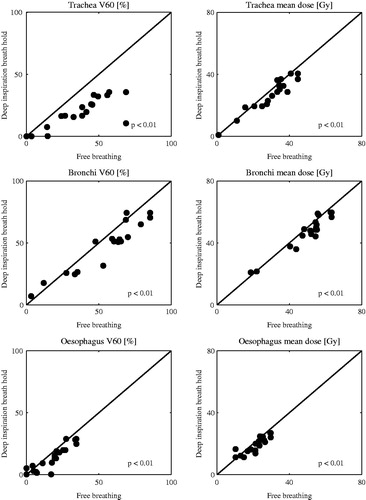
Overall DIBH significantly reduced high dose volumes and MD to trachea, bronchi and esophagus, the heart’s low dose volume and MD and all lung dose parameters (). With DIBH the median heart MD was reduced from 8.5 to 5.7 Gy with reductions up to 5.7 Gy, median esophagus MD from 23.0 to 19.9 Gy with reductions up to 7.5 Gy, median bronchi V60 from 60.5% to 51.2% with a maximum reduction of 21% and median trachea V60 from 38.5% to 16.6% with a maximum reduction of 58.3%. Lung MD was reduced from 15.7 Gy to 12.2 Gy with a maximum reduction of 4.9 Gy. The dose parameters in FB versus DIBH of the esophagus, bronchi and trachea are plotted in . The corresponding figures for heart- and lung dose parameters is plotted in Supplementary Figure 1S (available online at http://www.informahealthcare.com).
Figure 1. Plots of evaluated esophageal-, tracheal- and bronchial dose parameters in free breathing (FB) and deep inspiration breath hold (DIBH).
There were no statistically significant correlations between DIBH PTV size and esophagus, bronchi- and heart dose parameters. Likewise, we found no pattern in benefit – or lack of it – regarding doses to OAR between left, right or central tumors or between upper and lower lobe tumors in this group of patients.
Discussion
In this study we showed that DIBH-VMAT decreased heart MD and V5, as well as bronchi, trachea and esophagus MD and high dose volumes, compared to FB-VMAT. GTV was significant smaller in DIBH compared to FB, probably reflecting the fewer artifacts in the DIBH scan compared to the MidV scan used for FB planning [Citation16].
Earlier studies on DIBH in lung cancer RT reported a 15–30% decrease in lung dose parameters, approximately 15% reduction in heart dose parameters and 10% decrease in esophagus dose parameters [Citation7–9,Citation17–19]. Marchand et al. [Citation8] found a significant reduction with DIBH compared to FB in both heart MD (from 16.7 to 13.6 Gy) and esophagus MD (from 30.1 to 27.9 Gy). The magnitude of these doses is substantially larger than in our study (), probably reflecting the larger high dose volumes caused by the lower conformity of treatment planning with 3D-CRT techniques compared to VMAT. Ottosson et al. [Citation10] used DIBH-VMAT and found dose reductions in the same magnitude as in our study.
We have previously reported a patient case where the DIBH technique resulted in a much higher lung dose compared to FB, caused by separation of the mediastinal and the lower lobe tumors, resulting in a larger PTV in DIBH [Citation20]. Therefore, it is possible that the benefit of DIBH will be smaller for patients with both lower lobe tumors and mediastinal lymph node metastases. We found a large variation in the difference between DIBH and FB on planned heart- and lung dose, probably because of heterogeneity with regard to size and localization of the tumors. We therefore recommend that treatment plans for both FB and DIBH are made for each patient and that the overall best plan is chosen for the treatment.
The combination of DIBH and VMAT may, better than FB RT, facilitate dose escalation to target volumes or subvolumes. In a treatment planning study including 28 patients with lung cancer, target doses could be escalated with DIBH RT without increasing the risk of toxicity compared to FB RT [Citation21].
To conclude, RT in DIBH delivered with VMAT has the potential of decreasing the estimated doses to the heart, lungs, esophagus, and bronchial structures and may facilitate a dose escalation to target volumes or subvolumes, without an increase in toxicity.
Figure_1S.zip
Download Zip (20.5 KB)Acknowledgments
Gitte Fredberg Persson has received a grant from the Danish Cancer Society. Marianne Aznar and Mirjana Josipovic has received a grant from Varian Medical Systems. The research was supported by a grant from the Danish Cancer Society (grant number R90-R6009-14-S2).
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Auperin A, Le Pechoux C, Rolland E, Curran WJ, Furuse K, Fournel P, et al. Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non-small-cell lung cancer. J Clin Oncol 2010;28:2181–90.
- Kong FM, Ten Haken RK, Schipper MJ, Sullivan MA, Chen M, Lopez C, et al. High-dose radiation improved local tumor control and overall survival in patients with inoperable/unresectable non-small-cell lung cancer: Long-term results of a radiation dose escalation study. Int J Radiat Oncol Biol Phys 2005;63:324–33.
- Belderbos JSA, Heemsbergen WD, De Jaeger K, Baas P, Lebesque JV. Final results of a Phase I/II dose escalation trial in non-small-cell lung cancer using three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys 2006;66:126–34.
- Bradley JD, Paulus R, Komaki R, Masters G, Blumenschein G, Schild S, et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): a randomised, two-by-two factorial phase 3 study. Lancet Oncol 2015;16:187–99.
- Cannon DM, Mehta MP, Adkison JB, Khuntia D, Traynor AM, Tome WA, et al. Dose-limiting toxicity after hypofractionated dose-escalated radiotherapy in non-small-cell lung cancer. J Clin Oncol 2013;31:4343–8.
- Darby SC, Ewertz M, Hall P. Ischemic heart disease after breast cancer radiotherapy. N Engl J Med 2013;368:2527
- Sager O, Beyzadeoglu M, Dincoglan F, Oysul K, Kahya YE, Gamsiz H, et al. Evaluation of active breathing control-moderate deep inspiration breath-hold in definitive non-small cell lung cancer radiotherapy. Neoplasma 2012;59:333–40.
- Marchand V, Zefkili S, Desrousseaux J, Simon L, Dauphinot C, Giraud P. Dosimetric comparison of free-breathing and deep inspiration breath-hold radiotherapy for lung cancer. Strahlenther Onkol 2012;188:582–9.
- Brock J, McNair HA, Panakis N, Symonds-Tayler R, Evans PM, Brada M. The use of the Active Breathing Coordinator throughout radical non-small-cell lung cancer (NSCLC) radiotherapy. Int J Radiat Oncol Biol Phys 2011;81:369–75.
- Ottosson W, Sibolt P, Larsen C, Lykkegaard Andersen JA, Borissova S, Mellemgaard A, et al. Monte Carlo calculations support organ sparing in Deep-Inspiration Breath-Hold intensity-modulated radiotherapy for locally advanced lung cancer. Radiother Oncol 2015;117:55–63.
- Tanguturi SK, Lyatskaya Y, Chen Y, Catalano PJ, Chen MH, Yeo WP, et al. Prospective assessment of deep inspiration breath-hold using 3-dimensional surface tracking for irradiation of left-sided breast cancer. Pract Radiat Oncol 2015;5:358--365.
- Josipovic M, Persson GF, Hakansson K, Damkjaer SM, Bangsgaard JP, Westman G, et al. Deep inspiration breath hold radiotherapy for locally advanced lung cancer: comparison of different treatment techniques on target coverage, lung dose and treatment delivery time. Acta Oncol 2013;52:1582–6.
- Wolthaus JW, Schneider C, Sonke JJ, van HM, Belderbos JS, Rossi MM, et al. Mid-ventilation CT scan construction from four-dimensional respiration-correlated CT scans for radiotherapy planning of lung cancer patients. Int J Radiat Oncol Biol Phys 2006;65:1560–71.
- Josipovic M, Persson GF, Logadottir A, Smulders B, Westmann G, Bangsgaard JP. Translational and rotational intra- and inter-fractional errors in patient and target position during a short course of frameless stereotactic body radiotherapy. Acta Oncol 2012;51:610–17.
- Josipovic M, Persson GF, Dueck J, Bangsgaard JP, Westman G, Specht L, et al. Geometric uncertainties in voluntary deep inspiration breath hold radiotherapy for locally advanced lung cancer. Radiother Oncol 2015. doi: 10.1016 epub.
- Persson G, Nygaard D, Munck af Rosenschöld P, Korreman S, Specht L. Variations in GTV Size in Free Breathing 4D-CT, Breathhold CT and Conventional CT Scans of Patients with Lung Tumors. Int J Radiat Oncol Biol Phys 2010;78:S735
- Rosenzweig KE, Hanley J, Mah D, Mageras G, Hunt M, Toner S, et al. The deep inspiration breath-hold technique in the treatment of inoperable non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 2000;48:81–7.
- Panakis N, McNair HA, Christian JA, Mendes R, Symonds-Tayler JR, Knowles C, et al. Defining the margins in the radical radiotherapy of non-small cell lung cancer (NSCLC) with active breathing control (ABC) and the effect on physical lung parameters. Radiother Oncol 2008;87:65–73.
- Giraud P, Morvan E, Claude L, Mornex F, Le Pechoux C, Bachaud JM, et al. Respiratory gating techniques for optimization of lung cancer radiotherapy. J Thorac Oncol 2011;6:2058–68.
- Josipovic M, Aznar MC, Persson GF. Deep inspiration breath hold radiotherapy of lung cancer: The good, the bad and the ugly case. Acta Oncol 2014;53:1446–8.
- Partridge M, Tree A, Brock J, McNair H, Fernandez E, Panakis N, et al. Improvement in tumour control probability with active breathing control and dose escalation: a modelling study. Radiother Oncol 2009;91:325–9.
