Abstract
Background. Shoulder external rotation braces used for patients with a first-time shoulder dislocation are designed with a variety of arm positions in abduction as well as external rotation. However, few studies have focused on their immobilizing performance, comfort, or user-friendliness. Especially, there have been no robust data of shoulder abduction-external rotation (A-ER) braces in comparison to those of external rotation (ER) braces.
Methods. Four types of commercially available shoulder braces (two ER and two A-ER braces) were tested in 30 healthy participants. The angles of external rotation and abduction were measured for each brace at initial application, after simulated daily activities, and after reapplication. Then, subjects were asked to assess the discomfort of bracing and difficulty of reapplication using a visual analogue scale. Data were compared between the two ER braces and two A-ER braces as well as among the four braces.
Results. For both external rotation angle and subjective assessment, there were no significant differences between the ER and A-ER braces. Among the four braces, the measurement of arm position demonstrated no significant differences, except the external rotation angles between the two ER braces. The A-ER braces were assessed to be significantly less comfortable than the ER braces in the subjective assessment.
Conclusions. Immobilization using the A-ER braces could maintain the arm position in abduction-external rotation with comparable user-friendliness, although they tended to be less comfortable during daily activities compared to the ER braces.
Introduction
It has been reported that the gleno-humeral joint dislocates most frequently among all joints in the human body. The overall incidence of traumatic anterior shoulder dislocation per year ranges from 8.2 to 23.9 per 100,000 individuals (Citation1–3). The most common sequela to the first-time shoulder dislocation is a recurrent instability. Especially in young and active individuals, the recurrence rate is unacceptably high (Citation4–7).
Traditionally, the first-time dislocation has been treated with slings or shoulder braces, which immobilize the arm in internal rotation. Recently, an alternative arm position in external rotation was proposed as a better position for immobilization. Previous studies using cadavers (Citation8,9) or magnetic resonance imaging (Citation10) demonstrated that the immobilization in external rotation could provide a better reduction of detached Bankart lesion to the anterior glenoid rim than immobilization in internal rotation. Several clinical studies were carried out, which demonstrated that the immobilization in external rotation successfully reduced the recurrence rate after the first-time dislocation (Citation11–14). Based on these basic studies and clinical evidence, a number of shoulder braces immobilizing the arm in external rotation (ER braces) have been developed.
Hart et al. (Citation15) investigated the reduction of Bankart lesion in various arm positions during arthroscopic examination in 25 patients with a first-time traumatic anterior shoulder dislocation. The best reduction of the detached Bankart lesion was constantly observed when the arm was in 30° of abduction and 60° of external rotation. Among the available ER braces, some are designed to control the arm position not only in external rotation but also in abduction. Thus, shoulder braces immobilizing in abduction-external rotation (A-ER braces) are also used for patients with a first-time dislocation.
A shoulder brace used after initial dislocation of the shoulder is required to have high performance in keeping the position to reduce the Bankart lesion, but at the same time it is required to be comfortable to wear and easy to put on and take off. To keep exactly the intended arm position, the brace should be rigid and robust. However, to be comfortable and user-friendly, it needs to be light and easy to wear. Sullivan et al. (Citation16) compared four types of ER braces for their ability to keep the arm in external rotation and their extent of comfort in application. They demonstrated a variety of performance levels among the braces. They also suggested the difference of comfort levels in application as an important factor of patients' compliance.
Regarding the available A-ER braces, however, there have been no studies focused on their comfort or user-friendliness as well as their immobilizing performance. Therefore, we investigated whether the A-ER braces could maintain the intended arm positions after some activities of daily living as well as after reapplication. We also compared comfort and ease of brace application among various braces.
Material and methods
Thirty healthy volunteers without any prior histories of shoulder problems participated in the present study. All subjects were males, and their mean age was 23.4 years (range 18–30 years). This study was approved by our Institutional Review Board. All of the subjects agreed with the testing protocol and gave their consent for participation in accordance with the Ethical Committee procedures of our institution.
Braces
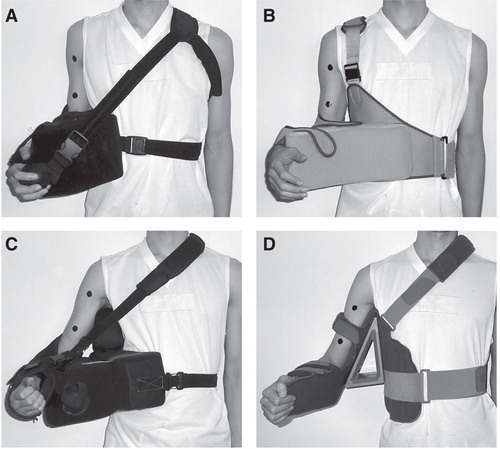
We used the following four braces: A: the UltraSling ER with a 15° wedge (DonJoy, Vista, CA, USA); B: the Shoulder Brace ER (Alcare, Tokyo, Japan); C: the Össur SmartSling with axilla pillow (Össur, Reykjavik, Iceland); and D: the Omo Immobil with shoulder positioning at 30° abduction and 30° external rotation (Otto Bock, Duderstadt, Germany) (). The former two braces were ER braces, and the latter two were A-ER braces. Each subject wore these four braces in random order in order to minimize practice effects. All braces were applied to the dominant arm of the subjects. The measurement data for each brace in each condition was presented as mean (standard deviation (SD)).
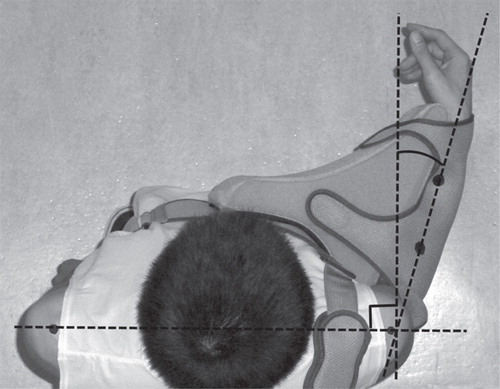
Measurement of the initial arm position with braces
Each brace was initially fitted by a physician. For the purpose of measuring the accurate abduction angle, skin markers were placed at the center of the proximal and distal upper arm (). Skin markers were also placed on the proximal and distal forearm as well as on bilateral acromio-clavicular joints similarly to the previous study by Sullivan et al. (Citation16) (). Then, for each brace, a digital photograph was taken in the frontal plane (frontal view) and the axial plane (overhead view) to measure the initial angle of abduction and external rotation. These photographs were taken from a position 3 meters away from the skin markers. The ImageJ software (version 1.42, http://rsbweb.nih.gov/ij) was used for the angle measurements in the present study.
Figure 2. Measurement of the angle of external rotation. Two skin markers were placed on the central portion of the proximal and distal forearm to define the forearm axis. To draw a line perpendicular to the frontal plane of the subject, skin markers were also placed on bilateral acromio-clavicular joints.
Changes in arm position after activities
To assess the performance of braces to maintain the arm position, the subjects wearing each brace performed several simulated daily activities (Citation16). These activities included 1) removing and reapplying a toothpaste cap, 2) removing and putting on pants, 3) opening a business letter, 4) ascending and descending a flight of stairs, 5) changing from standing to supine position and back to standing position, 6) typing on a computer keyboard, and 7) performing 15 jumping jacks. Afterward, the photographs of the overhead and frontal views were taken again to measure whether any changes in the angle of abduction and/or external rotation had occurred during these activities.
Reapplication of the braces by the subject
Each subject was instructed to remove and reapply the brace once according to the instructions provided by the manufacturer of each brace. After reapplication by the subject alone, photographs of the overhead and frontal views were taken to measure the angles of external rotation and abduction. Then, each angle obtained after each activity was compared with the initial angles.
Brace discomfort during activities and difficulty of reapplication
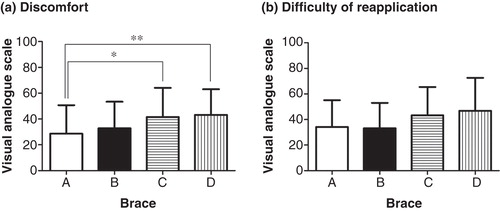
After completing the simulated daily activities and reapplying the brace, subjects were asked to assess the discomfort of braces during activities using a visual analogue scale from 0 to 100 (0 = no discomfort, and 100 = extreme discomfort). For the purpose of assessing the difficulty of reapplication by the subjects, we also used a visual analogue scale from 0 to 100 (0 = no difficulty, and 100 = extreme difficulty).
Statistical analyses
The Friedman test was used to determine the significance of differences both for the angle measurements and visual analogue scales among the brace types. The statistical analyses were performed using the GraphPad Prism software program (version 5.0, San Diego, CA, USA). The level of significance was set at P = 0.05.
Results
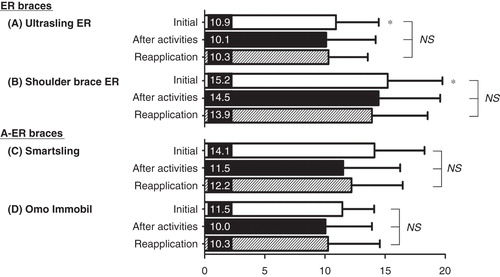
External rotation angle
The initial external rotation angles of the two ER braces, DonJoy UltraSling ER and the Alcare Shoulder Brace ER, were 10.9° (SD 3.55) and 15.2° (SD 4.54), respectively, whereas those of the A-ER braces, Össur SmartSling and the Otto Bock Omo Immobil, were 14.1° (SD 4.16) and 11.5° (SD 2.64), respectively. There was no significant difference in the initial external rotation angles between the ER braces and A-ER braces. However, within the ER braces, the Alcare Shoulder Brace ER showed a significantly greater angle of external rotation (15.2°) than the DonJoy UltraSling ER (10.9°) (P = 0.02). Regarding the ability to maintain the external rotation angle, no significant differences in all three conditions (the initial angle, the angle after activities, and the angle after reapplication) were observed either in A-ER or ER braces ().
Figure 3. The external rotation angle under three conditions (the initial angle, the angle after activities, and the angle after reapplication) for the four braces. There were no significant differences in mean values of the initial external rotation angle between the ER braces (A, B) and the A-ER braces (C, D), nor between the four braces, except for the difference between A and B, which was statistically significant (* P = 0.02). The bars are the means ± standard deviations.
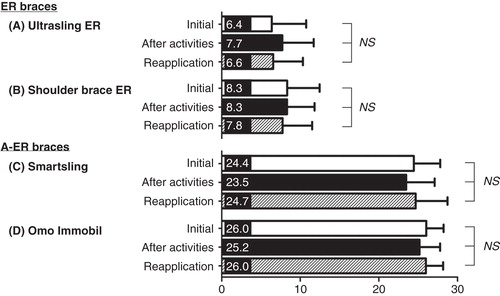
Abduction angle
The initial abduction angles of the ER braces were 6.4° (SD 4.37) for DonJoy UltraSling ER and 8.3° (SD 4.13) for Alcare Shoulder Brace ER. In contrast, the abduction angles of A-ER braces were 24.4° (SD 3.36) for Össur SmartSling and 26.0° (SD 2.21) for Otto Bock Omo Immobil. All four braces showed a sufficient ability to maintain the arm abduction position after simulated daily activities and after reapplication ().
Brace discomfort during activities and difficulty of reapplication
Regarding the comfort/discomfort of wearing the braces during simulated daily activities, the two A-ER braces were significantly less comfortable than the DonJoy UltraSling ER (). On the other hand, there were no significant differences among the four braces with regard to the ease and difficulty of reapplication ().
Figure 5. Subjective assessment of comfort and discomfort of wearing the braces during activities (a) and the ease and difficulty of reapplication (b). A = The UltraSling ER; B = The Shoulder Brace ER; C = The SmartSling; D = The Omo Immobil. The bars are the means ± standard deviations. *A to C: P = 0.02; **A to D: P = 0.01.
Discussion
In the present study, the external rotation angle of the arm maintained by the A-ER braces was comparable to that by the ER braces. Sullivan et al. (Citation16) previously focused on the external rotation angle in applying four types of ER braces and the braces' abilities to maintain the arm position after some activities or reapplication. The present study evaluated similar points using different types of braces. There were no significant differences in the external rotation angle between the ER braces and the A-ER braces. This study showed that the A-ER braces were as effective as the ER braces in maintaining external rotation of the arm. This study also showed that the A-ER braces were effective in maintaining the initial abduction position of the arm even after simulated daily activities and reapplication. From these results, we can say that the A-ER braces could provide a reliable arm immobilization in abduction and external rotation.
As for the external rotation angle, a significant difference was observed between the two ER braces: the DonJoy brace showed a significantly smaller angle of external rotation compared with the Alcare brace. This result supports the previous study by Sullivan et al. (Citation16); ER braces varied in ability to keep the arm position in external rotation. The difference in the braces' performance might indicate a possibility of inappropriate reduction of the Bankart lesion. In fact, a study using the former brace failed to show any significant effect of immobilization in external rotation (Citation17), whereas a study using the latter brace showed a significant effect (Citation18).
Using these braces in the clinical setting, not only the ability to maintain the intended arm position, but also the ease and difficulty of applying and removing the brace as well as the comfort and discomfort of wearing it need to be considered. The present study demonstrated that the A-ER braces had a tendency to be less comfortable than the ER braces during daily activities. The immobilized arm with A-ER braces is not attached to the trunk, and, accordingly, the hand is also farther from the trunk compared with the ER braces. This may cause more difficulty in carrying out activities that require both hands. On the other hand, the subjects felt no difference in the difficulty in putting on these braces. These factors are related to the patients' compliance to the braces. Therefore, when we perform conservative treatment after initial dislocation of the shoulder with use of a brace, it is important to explain to a patient not only the benefits of the brace, but also the difficulties or discomfort they may feel during brace application so that the patient would be compliant to the treatment.
There are several limitations in the present study. First, the wearing time of each brace for each participant was relatively short (30 minutes at the longest). This might have been too short to assess the true comfort or discomfort of the braces, and therefore further studies with a longer time of brace application would be required. Secondly, only healthy subjects were recruited in the present study. It would also be important to assess the performance of shoulder braces in patients with shoulder instability, because apprehension might affect the outcome of this type of study.
Conclusions
The present study revealed that the A-ER braces could maintain the arm position both in abduction and in external rotation after simulated daily activities and after reapplication of the braces. The A-ER braces and ER braces were the same in terms of difficulty in brace application, but the A-ER braces tended to be less comfortable during daily activities than the ER braces. The A-ER braces seem to be useful for the management of patients whose shoulders need to be immobilized in abduction and external rotation.
Acknowledgements
The authors thank an incorporate non-profit organization, Tohoku Seikeigeka, for funding this study.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Simonet WT, Melton LJ 3rd, Cofield RH, Ilstrup DM. Incidence of anterior shoulder dislocation in Olmsted County, Minnesota. Clin Orthop Relat Res. 1984;186–186–91.
- Krøner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg. 1989;108:288–90.
- Nordqvist A, Petersson CJ. Incidence and causes of shoulder girdle injuries in an urban population. J Shoulder Elbow Surg. 1995;4:107–12.
- Rowe CR. The results of operative treatment of recurrent dislocations of the shoulder. Surg Clin North Am. 1963;43:1667–70.
- Henry JH, Genung JA. Natural history of glenohumeral dislocation-revisited. Am J Sports Med. 1982;10:135–7.
- Arciero RA, Taylor DC. Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. J Bone Joint Surg Am. 1998;80:299–300.
- Postacchini F, Gumina S, Cinotti G. Anterior shoulder dislocation in adolescents. J Shoulder Elbow Surg. 2000;9:470–4.
- Itoi E, Hatakeyama Y, Urayama M, Pradhan RL, Kido T, Sato K. Position of immobilization after dislocation of the shoulder. A cadaveric study. J Bone Joint Surg Am. 1999;81:385–90.
- Miller BS, Sonnabend DH, Hatrick C, O'Leary S, Goldberg J, Harper W, Should acute anterior dislocations of the shoulder be immobilized in external rotation? A cadaveric study. J Shoulder Elbow Surg. 2004;13:589–92.
- Itoi E, Sashi R, Minagawa H, Shimizu T, Wakabayashi I, Sato K. Position of immobilization after dislocation of the glenohumeral joint. A study with use of magnetic resonance imaging. J Bone Joint Surg Am. 2001;83:661–7.
- Itoi E, Hatakeyama Y, Kido T, Sato T, Minagawa H, Wakabayashi I, A new method of immobilization after traumatic anterior dislocation of the shoulder: a preliminary study. J Shoulder Elbow Surg. 2003;12:413–15.
- Seybold D, Gekle C, Fehmer T, Pennekamp W, Muhr G, Kälicke T. [Immobilization in external rotation after primary shoulder dislocation]. Chirurg. 2006;77:821–6; In German.
- Scheibel M, Kuke A, Nikulka C, Maqosch P, Ziesler O, Schroeder RJ. How long should acute anterior dislocations of the shoulder be immobilized in external rotation? Am J Sports Med. 2009;37:1309–16.
- Schliemann B, Seybold D, Muhr G, Gekle C. [Immobilisation of the shoulder in external rotation after traumatic first-time dislocation-what is reasonable? A retrospective survey]. Sportverletz Sportschaden. 2009;23:100–5; In German.
- Hart WJ, Kelly CP. Arthroscopic observation of capsulolabral reduction after shoulder dislocation. J Shoulder Elbow Surg. 2005;14:134–7.
- Sullivan LG, Bailie R, Weiss N, Miller BS. An evaluation of shoulder external rotation braces. Arthroscopy. 2007;23:129–34.
- Liavaag S, Brox JI, Pripp AH, Enger M, Soldal LA. Immobilization in external rotation after primary shoulder dislocation did not reduce the risk of recurrence: a randomized controlled trial. J Bone Joint Surg Am. 2011;93:897–904.
- Itoi E, Hatakeyama Y, Sato T, Kido T, Minagawa H, Yamamoto N, Immobilization in external rotation after shoulder dislocation reduces risk of recurrence. A randomized controlled trial. J Bone Joint Surg Am. 2007;89:2124–31.