Abstract
Aims To study the 1-year outcome and to analyse predictors of outcome of a cohort of adolescent girls with anorexia nervosa (AN) or restrictive eating disorders not otherwise specified (EDNOSr) treated as out-patients in a family-based programme at a specialized eating disorder service. To calculate the incidence of anorexia nervosa among treatment-seeking girls younger than 18 in Uppsala County from 2004 to 2006.
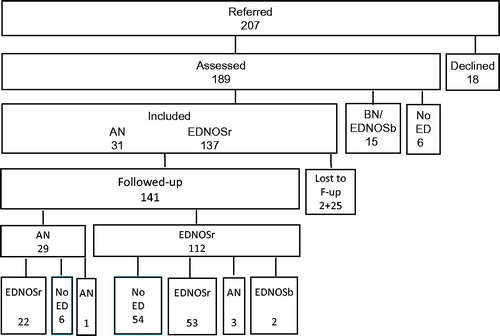
Methods A total of 168 female patients were offered treatment, and 141 were followed-up 1 year after starting treatment, 29 with AN and 112 with EDNOSr.
Results Of the 29 girls who initially had AN, 6 (20%) had a good outcome and were free of any form of eating disorder at follow-up; only 1 (3%) had AN. Of the patients with EDNOSr, 54 (48%) had a good outcome and were free of eating disorders. Three (3%) had a poor outcome and had developed AN. The incidence of AN was 18/100,000 person-years in girls younger than 12 and 63/100,000 in girls younger than 18.
Conclusion Restrictive eating disorders, including AN, in children and adolescents can be successfully treated in a family-based specialized out-patient service without in-patient care.
Introduction
Anorexia nervosa (AN) continues to have a serious prognosis despite considerable efforts to improve its treatment. Poor outcome and a chronic course of disease have been reported in 15%–20% of cases, and premature death occurs (Citation1–3). In the Global Burden of Disease Study 2013 eating disorders in women aged 15–19 in Western Europe rank as number 7 (Citation4). However, in Sweden, mortality due to AN has decreased dramatically (Citation5). The most recent lethal case of AN in a person under 20 was recorded in 1991 by the Swedish Causes of Death Register (Citation6).
There are ambiguous findings concerning the prognosis of AN with adolescent onset. Some studies report a better prognosis compared to later-onset AN, whereas others report that pre-menarcheal onset has a poorer outcome (Citation1,Citation7). Most studies are from specialist units where the referral system may cause selection bias. Also, randomized controlled trials (RCTs) that have been performed are difficult to interpret as many AN patients evade randomization and follow-up (Citation7–9).
There is increasing consensus that the start of treatment for adolescent AN should focus on weight restoration (Citation10,Citation11). Psychosocial treatment with reinforcement of parental engagement, the Maudsley model (Citation12), has shown the best long-term outcome in adolescent AN (Citation13,Citation14). The evidence supporting individual psychotherapy is weak (Citation13). Costly in-patient treatment, with disruption to everyday life, is still used for initiating weight restoration (Citation15). However, out-patient and day-patient treatment (Citation15–17) have been shown to be equally effective and may have fewer untoward effects (Citation18). Therefore, the latest recommendations emphasize treatment provided by specialized eating disorder (ED) services in out-patient settings with parents involved in treatment (Citation7,Citation19,Citation20). The ED service at Uppsala University Hospital, serving Uppsala County, was reorganized in line with these emerging recommendations in 2003. Moreover, the referral system was improved to shorten waiting lists (Citation11) and to enable assessment without delay. We have analysed the 1-year outcome of a cohort of adolescent girls diagnosed with AN or an eating disorder not otherwise specified with restrictive eating behaviours (EDNOSr) in Uppsala County, Sweden, treated between 2004 and 2006. Since there is no universally accepted measure of recovery from an ED (Citation21), we have used the following three outcome measures: 1) Not fulfilling the diagnostic criteria for AN, bulimia nervosa (BN), or eating disorder not otherwise specified (EDNOS) of the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) (Citation22); 2) Good outcome according to the Morgan–Russell Outcome Assessment Schedule (MROAS); and 3) School attendance on a full-time basis. For each of the outcome measures a prediction analysis based on the data registered at presentation of the ED was performed. Furthermore, we calculated the incidence of AN among girls up to the age of 18, based on the treatment-seeking patients in our catchment area.
Procedure
Patients
From 1 January 2004 to 31 December 2006, a total of 207 adolescent girls, 10 to 17.9 years old, from Uppsala County were referred for assessment to the Eating Disorder Unit (EDU). Of these, 18 declined assessment. Six did not fulfil criteria for an ED, and 15 were not included since they had subthreshold bulimia nervosa (). The referral documents and weight curves of those who declined assessment suggested that all had an ED but not AN. Nine of these patients eventually received treatment at other units in the Department of Child and Adolescent Psychiatry (CAP). By then, their ED was not the most prominent problem. Another 2 were re-referred with an ED outside the study period, but neither had AN. Ten boys were diagnosed with AN (n = 3) or EDNOSr (n = 7) but were not included in this study. The participants included in the study were 168 girls diagnosed with AN (n = 31) or EDNOSr (n = 137).
Initial assessment and follow-up
The initial assessment was performed by a paediatrician (I.S.). It followed a structured protocol and included the patients’ history of ED, demographic and medical background information, a somatic examination, and weight and height measurements. Patients’ weight and height history was obtained from their school health services’ growth charts. Eating disorder diagnoses and psychiatric diagnoses, according to the criteria of DSM-IV, were based on a subsequent interview by a specialist in child and adolescent psychiatry (A.R. or H.S.R.), with patients and their parent(s) (Citation23) and supported by information from self-report instruments.
One year after diagnosis, the patients were invited to a follow-up interview. A total of 132 (79%) participated in face-to-face interviews conducted by the nurse or therapist who had seen the patients during treatment. Nine were followed up by telephone interview or by reviewing their clinical records; of those 1 had AN, and 8 had an EDNOSr at initial assessment. Weight and height were measured, and the self-report instruments used at initial assessment were repeated and supplemented by the Morgan–Russell outcome assessment schedule (MROAS) (Citation24). The patients’ clinical records were scrutinized for past and present treatment and medication, and the patients were interviewed according to a structured protocol that maps ED symptoms and school attendance. For the 60 patients who no longer fulfilled the diagnostic criteria for an ED based on DSM-IV, the possible existence of lingering eating-disordered ideations of weight and shape was further explored using open-ended questions, and when there was any doubt on evaluating the degree of symptoms this was discussed within the team. However, the evaluation did not pose any difficulties for the vast majority of patients, and the ‘doubtful’ cases were very few and would not influence the overall results. During this exploratory interview, results of the self-report instruments were not available to the interviewer. The study protocol was approved by the Regional Ethical Vetting Board in Uppsala, Sweden (approval no. 2006/265).
Instruments
Two instruments were distributed to all patients at initial assessment and follow-up: 1) the Eating Disorder Inventory–Children’s version (EDI-C) (Citation25,Citation26); and 2) the Montgomery–Åsberg Depression Rating Scale–Self Report (MADRS-S) (Citation27,Citation28). At follow-up, the outcome was also evaluated using the MROAS scales: A, B, C, and E (Citation24) for the 3 months preceding the follow-up interview. Scale D—‘Psychosexual state’, concerning attitudes towards sexual relations and menstruation—was not used, as it was inappropriate to most patients’ age and development.
Analysis of growth charts
A documented maximal weight was obtained from the patients’ growth charts compiled by their school health services. Weight loss was calculated as the difference between this maximal weight and weight at assessment. Body mass index (BMI) was calculated as weight/height2 in kg/m2. Weight, height, and BMI were recalculated into Standard Deviation Scores (SDSs) (Citation29,Citation30).
Diagnostic criteria
Psychiatric diagnoses were established according to DSM-IV (Citation22). The weight criterion for AN was based on the International Statistical Classification of Diseases and Related Health Problems (ICD-10) (Diagnostic Criteria for Research) (Citation31), which, in adults, is a BMI equal to or below 17.5 kg/m2. This corresponds to a BMI SDS below –2.00 (Citation29,Citation30) in an 18-year-old girl, which was also used as the weight criterion for AN in this study. A BMI SDS of –2.00 for a 16-year-old girl corresponds to a BMI of 16.5 kg/m2, for a 14-year-old girl it corresponds to a BMI of 15.5 kg/m2, and for a 12-year-old girl to a BMI of 14.3 kg/m2. In young individuals, eating disorder symptoms may not be verbally expressed; nevertheless, meal-related and other behaviours may indicate a wish to avoid food and a preoccupation and/or dissatisfaction with shape and form. Care was, therefore, taken to assess both the symptoms verbalized by the patients and the behaviours observed and reported by their parents (Citation32), although this is not stated in DSM-IV. Depression was diagnosed according to DSM-IV (Citation22) criteria for a ‘depressive episode’.
The incidence of anorexia nervosa
The incidence of AN was calculated for all treatment-seeking girls aged 10–17.9 and stratified in four age groups.
Statistics
All statistical analyses were performed using SPSS 15.0. Values are reported as means ± SD. Student’s t tests and chi-square tests were used for comparisons of continuous and categorical variables, respectively. Predictions of outcome were calculated using logistic regression analysis for the outcome criteria: 1) absence of ED according to DSM-IV; 2) good outcome according to MROAS; and 3) attending school on a full-time basis.
Treatment
In Sweden, county councils are responsible for funding and providing health care. All services for child and adolescent psychiatry are tax-funded and free of charge. In Uppsala County, which has 300,000 inhabitants, 67,000 of which were under the age of 18 in 2004, the Department of Child and Adolescent Psychiatry (CAP) established the specialized Eating Disorder Unit (EDU) in its present form in 2003. It is the only treatment facility for adolescents with ED in the county. In order not to delay the start of treatment, patients are accepted for assessment without delay, following direct inquiries by their parents or referral by their school health services.
Care is provided by a multidisciplinary team. Treatment is in line with American Psychiatric Association (APA) recommendations (Citation33). However, in-patient care is only used as an emergency measure and not as a method for weight restoration. Treatment is manualized and strongly emphasizes parental involvement (Citation12). The only difference between out- and day-patient treatments is the time spent at the EDU. An important feature of the Swedish social security system and labour market regulations is the possibility for reimbursed parental leave to care for a severely sick child up to the age of 18 and for as long as needed.
The treatment programme comprises four steps. Day-patient treatment is offered when weight deficit is significant or eating at home involves great difficulty. The most intensive day treatment is composed of daily meals, usually from breakfast to an afternoon snack, five days a week, and supper once a week. Initially, out-patients come with one of their parents for one to five meals a week, but, as soon as families can manage meals at home, visits are reduced to once or twice a week. Adherence to the programme is monitored by weekly weighing.
The first step of the programme focuses solely on stopping on-going weight loss. At the initial assessment, parents receive advice regarding their role in the treatment and how to re-establish normal meal practices and serve meals according to a fixed schedule. School attendance is advised against, and exercise is banned until normal eating has been re-established. In family therapy, counselling is usually provided separately for parents and the patient since the level of expressed emotions may be high. Parents also participate in psycho-educative groups. The first step typically lasts 1–3 weeks.
The second step begins when eating has been almost normalized. It aims at restoring weight at a rate of 0.5–1 kg/week. If weight gain is slow and/or weight deficit large, nutritional supplements are introduced. The second step usually lasts 6–8 weeks.
The third step starts when a substantial proportion of the weight deficit has been recovered, and consists of a gradual reintroduction into school. This step usually takes several months, and parental support at meal-times may still be needed.
The fourth and final step starts only when eating, attending school, and daily routines are being reliably maintained. Cognitive Behavioural Therapy (CBT) with a ‘transdiagnostic’ approach for relapse prevention may be introduced (Citation34). When the effects of starvation are no longer present, the presence of co-morbid psychiatric disease may have to be reassessed and treated. The steps in the treatment programme are goal-oriented. Progression to the next step can only take place when the aims of the current step have been fulfilled. Treatment is offered as long as any lingering features of the ED are present.
Pharmacological treatment, primarily selective serotonin reuptake inhibitors (SSRI), is only used for co-morbid disorders such as depression or severe obsessive problems (Citation35). Olanzapine is tried if severe anxiety, constant rumination over weight and shape, or a strong urge to exercise excessively occurs (Citation36).
Hospitalization is used only as an emergency measure. When the risk for arrhythmia is imminent and/or there is complete abstinence from both food and drink, admittance to a paediatric ward for cardiac monitoring and naso-gastric tube-feeding may be required. Patients with serious suicidal ideation may require care at an adolescent psychiatric ward.
When adolescents are unwilling to participate in treatment, they are not forcibly admitted. Rather, motivational sessions are offered to support parents and enable them to motivate their children to undergo treatment (Citation37). If treatment progress is poor, active treatment may be paused for a period of 1–2 weeks and motivational sessions offered. In such cases, medical check-ups are performed weekly to ensure that emergency situations do not develop.
There are no defined criteria as to when treatment should be concluded. The patient, parents, and therapist can usually agree that the ED symptoms no longer persist and that the patient is well.
Results
Characteristics of patients at assessment
At initial assessment, the 168 adolescent girls were diagnosed with AN (n = 31) or EDNOSr (n = 137). The duration of ED symptoms, according to patients’ and parents’ recall, was 9.1 ±7.3 months (range <1–32 months) for AN, and 12 ± 10 months (range <1–41 months) for EDNOSr. The assessment was performed within 19 ± 12 days (range 2–46 days) for AN patients, and 27 ± 20 days (range 0–117 days) for EDNOSr. Six patients (4%) had previously been treated for an EDNOS, 14 (8%) had previously been treated for other psychiatric disorders, and 17 (10%) were in treatment for other psychiatric disorders. At presentation, the current medication for psychiatric disease was SSRI for depression (n = 10) and central stimulants for attention deficit/hyperactivity disorder (ADHD) (n = 2). Twenty-three patients (14%) reported current somatic disease including diabetes type 1 (n = 3), hypothyreosis (n = 3), juvenile rheumatoid arthritis (n = 2), intestinal disorders (n = 4), and asthma/allergy (n = 11). At first assessment, 128 (91%) of the 141 patients followed-up completed the EDI-C, and 138 (98%) completed the MADRS-S questionnaires. At follow-up, 115 (82%) and 118 (84%) completed the EDI-C and MADRS-S, respectively. MROAS was conducted only at follow-up; data were obtained from 124 (88%) patients ().
Table 1. Diagnoses and eating disorder features at assessment and follow-up of 141 adolescents with eating disorders.
Characteristics of 27 patients lost to follow-up
Two (6%) of the 31 patients with AN refused the treatment offered at the EDU and were also lost to follow-up. Of the patients with EDNOSr, 25 (18%) were lost to follow-up; 5 of these never started treatment. Five discontinued treatment after a few sessions. Eleven were in treatment at other units of the CAP because of neuro-developmental disorders (n = 3) or as part of a complex picture including self-harming behaviours (n = 8). Two accessed therapy outside the CAP, and 2 had left the catchment area ().
The 27 patients lost to follow-up did not differ in age, weight, BMI, weight loss, duration of ED, weight-controlling behaviours, co-morbid depression, or MADRS-S scores compared to those followed up. Amenorrhea was less common in those lost to follow-up, and they had higher (worse) scores on the EDI-C subscales: drive for thinness, body dissatisfaction, and asceticism.
Treatment given
Of the 141 patients followed up, 133 (94%) were treated at the EDU and 5 at other units of the CAP. Three with EDNOSr did not participate in any treatment ().
Table 2. Patients with anorexia nervosa (AN) or eating disorders not otherwise specified, restrictive subtype (EDNOSr), treated at the Eating Disorders Unit (EDU) or at other units in the Child and Adolescent Psychiatry (CAP) department, and number with each diagnosis at follow-up.
Thirty patients (21%), 14 with AN and 16 with EDNOSr, were enrolled in the day care programme for some part of the year, and 103 (73%) were out-patients throughout the year. No patient had been detained for compulsory treatment. There were no deaths. At follow-up, 77 (55%) were still in treatment at the EDU, but only 3 were in the day care programme.
Fifty-five patients (39%) took SSRI for some part of the year, and for 44 the medication had not yet been discontinued at follow-up. Thirty-three (23%) patients had taken olanzapine for some part of the year, but only 7 were still taking it at follow-up. Of the patients with AN, 15 (52%) had been treated with olanzapine.
Hospitalization
Three patients with AN were admitted to in-patient care: 1 with anaemia (blood haemoglobin 57 g/L), 1 received naso-gastric tube-feeding on a paediatric ward, and 1 had severe depression and was hospitalized at CAP for nearly 2 months.
Two patients with EDNOSr were admitted to a paediatric ward: 1 for cardiac monitoring following complete refusal to eat and drink, and 1 for naso-gastric tube-feeding. Hospitalization lasted 2 days and 2 weeks, respectively. Following discharge, the patients were treated in day care at the EDU. Three with EDNOSr were admitted to a CAP ward for depression, suicidal ideation, or family crisis; these admissions lasted between 2 and 4 weeks. While hospitalized, the patients continued treatment in day care at the EDU.
Of the 7 patients who were hospitalized (1 had been both on a paediatric and a CAP ward) during their first year of treatment, all had an EDNOS at follow-up. Only 2 patients out of 168 (1.2%), 1 with AN and 1 with EDNOSr, required emergency tube-feeding for 8 and 19 days respectively. None of the patients lost to follow-up had been hospitalized.
Anthropometry and menstrual status
Weight gain had been achieved at follow-up in all groups () and was of the same magnitude in patients with or without an ED diagnosis, except for the 3 with EDNOSr at initial assessment who had AN at follow-up. Menstrual status had improved during the first year of treatment, but 30 (21%) still had no menses at follow-up. Of these, 15 had not yet reached menarche. They were between 10.8 and 16.0 (median 13.8) years of age. One had a BMI SDS below –2.00 and persistent AN. Among patients with secondary amenorrhea, 3 had had EDNOSr at initial assessment but had lost weight and had AN with a BMI SDS below –2.00 at follow-up.
Table 3. Anthropometric measures and menstrual status according to diagnosis at assessment and follow-up of 168 adolescent girls with eating disorders (ED).
Diagnoses and ‘lingering symptoms’ at follow-up
Of the 141 patients followed-up, 81 had a persistent ED and 4 had AN, whereas 60 (43%) did not have an ED according to DSM-IV criteria. However, the explorative interviews with open-ended questions revealed that 20 of these 60 occasionally had some lingering symptoms and slight eating-disturbed ideations ().
Diagnoses and self-reported symptoms at follow-up
Among 81 patients with a persistent ED, the prevalence of different weight-controlling behaviours and the proportion of patients with depression were approximately similar to that at initial assessment. At follow-up, a total of 17 patients had psychiatric co-morbidity other than depression: 5 were diagnosed before assessment for their ED, and 12 were diagnosed during their first year of treatment. These patients had an obsessive-compulsive disorder (OCD) (n = 7), ADHD (n = 5), autism spectrum disorder (n = 3), bipolar disorder (n = 1), or non-mood psychosis (n = 1).
Psychometric measures
At follow-up, the MADRS-S scores were lower than at first assessment in all groups, especially among those who had recovered from their ED. Also, EDI-C scores were lower at follow-up on the subscales for drive for thinness and body dissatisfaction in patients who did not have an ED diagnosis and were completely free of symptoms (). Those not fulfilling DSM-IV criteria for an ED diagnosis but with lingering symptoms had not improved as much, while those still with an ED diagnosis had EDI-C scores comparable to those at initial assessment.
The Morgan–Russell Outcome Assessment Schedule overall outcome measures
The MROAS was performed for 124 (88%) patients at follow-up, and overall scores were high indicating a favourable outcome (). Thirteen (45%) of the patients with AN at assessment and 56 (74%) of those with EDNOSr at assessment had a good outcome. Those who still had an ED diagnosis had lower scores on the subscales for food intake and menstruation (p < 0.001). Notably, the subscales for family relationships, social activities, and school/work did not differ between groups with good or poor outcome, while the subscales for autonomy and personal contacts were lower for those with an ED diagnosis (p < 0.01). At follow-up, 122 patients (87%) were back at school on a full-time basis, although 14 (10%) had had to restart the academic year. Of those who did not have an ED diagnosis, 54 (90%) were in school.
Outcome in patients with anorexia nervosa
At follow-up, all patients with AN at assessment had gained weight. One (3%) of 29 patients still fulfilled the criteria for AN, 6 (21%) did not have an ED diagnosis, and 22 (76%) fulfilled the criteria for an EDNOSr (). Twenty-eight (97%) had recovered their weight to a level >–2.00 BMI SDS. Fifteen (52%) had regained menstruation, 7 (24%) still had secondary amenorrhea, and 7 (24%) had not reached menarche (). Twenty-seven (93%) were back at school on a full-time basis. Of the 29 patients with AN, 14 (48%) had been treated in day care during some part of the year, and 2 of these did not have an ED diagnosis at follow-up. At follow-up, of the 15 (52%) who had been treated entirely on an out-patient basis, 1 still had AN while 4 did not have an ED diagnosis (). Another 3 patients with EDNOSr at the initial assessment had been treated as out-patients but fulfilled criteria for AN at follow-up.
Prediction of outcome
The outcome predictors studied were: age at ED onset, age at menarche, BMI SDS at top weight, previous psychiatric disease, duration of the ED at presentation, menstrual status and BMI SDS at presentation, mode of weight control, presence of depression, self-destructive behaviours, and psychiatric or somatic co-morbidity. The outcome predictors differed only in that BMI SDS at presentation was lower in those with an ED at follow-up (p < 0.01). Of the self-reported measurements, the EDI-C subscales for body dissatisfaction, ineffectiveness, asceticism, and social insecurity were higher in those who had an ED at follow-up (p < 0.05). High BMI SDS at presentation predicted a favourable outcome (odds ratio (OR) of 2.12, 95% confidence interval (CI) 1.06–4.23, p < 0.05) for a 1-unit change in BMI SDS. The psychometric measurements, which were significant in the univariate analysis, did not improve prediction.
Good somatic outcome is defined by MROAS as weight being within 15% of that expected and having menses. Patients with good somatic outcome were older at the start of ED symptoms (p < 0.01), older at presentation (p < 0.01), and more often had retained menstruation (p < 0.001). However, they did not differ regarding psychometric measurements. Good somatic outcome according to MROAS could not be predicted in a logistic regression analysis.
Attending school on a full-time basis or not was analysed as an alternative outcome measurement. Psychiatric co-morbidity was a weak predictor for not attending school as evidenced by an OR of 3.09, CI 1.02–9.35 (p = 0.05). Neither anthropometric nor psychometric measurements improved prediction.
Eight patients had discontinued treatment, although further treatment had been strongly advised. Such a dropout rate could not be predicted using the above measurements. Four of these patients did not have an ED at follow-up.
Incidence of AN
The ages of the 31 patients with AN at assessment ranged from 10 to 17.9 years. There were 2, 7, 9, and 13 patients with AN in the four age groups: 10–11.9, 12–13.9, 14–15.9, and 16–17.9 years, respectively. Three patients with EDNOSr developed AN during follow-up but after the inclusion period ending 31 December 2006. They were, therefore, not included in the incidence calculation. The number of population person-years of observation was based on the mid-year population in the county of Uppsala from 2004 to 2006 obtained from Statistics Sweden (www.scb.se). The population person-years of observation were 11,311, 12,487, 12,869, and 12,158 in the four age groups. This adds up to a total of 48,825 person-years in girls aged 10–17.9 in the county. The 31 cases with AN generate an annual incidence of 63 new cases per 100,000 person-years in girls aged 10–17.9 and an annual incidence in the subgroups of 18, 56, 70, and 107 per 100,000, respectively.
Discussion
We report on a prospective 1-year follow-up of a 3-year cohort of all child and adolescent girls diagnosed with AN or EDNOSr from a defined catchment area and treated at a single specialized EDU. The assessment and manualized treatment was uniform and in line with APA recommendations (Citation37). It focused on family support to enable the parents to help their child back to normalized eating behaviours. The extensive acceptance, good adherence to treatment, and limited losses at follow-up suggest that the documented outcome was representative of the initial cohort. Treatment for adolescents was free of charge and fully financed by taxes paid in the county of residence. Treatment elsewhere in Sweden would have generated a request to the CAP for reimbursement. Private health insurance or out-of-pocket payment for specialized care of adolescents is extremely rare in Sweden. It is therefore unlikely that any treatment-seeking patients with AN would be missed. It is, however, possible that patients/families with EDNOSr and less severe symptomatology would chose support elsewhere. Indeed, such patients could probably be found among these who declined assessment.
We report two main findings. Firstly, almost all of the adolescent girls with AN or EDNOSr, irrespective of severity, could be treated as day- or out-patients without planned admissions or planned tube-feeding. Secondly, the vast majority of patients improved considerably in weight and menstrual status.
Prediction of not having an ED, at follow-up, was not strong, but it is notable that the high BMI SDS was the only predictor of such favourable outcome, which is an important predictor in numerous previous investigations (Citation1,Citation38). In this context it is important to note that the state of the patient at assessment is dependent not only on the natural course of the disease but is also influenced by the service organization. Weight loss can be reduced if the suspicion of an ED is raised early, when awareness of ED in the population is high, and when access to adequate care is rapid and uncomplicated. This has been achieved in our service through a close contact between school health services and the EDU, and by the possibility for parents to contact the EDU directly. It is thus possible that a health care organization with rapid access to care would improve outcome. It could then be expected that also short duration of disease and low age would emerge as predictors of a favourable outcome (Citation1,Citation38). This was not the case in the present study, but it is possible these potential predictors are mediators of higher BMI SDS at presentation, which then remains the single important predictor. In line with previous studies psychometric measures of ED psychopathology did not predict outcome (Citation38). It is notable that the variation of these measures at presentation was considerable and could be confounded by denial or minimization, which makes them less useful as predictors. Good outcome according to MROAS focuses on somatic outcome measures and could not be predicted by the multiple regression. This is not surprising in view of the fact that the vast majority of patients, and also those who still had an ED, had recovered weight and menstruations at follow-up. An alternative outcome measure is the ability to attend school, which presently could not be predicted by ED-related parameters. We only found a weak effect of co-morbid psychiatric disease on school attendance at 1-year follow-up. In many outcome studies, psychiatric co-morbidity is associated with less favourable ED outcome (Citation1). Our data would suggest that the ED had been handled during treatment, but the co-morbid psychiatric disease may cause difficulties when responsibilities have to be transferred from the parents to the adolescent. It is evident that parents must get adequate support to enable them to help their child. Further studies are needed to evaluate how actual and perceived parental support influences outcome (Citation39).
The challenge of the ego-syntonic values of ED symptoms and the ambivalence concerning treatment that focuses on weight gain and eating habits was addressed by offering only one treatment option and supporting the parents to help their children to adhere to it. This is not to say that treatment is only about eating and that it is concluded when full nutritional rehabilitation has been achieved. The important message to get across is that psychological issues, especially those outside the core symptoms of ED, are addressed once eating has been normalized and weight gain is well under way.
AN is often described as a disease with a protracted course, and there are reports of ca. 25% persistence of AN after 10–15 years (Citation37,Citation40). The present results give a more optimistic view and confirm the importance of early interventions as underscored by Walsh (Citation41) who explained that dieting is a habitual behaviour with specific pathways involving the amygdala, striatum, and the orbitofrontal cortex. Hopefully, by breaking the habit early, the risk for chronic development can be reduced. Treasure and Russell (Citation11) have also highlighted the importance of early interventions, emphasizing the risk of permanent damage to the developing brain caused by starvation. Preventing such damage may be the key to preventing a chronic course and the desperate outcome of chronic AN. There is no consensus regarding the definition of ‘normality’ or of being ‘free of symptoms’ when recovering from an ED (Citation21). Therefore, the significance of being completely symptom-free is unknown; one can only speculate that it implies a decreased risk of relapse (Citation40).
Comparing studies of the incidence of AN in children and adolescents entails several challenges; using different gender and age groups as well as different weight cut-offs creates difficulties. To define AN as strictly as possible, we have used a BMI SDS <–2.0 as the weight criterion together with amenorrhea. Thus, the AN incidence in our study was 63/100,000 for girls aged 10–17.9 and 107/100,000 for girls aged 16–17.9. This is lower than the 110/100,000 incidence reported by Lucas et al., based on a retrospective study of medical records from treatment-seeking 10–19-year-old female patients in 1980–1984 in Rochester, USA (Citation42). This higher incidence may be explained by the inclusion of 18–19-year-old females (Citation43). In a recent study from Canada (Citation44), the incidence among girls aged 10–12 was found to be 9.4/100,000 person-years, which is lower than our results. In a study by Nicolls et al. (Citation45), the incidence was found to be 3.6/100,000 and 4.5/100,000 in the age groups 10–11 and 11–12, respectively, which could be explained by the fact that boys were also included. There are several possible explanations for these discrepancies: 1) active screening may identify a few cases of AN which spontaneously improve without care; 2) there may be differences in the weight cut-offs used and age groups included; 3) incidence may vary considerably over time and place; and 4) when treatment is easily accessible without delay, patients may be less underweight and may not have reached the weight criterion for AN.
There are strong similarities between the patients studied here with AN and those in the two most cited RCTs of children and adolescents with AN (Citation17,Citation46). Comparing results from different studies can be difficult because of different criteria for diagnosis, treatment, and measurements of recovery (Citation2). Combining MROAS and weight recovery measurements enables comparisons between the three studies. The anthropometric data were recalculated into kilograms and meters. Individual weights, heights, and ages were not available, and BMI SDS was estimated on a group level using the mean values given in the articles (). The weight criterion for AN in the RCT by Lock et al. (Citation46) has a less strict cut-off than BMI SDS –2.0. At 1-year follow-up, there had been a weight gain corresponding to an improvement of ca. 1.0 BMI SDS over the year. In our study, there was an improvement of 1.9 BMI SDS. In the RCT by Gowers et al. (Citation17), they reported a ‘crude’ (not corrected for age) BMI at baseline of 15.3 and of 17.9 at 1-year follow-up. The corresponding values for ‘crude’ BMI in our study were 15.1 and 18.7, respectively.
Table 4. Comparison of 1-year outcome in two RCTs in specialist out-patient and family-based therapy (FBT) with a case series of a specialist out-patient FBT in Sweden.
In addition to different criteria for AN, the most striking differences between the studies are our limited use of in-patient treatment compared to the two RCTs and our high coverage of AN cases in our catchment area. The nearly exclusive day-/out-patient treatment may have augmented the self-confidence of both the patients and their parents and contributed to the outcome. In goal-oriented treatment steps, it is possible to make individual adjustments, which may have helped overcome the need for hospitalization. RCTs often yield better results than naturalistic clinical studies (Citation47). However, we are reporting on family-based treatment in a specialist out-patient setting which yielded results as good as or even better than those reported from two RCTs, especially when taking into consideration the higher proportion of poor outcome in the RCTs and the risk of long-standing AN () (Citation17,Citation46).
One weakness in this study is that the nurses/therapists who conducted the follow-up interviews knew the patients and were not blind to baseline measurements or progress through treatment. However, their knowledge of the patients and their families contributed to the retention of most of the patients for follow-up. Moreover, an interviewer with a relationship with a patient is more likely to discover lingering ED symptoms, which would otherwise pass unnoticed because of minimization or concealment. This allowed for an attempt to sharpen the stringency of the definition of recovery and assess whether patients without an ED according to DSM-IV were completely free of disturbed eating ideation (Citation40).
A second weakness refers to the calculation of AN incidence, as we have only used treatment-seeking adolescents and not an epidemiological screening approach. Nevertheless, we believe that few cases, if any, of AN have been missed thanks to co-operation with the school health services, which means that weight loss in an adolescent girl would hardly go unnoticed.
Acknowledgements
We are grateful to all participants in the study for their generosity when sharing their experiences with us. We are also grateful to the always enthusiastic staff at the Eating Disorder Unit (EDU) for taking care of the patients and helping us to distribute and collect the self-report instruments used in the study. We owe a special debt of gratitude to psychologist Åsa Törnkvist who, together with the staff at the EDU, helped us to develop the programme.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Funding information
This work was funded by Crown Princess Lovisa’s Fund for Child Health Care, the Gillbergska Foundation, the First of May Flower Annual Campaign, Professor Bror Gadelius Memorial Foundation, the Sven Jerring Foundation, and Uppsala University.
References
- Steinhausen HC. The outcome of anorexia nervosa in the 20th century. Am J Psychiatry. 2002;159:1284–93.
- Berkman ND, Lohr KN, Bulik CM. Outcomes of eating disorders: a systematic review of the literature. Int J Eat Disord. 2007;40:293–309.
- Rosling AM, Sparen P, Norring C, von Knorring AL. Mortality of eating disorders: a follow-up study of treatment in a specialist unit 1974-2000. Int J Eat Disord. 2011;44:304–10.
- Institute for Health Metrics and Evaluation (IHME), 2016. Available at: http://ihmeuw.org/3r50.
- Papadopoulos FC, Ekbom A, Brandt L, Ekselius L. Excess mortality, causes of death and prognostic factors in anorexia nervosa. Br J Psychiatry. 2009;194:10–17.
- Swedish National Board of Health and Welfare. Causes of death. 2014. Available at: http://www.socialstyrelsen.sestatisticsaldatabase/causeofdeath.
- Gowers S, Bryant-Waugh R. Management of child and adolescent eating disorders: the current evidence base and future directions. J Child Psychol Psychiatry. 2004;45:63–83.
- Treasure J, Claudino AM, Zucker N. Eating disorders. Lancet. 2010;375:583–93.
- Brownstone L, Anderson K, Beenhakker J, Lock J, Le Grange D. Recruitment and retention in an adolescent anorexia nervosa treatment trial. Int J Eat Disord. 2012;45:812–15.
- Golden NH, Meyer W. Nutritional rehabilitation of anorexia nervosa. Goals and dangers. Int J Adolesc Med Health. 2004;16:131–44.
- Treasure J, Russell G. The case for early intervention in anorexia nervosa: theoretical exploration of maintaining factors. Br J Psychiatry. 2011;199:5–7.
- Lock J, le Grange D, Agras WS, Dare C. Treatment manual for anorexia nervosa: a family-based approach. New York: Guilford Press; 2001.
- Keel PK, Haedt A. Evidence-based psychosocial treatments for eating problems and eating disorders. J Clin Child Adolesc Psychol. 2008;37:39–61.
- Couturier J, Kimber M, Szatmari P. Efficacy of family-based treatment for adolescents with eating disorders: a systematic review and meta-analysis. Int J Eat Disord. 2013;46:3–11.
- Herpertz-Dahlmann B, Schwarte R, Krei M, Egberts K, Warnke A, Wewetzer C, et al. Day-patient treatment after short inpatient care versus continued inpatient treatment in adolescents with anorexia nervosa (ANDI): a multicenter, randomised, open-label, non-inferiority trial. Lancet. 2014;383:1222–9.
- Meads C. How effective is outpatient care compared to inpatient care for the treatment of anorexia nervosa? A systematic review. Eur Eat Disord Rev. 2001;9:229–41.
- Gowers SG, Clark A, Roberts C, Griffiths A, Edwards V, Bryan C, et al. Clinical effectiveness of treatments for anorexia nervosa in adolescents: randomised controlled trial. Br J Psychiatry. 2007;191:427–35.
- Gowers SG, Weetman J, Shore A, Hossain F, Elvins R. Impact of hospitalisation on the outcome of adolescent anorexia nervosa. Br J Psychiatry. 2000;176:138–41.
- Lock J. Treatment of adolescent eating disorders: progress and challenges. Minerva Psichiatr. 2010;51:207–16.
- House J, Schmidt U, Craig M, Landau S, Simic M, Nicholls D, et al. Comparison of specialist and nonspecialist care pathways for adolescents with anorexia nervosa and related eating disorders. Int J Eat Disord. 2012;45:949–56.
- Couturier J, Lock J. What is recovery in adolescent anorexia nervosa? Int J Eat Disord. 2006;39:550–5.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, DSM-IV. Washington, DC: American Psychiatric Association; 1994.
- Rutter M. Psychopathy in childhood: is it a meaningful diagnosis? Br J Psychiatry. 2012;200:175–6.
- Morgan HG, Hayward AE. Clinical assessment of anorexia nervosa. The Morgan-Russell outcome assessment schedule. Br J Psychiatry. 1988;152:367–71.
- Garner DM. The eating disorder inventory- child (EDI-C). Lutz, FL: Psychological Assessment Resources Inc. 1991b.
- Thurfjell B, Edlund B, Arinell H, Hägglöf B, Engström I. Psychometric properties of Eating Disorder Inventory for children (EDI-C) in Swedish girls with and without a known eating disorder. Eat Weight Disord. 2003;8:296–303.
- Svanborg P, Asberg M. A new self-rating scale for depression and anxiety states based on the Comprehensive Psychopathological Rating Scale. Acta Psychiatr Scand. 1994;89:21–8.
- Cunningham JL, Wernroth L, von Knorring L, Berglund L, Ekselius L. Agreement between physicians’ and patients’ ratings on the Montgomery–Åsberg Depression Rating Scale. J Affect Disord. 2011;135:148–53.
- Lindgren G, Strandell A, Cole T, Healy M, Tanner J. Swedish population reference standards for height, weight and body mass index attained at 6 to 16 years (girls) or 19 years (boys). Acta Paediatr. 1995;84:1019–28.
- Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ. 2007;335:194–202.
- World Health Organization. International statistical classification of diseases and related health problems: ICD-10. Geneva: World Health Organization; 1994.
- Uher R, Rutter M. Classification of feeding and eating disorders: review of evidence and proposal for ICD-11. World Psychiatry. 2012;11:80–92.
- American Psychiatric Association. Treatment of patients with eating disorders, third edition. Am J Psychiatry. 2006;163:4–54.
- Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav Res Ther. 2003;41:509–28.
- Balestrieri M, Oriani MG, Simoncini A, Bellantuono G. Psychotropic drug treatment in anorexia nervosa. Search for differences in efficacy/tolerability between adolescent and mixed-age population. Eur Eat Disorders Rev. 2013;3:361–73.
- Swenne I, Rosling A. No unexpected adverse events and biochemical side effects of olanzapine as adjunct treatment in adolescent girls with eating disorders. J Child Adolesc Psychopharmacol. 2011;21:221–7.
- National Institute for Clinical Excellence (NICE). Eating disorders: core interventions in the treatment of anorexia nervosa, bulimia nervosa and related eating disorders. Clinical guidelines 9. 2004. http://www.nice.org.uk/guidelineseatingdisorders.
- Vall E, Wade T. Predictors of treatment outcome in individuals with eating disorders: a systematic review and meta-analysis. Int J Eat Disord. 2015;48:946–71.
- Nilsson K, Engström I, Hägglöf B. Family climate and recovery in adolescent onset eating disorders: a prospective study. Eur Eat Disorders Rev. 2012;20:e96–102.
- Strober M, Freeman R, Morrell W. The long-term course of severe anorexia nervosa in adolescents: survival analysis of recovery, relapse, and outcome predictors over 10-15 years in a prospective study. Int J Eat Disord. 1997;22:339–60.
- Walsh BT. The enigmatic persistence of anorexia nervosa. Am J Psychiatry. 2013;170:477–84.
- Lucas AR, Beard CM, O’Fallon WM, Kurland LT. 50-year trends in the incidence of anorexia nervosa in Rochester, Minn.: a population-based study. Am J Psychiatry. 1991;148:917–22.
- van Son G, van Hoeken D, Aad I, Barteds A, van Furth E, Hoek HW. Time trends in the incidence of eating disorders: a primary care study in the Netherlands. Int J Eat Disord. 2006;39:565–9.
- Pinhas L, Morris A, Crosby RD, Katzman DK. Incidence and age-specific presentation of restrictive eating disorders in children. Arch Pediatr Adolesc Med. 2011;165:895–9.
- Nicholls D, Lynn R, Viner RM. Childhood eating disorders: British national surveillance study. Br J Psychiatry. 2011;198:295–301.
- Lock J, Le Grange D, Agras WS. A randomized clinical trial comparing family based treatment to adolescent focused individual therapy for adolescents with anorexia nervosa. Arch Gen Psychiatry. 2010;87:1025–32.
- Accurso EC, Fitzsimmons-Craft EE, Ciao AC, Le Grange D. From efficacy to effectiveness: comparing outcomes for youth with anorexia nervosa treated in research trials versus clinical care. Behav Res Ther. 2015;65:36–41.