Abstract
A general consensus on the role of testicular biopsy in non-obstructive azoospermia (NOA) is needed. This paper reviews and updates technical aspects and clinical performance of the percutaneous testicular biopsy techniques, in particular large-needle aspiration biopsy (LNAB), and proposes a flow chart for the management of NOA.
The English literature and original data were reviewed or analyzed. Large-needle biopsy (LNB) includes large-needle cutting biopsy (LNCB) and large-needle aspiration biopsy (LNAB). LNCB usually requires scrotal incision for the insertion of relatively large needles. Fine-needle aspiration biopsy (FNAB) does not require surgical equipment or expertise, employs the smallest needles (23- to 20-gauge), and permits sperm cytologic detection. LNAB also does not require surgical equipment or expertise, employs needles of size from 20- to 18-gauge, is safe, and can be used for testicular histology and sperm recovery.
An operative flow chart is proposed for the management of NOA in which FNAB, LNAB and open surgical biopsy are used for the optimal management of NOA.
| Abbreviations | ||
| FNAB | = | fine-needle aspiration biopsy |
| IVF-ICSI | = | in-vitro fertilization with intracytoplasmic sperm injection |
| LNAB | = | large-needle aspiration biopsy |
| LNB | = | large-needle biopsy |
| LNCB | = | large-needle cutting biopsy |
| NOA | = | non-obstructive azoospermia |
| ST | = | seminiferous tubules |
| TESE | = | testicular surgical sperm extraction |
Key messages
The percutaneous testicular needle biopsy techniques include different procedures undergoing clinical and technical evaluation and progress.
Recent data suggest that they can be used for the management of non-obstructive azoospermia either for retrieval of spermatozoa or for selecting patients for surgical biopsy aimed at in-vitro fertilization.
Introduction
Testicular biopsy is commonly used in infertile men to assess the morphology and function of the testis and to distinguish between obstructive and non-obstructive azoospermia (Citation1). It is also used to retrieve sperm for in-vitro fertilization with intracytoplasmic sperm injection (IVF-ICSI) (Citation2,Citation3). We previously reviewed the different testicular biopsy techniques and classified them as percutaneous and open surgical techniques (Citation3). In the percutaneous techniques, we included the fine- and large-needle aspiration biopsy techniques. The large-needle biopsy (LNB) technique includes two types: large-needle cutting biopsy (LNCB) and large-needle aspiration biopsy (LNAB).
Although the literature contains the technical details of the aforementioned biopsy techniques, there is no consensus as to when each should be used nor on the selection of the type of procedure according to the type of azoospermia and specific clinical circumstance (Citation1,Citation4). Moreover, there is no agreement regarding the classification and the description of these techniques (Citation3). In fact, a recent report included fine-needle aspiration biopsy (FNAB) among the surgical techniques (Citation4). Indeed, testicular FNAB was used during surgical procedures (Citation5), although it is not per se a surgical procedure.
The aim of this paper is to review and update the technical aspects and clinical performance of LNAB and to compare it with the other testicular biopsy techniques—with percutaneous LNCB, in particular. Furthermore, we introduce an operative flow chart for the management of non-obstructive azoospermia (NOA) that includes percutaneous and surgical biopsy procedures.
Technical details
The percutaneous technique of LNAB was initially proposed in 1930 (Citation6) for the exploration of many superficial organs. Today, it also used for thyroid nodule examination (Citation7).
LNAB of the testicle is performed under local anesthesia; 5–7 mL of 2% lidocaine is injected into the spermatic cord with a 23-gauge needle (Citation8). A few drops of anesthetic are also injected in the scrotal puncture area. A few minutes later, the testicle is immobilized manually. A larger needle (20- or 18-gauge) is inserted into the surface of the testicle through the same skin puncture that was used for anesthesia. The needle is connected to a 20- or 30-mL disposable syringe mounted in a syringe holder. Tissue fragments are aspirated from multiple sites. The same procedure is followed for FNAB except for the smaller-sized needles (23- to 20-gauge). A 20-gauge needle can be used for either FNAB or LNAB.
The aspiration in the syringe is interrupted when tissue fragments appear in the needle extremity and in the syringe. The needle and syringe are extracted from the testicle, and the tissue fragments in the needle and/or in the syringe are recovered. In some cases, a testicular tissue fragment adheres to the scrotum at the puncture site. The puncture is performed usually twice, sometimes more, until a macroscopically satisfactory specimen is recovered, or until the patient is no longer able to tolerate the procedure. The size of the needle used for each aspiration biopsy is chosen based on the macroscopic size and aspect of the tissue fragments obtained with the previous puncture. If the aspirate appears bloody, a smaller needle can be used in the successive puncture, and some drops of heparin are included in the syringe. The testicle size dictates the initial choice of needle size—the smaller the testicle, the smaller the needle that is used (Citation9).
Cohen and Weiner described testicular LNCB using a modified Tru-Cut biopsy needle (6.3 cm) with 14-mm notch (Citation10). A spermatic cord block was performed, and local anesthesia was delivered into the scrotum. With the obturator fully retracted, the needle was inserted into the testicle through a scrotal incision. The biopsy was performed using the cutting cannula. The needle was withdrawn, and the scrotal incision was closed with suture material. The patient was advised to apply direct pressure for 15 minutes, to wear a scrotal support for 3 days, and to maintain chair or bed rest for 12 hours. Prophylactic antibiotics were also prescribed.
More recently, the Tru-Cut needle was modified into a 14-gauge automatic biopsy gun with a short (1 cm) excursion (Citation11–13) and an 18-gauge biopsy needle with a 17-mm sampling notch (Citation14,Citation15). With the latter needle, its technical performance was compared with and without that of preliminary skin incision (Citation15).
Safety
FNAB is considered a relatively safe technique, because it uses the smallest needles. However, a case of testicular bleeding after FNAB with a 21-gauge butterfly needle has been reported (Citation16).
The safety of LNAB was evaluated clinically in 387 testicles from 233 patients with non-obstructive azoospermia (Citation17). No clinical complications occurred after the needle biopsy sampling. No drugs were prescribed before or immediately after the biopsy, and no patient requested a certificate to justify his absence from work in the days after the biopsy sampling. Finally, none of the patients contacted the biopsy sampler after the biopsy, even though they had been instructed to do so if local or general problems occurred that were related to the procedures.
In another study, a total of 89 testicles from 54 patients were assessed. All of the men had undergone FNAB plus LNAB and two ultrasonographic examinations. The first image was taken immediately before the biopsy, and the second image was obtained on the days following the biopsy sampling: within 1 day (5 patients), from 1 to 10 days (5 patients), from 10 to 20 days (38 patients), from 20 to 40 days (5 patients), and on the 63rd day (1 patient). The size of 89 testicles ranged from 2.4 to 20 mL. The size of the needle used for LNAB was 18-gauge for 19 testicles, 20-gauge for 52 testicles, 21-gauge for 5 testicles, and 22-gauge for 13 testicles. There was no difference between the two images in 48 (88.9%) of the patients, whereas the second images from the remaining 6 patients performed 10 to 15 days after the biopsy showed a hypoechoic area of 1 cm around the incision site. The testicles of these six patients were examined with a needle of 18-gauge (two testicles), 20-gauge (two testicles), 21-gauge (one testicle), and 22-gauge (one testicle) (Citation17).
In a study by Cohen, the author performed 287 LNCBs (Citation10). Three patients developed small hematomas, which were treated conservatively, and five patients developed orchialgia, which did not require narcotic analgesia. Harrington performed 58 LNCBs in 58 patients. Afterwards, four of the patients (7%) had sonographic evidence of intratesticular bleeding characterized by a hypoechoic region which resolved by 6 months (Citation14). Of the 32 patients undergoing percutaneous testis biopsy, 3 (9%) required narcotic analgesia.
Tuuri et al. did not report any complication following LNCB in a small group of infertile patients (Citation18). However, the study was not aimed to assess the issue of percutaneous biopsy complications, and LNCB was performed in some patients at the time of surgical biopsy. Furthermore, in some patients LNCB required the administration of prophylactic antibiotics (Citation19) as well as time away from work (Citation11,Citation19).
Bioptic specimen size
For FNAB, the size of the bioptic specimen is not a relevant issue, because cytologic features are usually obtained with a relatively small amount of tissue. In most of the studies reporting the size of the testicular biopsy specimen obtained with LNB or open surgery, this parameter has been evaluated by the number of seminiferous tubules (ST) per histologic section. A few reports describe the weight and the dimensions of biopsy specimen.
Carpi et al. reported that in 101 LNAB testicular biopsies in 66 infertile patients—almost all of whom had NOA—the mean number of ST was 74. Six biopsies in five patients did not show sufficient material for histologic examination. The volume of the testicles varied from 11 to 29 mL (mean 22 mL), and the size of the needles ranged from 18- to 21-gauge. The mean number of ST was 24.7 when a 21-gauge needle was used, 56.2 when a 20-gauge needle was used, and 103 when an 18-gauge needle was used (Citation20).
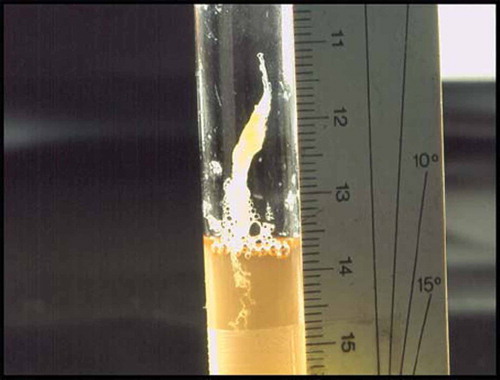
In a larger series of 215 LNABs, the data were analyzed for information on testicular size. From the testicles that were 10 mL or larger, an 18-gauge needle obtained fragments with a mean number of 92.1 ST. The smaller needle sizes—20-, 21-, and 22-gauge—obtained a mean ST of 39.5, 22.4, and 39.2, respectively. From the testicles that were between 10 and 6 mL, each of the four different-sized needles obtained specimens with a similar mean number of ST (from 34.7 to 50.9). From the testicles that were smaller than 6 mL to 3 mL, the 20-gauge and 22-gauge needles extracted 25 and 70 ST, respectively (Citation9). From 213 testicles, the mean biopsy specimen dimension and weight were 0.20 × 0.30 × 0.62 cm and 385 mg () (Citation21).
Tuuri reported ten patients with NOA who underwent percutaneous LNCB (biopsy gun). The testicular biopsy specimen showed 15 to 20 cross-sections of ST. The amount of tissue was considered sufficient to make a definitive diagnosis and to provide enough spermatozoa for IVF-ICSI (Citation18).
Morey et al. compared two groups of men undergoing testicular biopsy with a biopsy gun. In group 1, 27 testis biopsies were performed without skin incision and local anesthesia. In group 2, 40 biopsies were performed with skin incision and spinal or general anesthesia (Citation22). The mean number of ST per histologic section was 18.7 (range 6–40) in group I and 25.9 (range 2–60) in group 2 (Citation22).
Use of the biopsy specimen and principal performances
The specimens obtained with a percutaneous biopsy can be used for cytologic examination, histologic examination, and retrieval of fresh tissue for immediate IVF-ICSI, sperm research, and cryopreservation.
There is a large variation among the percutaneous techniques in terms of materials, technical aspects, and general conditions that makes a comparison difficult (Citation9). FNAB has been performed using needles with very different sizes, from 23- to 19-gauge. Multiple aspirations have been performed under general anesthesia (Citation9). FNAB cytology identifies the nuclei of Sertoli cells and adequately describes spermatogenetic cells. It does not show tubules and interstitium. FNAB is the most suitable technique for cytologic investigation.
Because the size of the tissue specimen depends on the needle size, some studies with the largest needle sizes also reported successful sperm retrieval. However, FNAB cannot be systematically recommended for sperm retrieval in patients with NOA (Citation1,Citation2,Citation23). The histologic examination usually requires a larger amount of tissue than can be obtained with FNAB.
The main purpose of FNAB is cytological examination. However, a few studies have used FNAB for testicular histologic examination and sperm retrieval in men with NOA (Citation24). When fine needles were used (21- or 23-gauge), multiple punctures, up to 15 per testicle, under general anesthesia were performed (Citation5,Citation16,Citation25). Other studies employed a 19-gauge needle with multiple punctures following intravenous sedation, followed by compression dressing and antibiotic therapy (Citation26,Citation27). Indeed, the 19-gauge needle should be considered a ‘large needle’ compared with 23- or 21-gauge needles, which are more commonly used with FNAB.
Because of the larger needle sizes used with LNCB, the procedure can obtain larger amounts of tissue than FNAB. The bioptic specimen has been largely used for histologic examination. The same specimen has also been used for sperm retrieval in a limited number of patients with NOA (Citation18). LNAB has been used for testicular histologic examination in a large series of patients with NOA. The morphologic features of LNAB histology have been compared with those of FNAB cytology in 89 testicles (Citation25). This comparison showed that elongated spermatids and spermatozoa were observed more frequently at FNAB cytology than at LNAB histology (54.2% versus 33.2%). This finding is in accordance with other limited observations reporting that spermatozoa are observed in FNAB specimens more frequently than in surgical biopsy samples (Citation28,Citation29). It also seems to confirm the observation that ‘mature sperm with tails are difficult to see on surgical biopsy’ (Citation29). During histologic preparation, when the specimens are cut into thin sections, some sperm tails may be cut. A different explanation is that the thickness of the FNAB cytology preparation is less than that of conventional histology. However, the tails are well preserved when the whole FNAB specimen is smeared on the glass (Citation17). Therefore, the addition of FNAB to LNAB or LNCB can be used to avoid an important number of cases excluded from sperm retrieval due to the absence of spermatozoa– elongated spermatids in the LNB bioptic specimen.
LNAB is now successfully used for sperm retrieval in patients with NOA for use in IVF-ICSI (unpublished data). However, the performance data have not yet been evaluated.
summarizes the principal technical characteristics and performance data of the percutaneous testicular biopsy techniques. The percutaneous testicular biopsy technique can play a central role in the management of the patients with NOA. Most of the testicular biopsy techniques are ‘entirely’ surgical such as the open surgical techniques or the traditional Tru-Cut or Biopsy-gun percutaneous biopsy technique. When clinical, hormonal, and ultrasonographic data are used, a rather reliable estimation can be made of the probability for extracting spermatozoa with a successive surgical biopsy (predicts success extraction in 71%) (Citation30). When testicular biopsy is used, this predictive power increases because intratesticular morphology including spermatogenesis is considered (positive predictive value 77% to 100%) (Citation30–33) and also extraction of spermatozoa can be achieved.
Table I. Principal technical characteristics and performances of the percutaneous testicular biopsy techniques.
However, the use of surgical biopsy in patients with NOA may represent an excessive procedure for the 50% of these patients who are expected to be devoid of intratesticular spermatozoa. The percutaneous testicular biopsy techniques, which do not require scrotal incision and any other procedure typical of surgery (FNAB and LNAB), are less expensive and well tolerated by patients. Therefore, they can be used to systematically evaluate all patients with NOA who require an estimation of the probability of a successful biopsy retrieval of spermatozoa. Furthermore they permit immediate sperm extraction probably in about 50% of the patients.
Discussion
FNAB is a relatively easy, safe and cheap biopsy technique. Furthermore, it seems more suitable for identifying intratesticular spermatozoa than the more complicated LNAB (Citation17,Citation34) and LNCB. Consequently, absence of spermatozoa by FNAB cytology should be taken into consideration in patient counseling before surgical sperm retrieval as this may imply low sperm recovery rate. In fact, sperm retrieval from the testicles of patients with NOA is unsuccessful in about 50% of cases (Citation3). This counseling may prevent the need for complicated testicular biopsy procedures in many NOA patients.
On the other hand, the needles used with FNAB may not be large enough to retrieve a tissue fragment including sperm from patients with NOA. LNCB has been used for sperm retrieval in such patients (Citation18). The data regarding sperm retrieval with LNAB have not yet been published. However, some of the authors of the current review are successfully using LNAB for this purpose. This is in agreement with the observation that the testicular biopsy size sampled with LNAB is larger than that obtained by LNB. In this vein, a recent study described how LNAB obtains relatively large biopsy specimens in a safe manner (Citation7). In that study, the internal and external cross-section area and volume of eight disposable single-cylinder needles of different sizes (25-, 23-, 22-, 21-, 20-, 18-, 16-, and 15-gauge) were determined and presumed to indicate the size of the tissue sampled (internal values) or size of tissue injured (external values) by the needle. The same reasoning was applied to a 14-gauge Tru-Cut needle. The ratio between the internal and external cross-section area or volume was regarded as a measure of safety. These ratios were greater with the 20- (0.47) or 18- (0.53) gauge needle than the 14-gauge Tru-Cut needle (0.45). This is consistent with the conclusion that LNAB is associated with less tissue injury than LNCB (Citation7).
Uncontrolled studies have compared the sperm retrieval rate obtained with percutaneous biopsy techniques and open surgical techniques, and different results have been reported (Citation4). One reason for the different results may be that the studies were not biased for etiology of NOA, biopsy techniques, and general conditions under which the percutaneous biopsy was performed (e.g. type of anesthesia) (Citation3,Citation23).
Because the presence of spermatozoa at testicular cytology or histology is the best test for predicting successful sperm retrieval with testicular surgical sperm extraction (TESE), all the percutaneous biopsy techniques can be used to this purpose (Citation3).
Each type of percutaneous biopsy technique is not standardized. For FNAB, needles of very different sizes (from 23- to 20-gauge) are generally employed (Citation5), and funicular or scrotal anesthesia has been used. For LNCB, different needles including modifications of the original Tru-Cut needle have been used. For LNAB, only one group described its use (Citation20).
In some studies, FNAB performed with relatively large needles (19-gauge) reduced the need for open surgical biopsy (Citation5,Citation26,Citation27,Citation35,Citation36). On the other hand, other studies reported that the FNAB efficacy in sperm retrieval was not very different from that of open biopsy. FNAB can be successful in sperm retrieval (Citation5), but when compared in head-to-head studies with open surgery the results suggest that open surgery was successful more often than FNAB and that after unsuccessful FNAB open surgery could still yield sperm (Citation27,Citation36).
Open surgical techniques are the most commonly described techniques in sperm retrieval from NOA patients. They are considered by many authors the gold standard, because in comparison studies with LNAB or LNB they have higher success rates (Citation23). Among the open surgical techniques, the selective microdissection reported the highest retrieval rates (Citation1,Citation3).
Conclusions
The principal difference amongst all of the biopsy techniques discussed in this review is the need for surgical equipment and expertise—neither of which is necessary with FNAB and LNAB. Concerning their different performance the following flow chart can be proposed in the management of patients with NOA (). First, perform FNAB. If FNAB retrieves spermatozoa, the goal is achieved. If FNAB does not retrieve spermatozoa while showing spermatozoa in the cytologic specimen, perform LNB, preferentially LNAB, for sperm retrieval. If FNAB cytology does not show any spermatozoa, the probability of retrieving spermatozoa with a percutaneous or an open surgical testicular biopsy is low; therefore the physician must inform and discuss with the patient. If FNAB cytology shows the presence of spermatozoa while LNAB fails in retrieving spermatozoa, an open surgical biopsy technique, particularly the microdissection sperm extraction, can still be considered. This operative flow chart, although based on limited controlled studies, considers patient compliance and safety, invasiveness, complexity, and performance data of the percutaneous and surgical testicular biopsy techniques.
Declaration of interest: The authors state no conflict of interest and have received no payment in preparation of this manuscript.
References
- Wald MA, Makhlouf A, Niederberger. Therapeutic testis biopsy for sperm retrieval. Curr Opinion Urol. 2007;17: 431–8.
- Chan PT, Schlegel PN. Diagnostic and therapeutic testis biopsy. Curr Urol Rep. 2000;1:266–72.
- Carpi A, Sabanegh E, Mechanick J. Controversies in the management of nonobstructive azoospermia. Fertil Steril. 2009;91:963–70.
- Van Peperstraten A, Proctor ML, Johnson NP, Philipson G. Techniques for surgical retrieval of sperm prior to intra-cytoplasmic sperm injection (ICSI) for azoospermia. Cochrane Database of Systematic Reviews. 2008;(2):CD002807.
- Lewin A, Reubinoff B, Porat-Katz A, Weiss D, Eisenberg V, Arbel R, . Testicular fine needle aspiration: the alternative method for sperm retrieval in nonobstructive azoospermia. Hum Reprod. 1999;14:1785–90.
- Martin HE, Ellis EB. Biopsy by needle puncture and aspiration. Ann Surg. 1930;92:169–81.
- Carpi A, Nicolini A, Marchetti C, Iervasi G, Antonelli A, Carpi F. Percutaneous large-needle aspiration biopsy histology of palpable thyroid nodules: technical and diagnostic performance. Histopathol. 2007;51:249–57.
- Li PS, Li SQ, Schlegel PN, Goldstein M. External spermatic sheath injection for vasal nerve block. Urol. 1992;39:173–6.
- Carpi A, Menchini Fabris FG, Todeschini G, Nardini V, Toldin MR, Nicolini A, . Large needle percutaneous aspiration biopsy of the testicle in men with nonobstructive azoospermia: technical performance. Biomed Pharmacother. 2006;60:557–60.
- Cohen MS, Warner RS. Needle biopsy of testes: a safe outpatient procedure. Urol. 1987;29:279–81.
- Kessaris DN, Wasserman P, Mellinger BC. Histopathological and cytopathological correlations of percutaneous testis biopsy and open testis biopsy in infertile men. J Urol. 1995; 153:1151–5.
- Sheynkin YR, Ye Z, Mendez S, Liotta D, Veeck LL, Schlegel P. Controlled comparison of percutaneous and microsurgical sperm retrieval in men with obstructive azoospermia. Hum Reprod. 1998;13:3086–9.
- Hovatta O, Moilanen J, von Smitten K, Reima I. Testicular needle biopsy, open biopsy, epididymal aspiration and intracytoplasmic sperm injection in obstructive azoospermia. Hum Reprod. 1995;10:2595–9.
- Harrington TG, Schauer D, Gilbert BR. Percutaneous testis biopsy: an alternative to open testicular biopsy in the evaluation of the subfertile man. J Urol. 1996;156:1647–51.
- Morey AF, MacDonald MF, Rozanski TA, Natarajan S, Thompson IM. Yield and efficacy of biopty gun testis needle biopsy. Urol. 1999;53:604–7.
- Friedler S, Raziel A, Strassburger D, Soffer Y, Komarovsky D, Ron-El R. Testicular sperm retrieval by percutaneous fine needle sperm aspiration compared with testicular sperm extraction by open biopsy in men with non-obstructive azoospermia. Hum Reprod. 1997;12:1488–93.
- Carpi A, Menchini Fabris FG, Palego P, Di Coscio G. Fine-needle and large-needle percutaneous aspiratiopsy of testicles in men with nonobstructive azoospermia: safety and diagnostic performance. Fertil Steril. 2005;83:1029–33.
- Tuuri T, Moilanen J, Kaukoranta S, Makinen S, Kotola S, Hovatta O. Testicular biopty gun needle biopsy in collecting spermatozoa for intracytoplasmic injection, cryopreservation and histology. Hum Reprod. 1999;14:1274–8.
- Rajfer J, Binder S. Use of biopty gun for transcutaneous testicular biopsies. J Urol. 1989;142:1021–2.
- Carpi A, Menchini Fabris FG, Gorini I, Gaeta P, Romani R, Marchetti A. A percutaneous large-needle aspiration biopsy technique for histologic examination of the testis in infertile patients. Fertil Steril. 1999;71:756–60.
- Carpi A, Menchini Fabris FG, Todeschini G, Nardini V. Large-needle percutaneous aspiration biopsy of the testicle in men with nonobstructive azoospermia. Fertil Steril. 2006;8:464–5.
- Morey AF, Plymyer M, Rozanski TA, Deshon GE, Myers JB, Dresner ML. Biopty gun testis needle biopsy: a preliminary clinical experience. Br J Urol. 1994;74:366–9.
- Chan PT, Schlegel PN. Nonobstructive azoospermia. Cur Opinion Urol. 2000;10:617–24.
- Craft I, Tsirigotis M, Courtauld E, Farrer-Brown G. Testicular needle aspiration as an alternative to biopsy for the assessment of spermatogenesis. Hum Reprod. 1997;2: 1483–7.
- Lewin A, Weiss DB, Friedler S, Ben-Shachar I, Porat-Katz A, Meirow D, . Delivery following intracytoplasmatic injection of mature sperm cells recovered by testicular fine needle aspiration in a case of hypergonadotropic azoospermia due to maturation arrest. Hum Reprod. 1996;11:769–71.
- Levine LA, Dimitriou RJ, Fakouri B. Testicular and epididymal percutaneous sperm aspiration in men with either obstructive or nonobstructive azoospermia. Urology. 2003; 62:328–32.
- Westlander G, Hamberger L, Hanson C, Lundin K, Nilsson L, Söderlund B, . Diagnostic epididymal and testicular sperm recovery and genetic aspects in azoospermic men. Hum Reprod. 1999;14:118–22.
- Meng MV, Cha I, Ljung BM, Turek PJ. Testicular fine-needle aspiration in infertile man. Correlation of cytologic pattern with biopsy histology. Am J Surg Pathol. 2001;25:71–9.
- Turek PJ, Chai I, Ljung BM. Systematic fine-needle aspiration of the testis: correlation to biopsy and results of organ ‘mapping’ for mature sperm in azoospermic men. Urology. 1997;49:734–78.
- Ezeh UIO, Taub NA, Moore HD, Cooke ID. Establishment of predictive variable associated with testicular sperm retrieval in men with nonobstructive azoospermia. Hum Reprod. 1999;14:1005–12.
- Su LM, Palermo GD, Goldstein M, Veeck LL, Rosenwaks Z, Schlegel PN. Testicular sperm extraction with intracytoplasmatic sperm injection for nonobstructive azoospermia: testicular histology can predict success of sperm retrieval. J Urol. 1999;161:112–6
- Mulhall JP, Burgess CM, Cunningham D, Carson R, Harris D, Oates RD. Presence of mature sperm in testicular parenchyma of men with nonobstructive azoospermia: prevalence and predictive factors. Urol. 1999;49:91–5.
- Amer M, Haggar SE, Moustafa T, Abd El-Naser T, Zohdy W. Testicular sperm extraction: Impact of testicular histology on outcome, number of biopsies to be performed and optimal time for repetition. Hum Reprod. 1999;14:3030–4.
- Carpi A, Menchini Fabris FG, Chiechi A, Nardini V, Romani R, Di Coscio G. Spermatogenesis in azoospermic, formerly cryptorchid men. Use of needle aspiration techniques. Acta Cytol. 2002;46:848–54.
- Silber SJ, Nagy Z, Devroey P, Tournaye H, Van Steirteghem AC. Distribution of spermatogenesis in the testicles of azoospermic men: the presence or absence of spermatids in the testes of men with germinal failure. Hum Reprod. 1997;12:2422–8.
- Khadra AA, Abdulhadi I, Ghunain S, Kilani Z. Efficiency of percutaneous testicular sperm aspiration as a mode of sperm collection for intracytoplasmic sperm injection in nonobstructive azoospermia. J Urol. 2003;169:603–5.