Abstract
Background Current guidelines recommend initial treatment with anticoagulants at home in patients with acute deep vein thrombosis (DVT) and in patients with low-risk pulmonary embolism (PE) with adequate home circumstances. However, most of the patients with acute venous thromboembolism (VTE) are currently hospitalized regardless of their risk of short-term complications.
Aim of the study To assess the proportion of outpatients with acute VTE initially treated in hospitals, to assess the mean duration of hospitalization, and to identify predictors for in-hospital or home treatment.
Methods Data of Italian patients enrolled in the RIETE registry from January 2006 to December 2013 were included.
Results Altogether 766 PE and 1,452 isolated DVT were included. Among PE patients, mean PESI score was 84 points (SD 35), and 56% of patients had a low-risk PESI score (<85). In all, 53.7% of DVT and 17.0% of PE were entirely treated at home, and 38.2% of DVT patients and 19.9% of PE patients were hospitalized for ≤5 days. On multivariate analysis, low PESI score was not independently associated with the hospitalization of PE patients.
Conclusions One in every two patients with DVT and five in every six with PE are still hospitalized.
A significant number of patients with venous thromboembolism (VTE) are still hospitalized for the acute phase of the treatment despite current guidelines recommending initial treatment with anticoagulants at home in patients with acute deep vein thrombosis (DVT) and in patients with low-risk pulmonary embolism (PE) with adequate home circumstances.
Key Messages
Introduction
Venous thromboembolism (VTE), including deep venous thrombosis (DVT) and pulmonary embolism (PE), is a serious and frequent medical condition (Citation1). Current guidelines of antithrombotic therapy recommend the use of anticoagulants in order to avoid life-threatening complications (Citation2,Citation3). A number of studies revealed that many patients presenting with DVT without PE symptoms may be safely treated entirely as outpatients (Citation4). Furthermore, in the last few years, a number of clinical rules have been developed to select a significant subgroup of patients presenting with PE at low risk of short-term complications (Citation5), and some small randomized trials have shown that these patients may be treated entirely as outpatients or may be early discharged after a short period of hospitalization (Citation6,Citation7). Thus, current guidelines recommend initial treatment at home over treatment in hospital in patients with acute DVT and suggest a home treatment or an early discharge in patients with low-risk PE, providing that home circumstances are adequate (e.g. patients expected to be compliant with follow-up, and with good social support and ready access to medical care) (Citation8,Citation9). Direct oral anticoagulants (DOACs) have been recently introduced to the market and thanks to their pharmacokinetic and pharmacodynamic characteristics may simplify the treatment of acute VTE, facilitating the management at home of these patients (Citation10). However, most of the patients with acute PE are currently treated in hospital for a standard period independently of their risk of short-term complications, and a consistent number of patients are still hospitalized for the acute DVT treatment.
This may be due to patients’ or doctors’ preference, and to local or country differences in organization and access to outpatient medical facilities. Thus, the aim of our study is to provide information on the management of acute VTE treatment in Italy in terms of rate and duration of hospitalization using data collected by Italian centers of the RIETE study. Furthermore, using data from this database, we evaluated potential predictors of complete home treatment and of early discharge.
Methods
Study design
The RIETE registry is an ongoing, multicenter, observational registry initiated in March 2001 with the aim to record current clinical management of VTE, initially in Spanish hospitals and subsequently also in hospitals from other European and American countries. In Italy, patient enrolment started in September 2003 and is currently ongoing. At each participating site, investigators enrolled consecutive patients with acute symptomatic VTE confirmed by positive compression ultrasonography for DVT. Treatment decisions were entirely left at the discretion of attending clinicians, and no therapeutic algorithms were provided. Patients enrolled in blinded randomized controlled trials on VTE treatment were excluded. Investigators recorded data on a computer-based case report form and submitted the forms to a centralized coordinating center through a secure website. The RIETE coordinating center used multiple data quality control procedures to optimize data quality. In particular, data were regularly monitored to detect inconsistencies or errors, and queries requiring resolution by the local investigators were sent to each site. Furthermore, contract research organizations monitored data quality by comparing medical records with the submitted data during periodic visits to participating hospitals. This Registry is supported by unrestricted educational grants from Sanofi Spain and Bayer Pharma AG.
The RIETE registry is conducted in accordance with human subject protection.
Study variables
The following baseline data were collected at the time of inclusion in the study: age; gender; body weight; VTE presentation (i.e. DVT as the first presentation); presence of comorbid conditions including chronic heart or lung disease; recent (<30 days prior to VTE) major bleeding; concomitant medications use, including antiplatelet drugs, statins, or steroids; presence of major risk factors for VTE including active cancer (defined as newly diagnosed cancer, metastatic cancer, or cancer undergoing treatment), immobility (defined as non-surgical patients assigned to bed rest with bathroom privileges for ≥4 days 2 months prior to VTE), surgery (≤2 months prior to VTE), leg trauma or fracture, use of hormonal therapy, pregnancy or puerperium; and laboratory tests results including full blood count and serum creatinine levels. Patients presenting with PE either with or without a concomitant DVT were considered as PE patients for the study purposes. For each patient, information on management (hospitalization or treatment on an outpatient basis) and on length of hospital stay was gathered. Therapeutic strategies were distinctly documented for both acute treatment and for the long-term treatment.
Investigators assessed the occurrence of symptomatic recurrent DVT (defined as a new non-compressible vein segment, or an increase of the vein diameter by at least 4 mm compared with the last available measurement on venous ultrasonography), of recurrent symptomatic PE (defined as a new ventilation-perfusion mismatch on lung scan or a new intraluminal filling defect on spiral computed tomography), and of major bleeding (defined as fatal, retroperitoneal, spinal, or intracranial, or requiring a transfusion of at least two units of blood) during the follow-up period. Mortality in the first 3 months after the index event was collected and assessed using medical record review, and proxy interviews when necessary. For the study purposes, only data from Italian centers regarding the acute management of VTE were considered.
Statistical analysis
Baseline characteristics are reported by means of descriptive statistics: continuous variables are expressed as mean plus or minus the standard deviation (SD) or as median with interquartile range when data did not have a normal distribution (according to the Wilk–Shapiro test); categorical data are given as counts and percentages. In particular, for the study purposes, we provide information on the rate of hospitalization and on the mean length of in-hospital stay (LOS) in patients presenting with acute PE (with or without a concomitant DVT) and in patients presenting with acute DVT without a concomitant diagnosis of PE. Rate of complete home treatment and of early discharge in DVT and in PE patients in different study periods were compared. Variables potentially associated with a treatment on an outpatient basis and with an early discharge (LOS ≤5 days) were evaluated at the univariate analysis using the Mann–Whitney test (for continuous variables) and the chi-square or Fisher’s exact test (for dichotomous variables). Variables statistically or marginally significant (P < 0.10) at the univariate analysis were introduced in a multivariate model (backward binary logistic regression model) repeated for DVT and PE patients and using complete home treatment and early discharge as the dependent variable. Patients who died within 72 hours from VTE diagnosis were excluded from this analysis. The SPSS software (version 15, SPSS Inc., Chicago, IL, USA) was used for statistical management of the data. A two-sided P value of 0.01 was considered to be statistically significant.
Results
Between January 2006 and December 2013, a total of 3,970 consecutive patients over 18 years with acute, symptomatic, objectively confirmed VTE had been enrolled by the Italian centers of the RIETE study. Exclusion of 1,752 patients who developed VTE during hospitalization left 2,218 patients for evaluation; 766 patients (34.5%) had PE (with or without a concomitant DVT), and 1,452 patients (65.5%) had an isolated DVT. As expected, DVT and PE patients had a number of differences in terms of clinical characteristics, initial presentation, risk factors, and underlying clinical conditions (). Furthermore, patients with DVT were more likely treated at home than those with PE, and significantly more DVT patients were hospitalized for 5 days or less compared to PE patients (53.7% versus 17.0%; and 38.2% versus 19.9% respectively; P < 0.01 for both).
Table I. Clinical characteristics of the patients, according to initial VTE presentation.
Patients with PE were more likely treated with unfractionated heparin and less likely with low molecular weight heparin (LMWH) as initial therapy in comparison to DVT patients (). Furthermore, significantly fewer patients with PE were treated with long-term LMWH and fondaparinux in comparison to DVT patients. At the time of data collection only a few patients were treated initially and in the long-term phase with direct oral anticoagulants.
Table II. Treatment strategies and 90-day outcome, according to initial VTE presentation.
In PE patients the mean PESI score was 84 (SD 35), and 56% of patients had a low-risk PESI score (≤85).
On univariate analysis, several parameters and characteristics were significantly associated with home treatment and with early discharge in patients presenting with PE and with isolated DVT ( and ). Among these, age, pulse >110 bpm, anemia, and creatinine clearance (CrCl) levels <60 mL/min were associated with initial in-hospital treatment, whereas estrogen therapy as risk factor was associated with complete home treatment both for DVT and PE patients. Significantly more patients had a low-risk PESI, and the mean PESI score was significantly lower in PE patients treated at home.
Table III. Univariate analysis comparing home treatment versus in-hospital treatment. Patients dying ≤24 h after the index event were excluded from this analysis.
Table IV. Univariate analysis comparing early discharge (≤5 days) or home treatment versus in-hospital treatment. Patients dying ≤24 hours after the index event were excluded from this analysis.
On multivariate analysis, in patients presenting with PE, pulse >110 bpm was significantly associated with initial in-hospital treatment and with a hospitalization >5 days, whereas presence of cancer was associated with short duration of hospitalization (<5 days), and pregnancy or puerperium were significantly associated with complete home treatment (). However, only 15 of 726 patients (2.1% of the whole population presenting with PE) had pregnancy or puerperium, thus these latter results should be considered with caution. In patients presenting with isolated DVT, age >65 years, anemia, and CrCl levels <60 mL/min were associated with initial in-hospital treatment and with a longer period of hospitalization (>5 days); pulse >110 bpm was associated with initial in-hospital treatment; and heart failure, anemia, and CrCl levels <60 mL/min were all associated with a longer duration of hospitalization ().
Table V. Multivariate analysis (backward binary logistic regression model) using variables statistically or marginally significant (P < 0.10) at the univariate analysis repeated for DVT and PE patients and using complete home treatment and early discharge as dependent variable (four multivariate models in total).
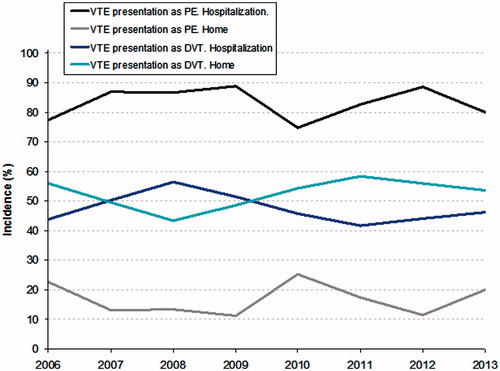
The rate of hospitalization for PE and for isolated DVT did not significantly change during the period of the study (P = NS) (). Although mean duration of hospital stay appeared highly variable in patients presenting with PE, it was significantly reduced during the study period in patients at high risk according to the PESI score (P = 0.02), and there was a non-significant trend towards a reduction in patients at low risk according to the PESI score (P = 0.07) ().
Figure 2. Mean duration of hospital stay of PE patients according to the PESI score during the study period.
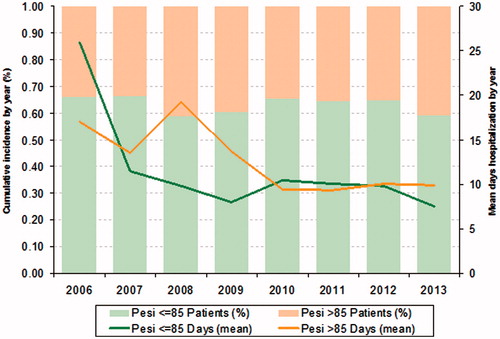
Finally, duration of hospitalization for DVT decreased significantly during the study period (from 12.3 to 7.02 days; P = 0.02)
Discussion
Recent guidelines on the management of VTE suggest that the vast majority of patients with acute DVT may be safely treated at home and that a not negligible proportion of patients with acute PE may be treated entirely as outpatients or may be discharged early after a short period of hospitalization (Citation8,Citation9). However, there are major country differences in the treatment of patients with acute VTE. Thus, information from specific countries may be useful to improve the management of these patients. Using data collected in the RIETE registry, we were able to provide information on the rate and length of hospitalization for acute PE or DVT in a large cohort of consecutive Italian patients. In our population, about 80% of patients presenting with PE and about 50% of patients presenting with isolated DVT were initially treated on an in-hospital basis. Mean length of hospitalization was 11 days for PE patients and 9 days for DVT patients respectively. Interestingly, mean hospitalization progressively reduced over time, whereas the rate of hospitalization for the acute VTE did not vary over time. Information on the acute management of VTE came mainly from studies that used the national hospital discharge databases (Citation11,Citation12), and only limited inferences can be drawn from them since they included only hospitalized patients. Furthermore, in these databases only limited data on comorbidities were presented. Conversely, only a few registries providing data on this topic are available. In the MASTER registry, a collaborative study published a few years ago that collected information from 25 Italian centers for a total of 2,119 patients (519 with pulmonary embolism), 68.1% of patients were initially treated in hospital for their VTE (Citation13). This percentage appeared significantly higher in comparison to our population, especially considering that less than one-quarter of the patients included in this registry were treated for a PE. Although several prospective studies and a small randomized controlled trial demonstrated that PE patients with a low PESI score (PESI score I–II) may be safely treated at home or discharged after a few days of hospitalization (Citation5,Citation6), this did not appear to influence the rate and the length of hospitalization in our population. A lack of knowledge about the different risk of short-term complications in patients with different PESI scores may be a possible explanation for these results. Alternatively, we should consider other factors including a lack of an adequate outpatient medical facility or of support from family or friends, or the doctor’s or patient’s preferences. Older age, pulse >110 bpm, anemia, and the presence of heart or renal failure were significantly associated with rate and length of hospitalization at multivariate analysis. Many of these variables were included in the PESI score, and all these have been consistently associated with an increased risk of short-term adverse outcome in a number of different studies (Citation14). Conversely, in patients treated for an acute PE, the presence of cancer was associated with short duration of hospitalization (<5 days), and pregnancy or puerperium were significantly associated with complete home treatment. Usually, an adequate outpatient medical facility is already present in cancer patients, and they are frequently seen as outpatients by oncologists for the treatment of their disease, thus facilitating an early discharge. On the other hand, results on treatment of patients with pregnancy or puerperium should be considered with caution since only a few patients with these conditions have been included in our study.
Reduction of the rate of hospitalization and in the length of hospital stay in patients with acute VTE may be of clinical relevance. The economic burden of in-hospital treatment of DVT and PE is not negligible (Citation15,Citation16), and different policies may be useful to reduce these costs. Implementation of recent guidelines on the management of acute VTE may reduce the rate of hospitalization and the length of hospitalization for acute VTE. Furthermore, the use of DOAC may simplify the acute treatment of VTE, and recent studies suggest that treatment with these compounds is associated with a lower rate of hospitalization and with a shorter duration of hospitalization both in patients presenting with DVT and with PE (Citation17). However, to date, the effectiveness of these strategies has not been confirmed in any clinical ‘real-world’ study, and future studies are warranted to confirm our hypothesis.
Our study has some limitations. First, RIETE is an ongoing observational registry, and thus our results should be interpreted with extreme caution. Second, although we collected data from 30 different centers from different Italian regions, treatment in centers participating in the RIETE registry may not be representative of the general treatment in Italian centers, and thus our results may not be fully generalizable. Last, some of the results are based on a limited number of patients with a specific clinical condition and should be interpreted with extreme caution.
In conclusion, a significant number of patients with PE and with DVT are still hospitalized for the acute phase of the treatment. PESI score did not appear significantly to affect the rate and the length of hospitalization in patients presenting with acute PE. Studies evaluating strategies facilitating the home treatment of acute VTE in Italy are warranted.
Acknowledgements
We thank the RIETE Registry Coordinating Center, S & H Medical Science Service, for their quality control data, logistic, and administrative support and Professor Salvador Ortiz, Universidad Autónoma de Madrid and Statistical Advisor S& H Medical Science Service, for the statistical analysis of the data presented in this paper.
Funding
Bayer Pharma AG supported this Registry with an unrestricted educational grant. RIETE is exclusively supported by Bayer Pharma AG for those centers including patients in the database with regard to the territory (outside of Spain).
Declaration of interest
The authors have no economic or intellectual conflict of interest to declare.
References
- Cohen AT, Agnelli G, Anderson FA, Arcelus JI, Bergqvist D, Brecht JG, et al. VTE Impact Assessment Group in Europe (VITAE). Venous thromboembolism (VTE) in Europe. The number of VTE events and associated morbidity and mortality. Thromb Haemost. 2007;98:756–64.
- Agnelli G, Becattini C. Acute pulmonary embolism. N Engl J Med. 2010;363:266–74.
- Lensing AW, Prandoni P, Prins MH, Büller HR. Deep-vein thrombosis. Lancet. 1999;353:479–85.
- Wells PS, Kovacs MJ, Bormanis J, Forgie MA, Goudie D, Morrow B, et al. Expanding eligibility for outpatient treatment of deep venous thrombosis and pulmonary embolism with low-molecular-weight heparin: a comparison of patient self-injection with homecare injection. Arch Intern Med. 1998;158:1809–12.
- Squizzato A, Donadini MP, Galli L, Dentali F, Aujesky D, Ageno W. Prognostic clinical prediction rules to identify a low-risk pulmonary embolism: a systematic review and meta-analysis. J Thromb Haemost. 2012;10:1276–90.
- Aujesky D, Roy PM, Verschuren F, Righini M, Osterwalder J, Egloff M, et al. Outpatient versus inpatient treatment for patients with acute pulmonary embolism: an international, open-label, randomised, non-inferiority trial. Lancet. 2011;378:41–8.
- Otero R, Uresandi F, Jiménez D, Cabezudo MA, Oribe M, Nauffal D, et al. Home treatment in pulmonary embolism. Thromb Res. 2010;126:e1–5.
- Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, et al. American College of Chest Physicians. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e419S–94S
- Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al. Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35:3033–69.
- Schulman S. Advantages and limitations of the new anticoagulants. J Intern Med. 2014;275:1–11.
- de Miguel-Díez J, Jiménez-García R, Jiménez D, Monreal M, Guijarro R, Otero R, et al. Trends in hospital admissions for pulmonary embolism in Spain from 2002 to 2011. Eur Respir J. 2014;44:942–50.
- Pomero F, Fenoglio L, Melchio R, Serraino C, Ageno W, Dentali F. Incidence and diagnosis of pulmonary embolism in Northern Italy: a population-based study. Eur J Intern Med. 2013;24:e77–8.
- Agnelli G, Verso M, Ageno W, Imberti D, Moia M, Palareti G, et al. MASTER Investigators. The MASTER registry on venous thromboembolism: description of the study cohort. Thromb Res. 2008;121:605–10.
- Agrawal N, Ramegowda RT, Patra S, Hegde M, Agarwal A, Kolhari V, et al. Predictors of inhospital prognosis in acute pulmonary embolism: keeping it simple and effective! Blood Coagul Fibrinolysis. 2014;25:492–500.
- Gussoni G, Foglia E, Frasson S, Casartelli L, Campanini M, Bonfanti M, et al. FADOI Permanent Study Group on Clinical Governance. Real-world economic burden of venous thromboembolism and antithrombotic prophylaxis in medical inpatients. Thromb Res. 2013;131:17–23.
- Merli G, Ferrufino C, Lin J, Hussein M, Battleman D. Hospital-based costs associated with venous thromboembolism treatment regimens. J Thromb Haemost. 2008;6:1077–86.
- van Bellen B, Bamber L, Correa de Carvalho F, Prins M, Wang M, Lensing AW. Reduction in the length of stay with rivaroxaban as a single-drug regimen for the treatment of deep vein thrombosis and pulmonary embolism. Curr Med Res Opin. 2014;30:829–37.
Appendix 1
The RIETE Registry
Coordinator of the RIETE Registry: Dr Manuel Monreal (Spain)
RIETE Steering Committee Members: Dr Hervè Decousus (France); Dr Paolo Prandoni (Italy); Dr Benjamin Brenner (Israel)
RIETE National Coordinators: Dr Raquel Barba (Spain); Dr Pierpaolo Di Micco (Italy); Dr Laurent Bertoletti (France); Dr Sebastian Schellong (Germany); Dr Inna Tzoran (Israel); Dr Abilio Reis (Portugal); Dr Marijan Bosevski (Republic of Macedonia); Dr Henri Bounameaux (Switzerland); Dr Radovan Malý (Czech Republic); Dr Philip Wells (Canada); Dr Manolis Papadakis (Greece)
RIETE Registry Coordinating Center: S & H Medical Science Service
Members of the RIETE Group (Italy): Amitrano M, Apollonio A, Barillari G, Bilora F, Brandolin B, Bucherini E, Camerota A, Ciammaichella M, Dentali F, Di Micco P, Enea I, Ferrazzi P, Guida A, Giorgi-Pierfranceschi M, Gussoni G, Lessiani G, Lodigiani C, Maida R, Mastroiacovo D, Pace F, Pesavento R, Pinelli M, Prandoni P, Rota L, Tufano A, Turello M, Venturelli U, Visonà A, Zalunardo B