Abstract
Aim: Recently, monocyte-to-high density lipoprotein ratio (MHR) has been proposed as a novel prognostic indicator of cardiovascular diseases. However, no study is currently available regarding the comparison between MHR and monocyte count (MC) in predicting the outcomes among patients undergoing coronary angiography.
Methods: A total of 3798 patients scheduled for selective coronary angiography were enrolled and followed up to capture major adverse cardiovascular events (MACEs, death, acute myocardial infarction, unstable angina, stroke, heart failure, and unexpected coronary revascularization). Cox proportional hazards models were used to evaluate the risk of MHR or MC on MACEs.
Results: During a median of 24.6 months follow-up, 347 (9.1%) MACEs occurred. The upper tertiles of MC and MHR have a significant lower event-free survival (p = 0.011; p = 0.014, respectively). Significantly, both MC and MHR were associated with increased MACEs risk after adjusting for potential confounders [adjusted HR (95% CI): 2.734 (1.547–4.832); 2.031 (1.268–3.254), respectively]. Additionally, the area under the receiver-operating characteristic curves of MC or MHR in predicting MACEs were 0.574 (0.542–0.606) and 0.562 (0.530–0.594) (p < 0.001, both), respectively.
Conclusions: Our data firstly indicated that MHR was an independent predictor of MACEs whereas the prognostic impact was not superior to MC in patients who underwent coronary angiography.
MHR has been suggested as a novel prognostic indicator of several cardiovascular diseases.
No study is currently available regarding the comparison of MHR to MC in predicting the outcomes in a large cohort of patients undergoing coronary angiography.
Our data firstly indicate that MHR is independently associated with MACEs in patients undergoing coronary angiography whereas the prognostic impact is similar to MC.
Key Messages
Introduction
Although atherosclerosis, the main cause of coronary artery disease (CAD), has been considered to be a multi-factorial disease, the nature of inflammatory response has been widely recognized in recent years (Citation1). Professionally, the inflammatory response has been described as the recruitment, maintenance and amplification of white blood cells (WBC) in the atherosclerotic lesions (Citation2,Citation3).
WBC count and its subsets are easily and widely available and have been reported to be consistently associated with the risk of atherosclerotic cardiovascular diseases (Citation4,Citation5). It has been proved that monocytes and differentiated macrophages can modulate inflammatory cytokines and tissue remodeling in the process of CAD (Citation6).
In addition, the effects of high-density lipoprotein (HDL) particles on monocytes have been proposed, such as mediating cholesterol efflux from macrophages, inhibiting the endothelial cells against inflammation and oxidation (Citation7,Citation8). Recently, monocyte-to-HDL-cholesterol (HDL-C) ratio (MHR) has been emerged as a novel cardiovascular prognostic marker. It has been reported to be related to cardiovascular outcomes in patients with chronic kidney disease (Citation9), the recurrence of atrial fibrillation (Citation10), and presence and severity of isolated coronary artery ectasia (CAE) (Citation11). Moreover, the recent evidence suggested that in patients with acute ST-segment elevation myocardial infarction (STEMI), the admission MHR values were independently correlated with in-hospital major adverse cardiovascular events (MACEs) (Citation12) and seemed to be an independent predictor of stent thrombosis in STEMI patients (Citation13).
However, to the best of our knowledge, no studies investigated the relationship between MHR and future MACEs in patients with suspected CAD who underwent selective coronary angiography up to date. Furthermore, no current data has compared the predictive value of MHR to monocyte count (MC) directly in the same cohort of population.
Thus, in the current follow-up investigation regarding a large cohort of Chinese Han patients who underwent coronary angiography, we sought to comprehensively investigate the prognostic value of MHR on future MACEs and further compared with the value of MC directly.
Methods
Study design and population
The study complied with the Declaration of Helsinki and was approved by the hospital’s ethical review board (FuWai Hospital & National Center for Cardiovascular Diseases, Beijing, China). Each participant provided written, informed consent before enrollment.
The design of the current study has been previously described (Citation14). In brief, a total of 3823 Chinese Han subjects who scheduled for selective coronary angiography for being suspected or known coronary atherosclerosis were enrolled between March 2011 and April 2014. The reasons for hospitalization were typical angina-like chest pain or tightness brought on by exertion and relieved by rest or sublingual nitrates or both, a positive treadmill exercise test (>1 mm ST-segment depression) or coronary stenosis indicated by coronary computed tomography (CT) angiography. Of these patients, 25 were excluded due to no WBC count and its subsets measurement available. Therefore, there were 3798 eligible cases finally studied. Exclusion criteria included acute coronary syndrome (ACS), active cardiopulmonary diseases and serious systematic disease such as serious acute left heart failure, severe trauma, significant hematologic disorders, infectious or systematic inflammatory disease within one month, severe liver (aspartate aminotransperase or alanine aminotransferase three times more than the upper normal limits) and/or renal insufficiency (blood creatinine >132 μmol/L) and malignant disease on the baseline.
In this study, the detailed demographic, clinical, hematologic, and angiographic data were collected from all subjects at baseline. Hypertension was defined as repeated blood pressure measurements ≥140/90 mmHg (at least two times in different environments) or currently taking anti-hypertensive drugs. Diabetes mellitus (DM) was defined as a fasting serum glucose level ≥7.0 mmol/L in multiple determinations and/or the current use of medication for diabetes. Dyslipidemia was defined by medical history or the use of lipid-modulating medications in order to reduce lipids or fasting total cholesterol (TC) ≥ 5.1 mmol/L or triglyceride (TG) ≥ 1.70 mmol/L.
Biochemical analyses
Fasting blood samples were collected in pre-cooled EDTA tubes at baseline before the procedure of coronary angiography. The HDL-C concentration was determined by selective solubilization method (Determiner L HDL, Kyowa Medex, Tokyo, Japan). The other lipid parameters were measured by enzymatic methods. The levels of lipid profiles were determined by automatic biochemistry analyzer (Hitachi 7150, Tokyo, Japan). WBC counts were determined by the automated hematology analyzer XE-1200 (Sysmex, Kobe, Japan).
Assessment of traditional risk factors and severity of coronary atherosclerosis
The traditional risk factors included risk age of onset, male, obesity, hypertension, DM, dyslipidemia, smoking, and family history of CAD. The angiography proven CAD was diagnosed as obstructive lesion >50% in at least one of the three major coronary arteries or major branches assessed by at least two independent senior interventional cardiologists based on quantity coronary angiography. The severity of coronary atherosclerosis was evaluated by Gensini score, which was computed by assigning a severity score to each coronary lesion according to the degree of luminal narrowing and the importance of location (Citation15).
Outcome measure
Follow-up data were obtained via standardized telephone interviews conducted by study nurses who were blinded to the aim of this study, after 6, 12, 24, 36, 48, and 60 months. If patients reported that they had been hospitalized, appropriate hospital records were consulted. The MACEs (Citation16) were the composite of all cause death (including cardiac death), non-fatal acute myocardial infarction (MI), unstable angina need for hospitalization, stroke, heart failure, and unexpected coronary revascularization [including percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG)] due to clinical deterioration. All available relevant data from any reported possible event were collected. Death of a participant was reported by relatives or the general practitioners who treated the participant. Cardiac death defined as a primary cause of acute MI, sudden cardiac death, congestive heart failure, and other structural or primary cardiac cause of death. Stroke was defined on the basis of the presence of acute infarction as demonstrated by imaging or based on the persistence of symptoms. Non-fatal MI was confirmed of the following: chest pain or equivalent symptom complex, positive cardiac biomarkers, and electrocardiogram changes typical of MI. Unstable angina was defined as chest pain or chest pain equivalent with dynamic electrocardiogram changes such as ST depression or T wave inversion but without abnormal cardiac biomarkers and characterized by rest symptoms, new-onset angina (<2 months duration), or increasing duration or severity of previously stable angina symptoms. Three experienced physicians who were masked to any of the study data independently classified the events.
Statistical analysis
The values are expressed as the mean ± SD, median with interquartile range (IQR) for the continuous variables and as the number (percentage) for the categorical variables. Continuous variables and categorical variables were analyzed by Student’s t tests, Mann–Whitney U tests or chi-squared statistic tests when appropriate.
The event-free survival rates among tertiles of MC or MHR were estimated by the Kaplan–Meier method and compared by the log rank test. The effect of MC or MHR on the occurrence of MACEs was evaluated using Cox proportional hazards models. Hazard ratio (HR) and 95% confidence interval (CI) were calculated. Patients were censored if they were lost to follow-up. The predictive value of MHR and MC on the occurrence of MACEs was analyzed by receiver-operating characteristic curves (ROC), and the area under the ROC (AUC) was assessed thereby.
The statistical analysis was performed with SPSS version 19.0 software (SPSS Inc., Chicago, IL). For all analyses, p < 0.05 was considered significant.
Results
Baseline characteristics
The current analysis included 3798 eligible patients. Follow-up data were not obtained in 168 patients (4.4%) for several reasons. Therefore, prospective analysis was confined to 3630 patients. Baseline characteristics according to the occurrence of MACEs are shown in . There was a trend towards to be older, higher percentage of hypertension, and DM in patients with MACEs. Additionally, among different treatment strategies, patients who underwent CABG had significant high rate of MACEs (CABG vs. PCI vs. medicine management: 17.0% vs. 11.2% vs. 7.1%). Meanwhile, the use of cardiovascular medications such as angiotensin converting enzyme inhibitors (ACEI), angiotensin receptor blocker (ARB), β-blockers and statins was similar between groups. Significantly, compared with patients without MACEs, several inflammatory markers were markedly higher (such as the WBC count and its subsets, high sensitivity C reactive protein (hs-CRP), p < 0.01, all). As expected, the MC was higher in patients with MACEs (p < 0.001, ). Although the HDL-C levels were similar between two groups (p > 0.05, all), the MHR remained significantly higher in patients who suffered MACEs (p < 0.001, ).
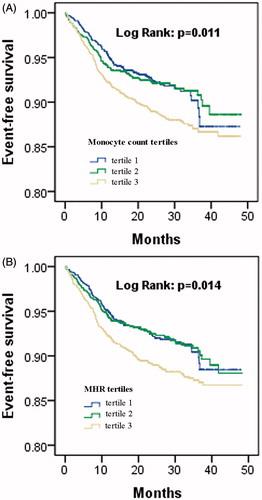
Figure 1. The levels of MHR (A), MC (B), and Gensini score (C) in patients with or without MACEs and the levels of Gensini score by MHR (D) or MC (E) tertiles.
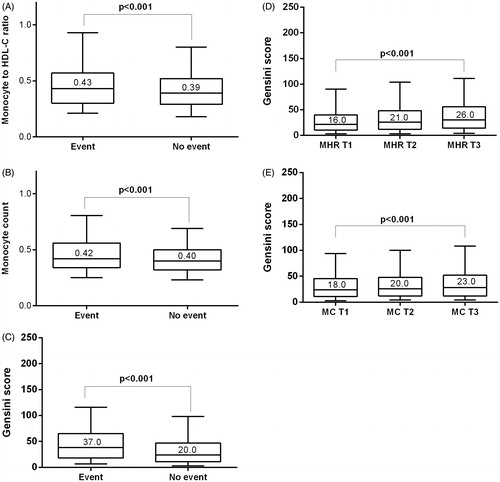
Table 1. Baseline and demographical characteristics of the study population.
Relation of MC and MHR with cardiovascular characteristics
Firstly, we made this analysis to reveal the association of baseline MC and MHR with cardiovascular characteristics. As a result, with increasing tertiles of MC or MHR, the levels of hs-CRP, left ventricular end diastolic diameter increased accompanied by left ejection fraction declined (p < 0.01, all, ). The prevalence of angiography proven CAD, left main artery diseased, and multi-vessels diseased was higher (p < 0.01, all, ), whereas the traditional risk factors were not different among groups (p > 0.05, all, ). The severity of coronary atherosclerosis assessed by Gensini score was dramatically higher in patients with MACEs (p < 0.001, ), and also in the upper tertile of MC or MHR (p < 0.001, all, and ).
Figure 2. The number of traditional cardiovascular risk factors by monocyte (A) or MHR (B) tertiles.
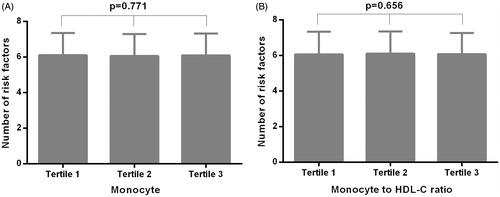
Table 2. Relationship of MHR or MC with cardiovascular characteristics.
Cardiac events during follow-up
The median period of follow-up was 24.6 months (interquartile range: 16.5–34.5 months). A total of 347 patients (9.1%) presented with MACEs during the follow-up period. Of these, 69 (19.9%) developed unstable angina pectoris, 32 (9.2%) suffered non-fatal MI, 10 (2.9%) developed heart failure, 169 (48.7%) underwent myocardial revascularization procedures (PCI or CABG) because of clinical deterioration, 43 (12.4%) had strokes, and 24 (6.9%) died (18 cardiac death).
Predictive value of MC or MHR on the risk of MACEs
As shows, patients in the upper MC or MHR tertiles had an increased risk of MACEs (p < 0.001, p = 0.002, respectively). The Kaplan–Meier analysis demonstrated a significant difference in the event-free survival rate among three groups (, p = 0.011, p = 0.014, respectively).
According to univariate Cox proportional hazard regression analysis, age, hypertension, DM, angiography proven CAD, Gensini score, WBC count, MC and MHR were all significantly associated with MACEs occurrence (p < 0.01, ). Consequently, to reveal the predictive value of MC and MHR, we further performed the multivariate adjustment for these potential risk factors. The data indicated that the associations of MC or MHR with MACEs were not substantially altered in this analysis (multivariate-adjusted model 2, MC: HR =2.734, 95%CI: 1.547–4.832; MHR: HR =2.031, 95%CI: 1.268–3.254, respectively, ). The ROC analysis revealed that both MC and MHR could predict MACEs, and the AUC were 0.574 (0.542–0.606) and 0.562 (0.530–0.594) (p < 0.001, both), respectively ().
Figure 4. The ROC analysis revealing the value of MHR (A) and MC (B) in predicting the future MACEs.
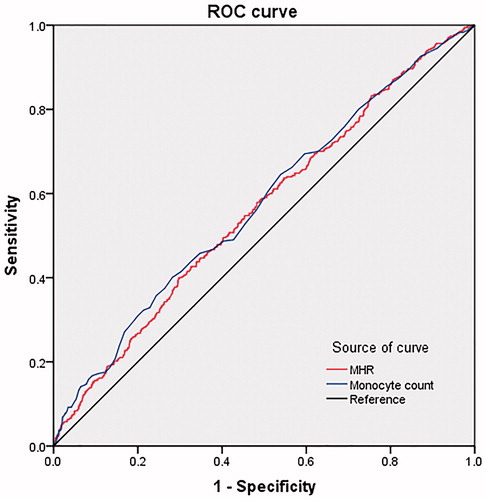
Table 3. Univariate Cox proportional hazard models results of the MACEs.
Table 4. Predictive value of white blood cell subsets and MHR tested by multivariate Cox proportional hazard models.
Discussion
In this prospective observational study, we aimed to focus on the prognostic value of MHR vs. MC on the occurrence of MACEs during a median 24.6 months follow-up. We demonstrated that MHR is an independent predictor of MACEs occurrence in patients undergoing coronary angiography. However, this predictive impact is not superior to MC in the current analysis. To the best of our knowledge, this is the first report for the comparison between MHR and MC directly in the same large cohort of patients with high cardiovascular risk.
As shown in various pathologic conditions, inflammation is a well-known mechanism during development and progression of atherosclerosis (Citation17). Monocytes as a distinct type of WBC, the subpopulations of intermediate (CD14 + CD16+; IM) and non-classical monocyte (CD-14 + CD16++; NCM) are both pro-inflammatory cells (Citation18). Not only inside the arterial wall but also in circulation, monocyte activation plays an important role in atherogenesis and atherothrombosis. The accumulation of macrophages correlates with the atherosclerotic plaque progression and rupture (Citation19,Citation20). Multiple evidences suggested a significant association of serum MC with the extent of atherosclerotic entities (Citation21,Citation22). Therefore, MC is a well-known prognostic factor for cardiovascular disease.
Dyslipidemia, the causal risk factor for CAD, has been investigated for decades. It has been evidenced that HDL particles exhibited anti-inflammatory effects on human monocytes by inhibiting activation of CD11b (Citation23). Based on the pro-inflammatory effect of monocyte and the anti-inflammatory effect of HDL, MHR was proposed as a novel marker to reflect the prognosis of cardiovascular diseases. In a recent study, Kanbay et al. enrolled 340 subjects with stages 1–5 chronic kidney disease and followed for a mean follow-up period of 33 months. They reported that MHR was negatively correlated with estimated glomerular filtration rate. Moreover, MHR was found to be associated with poor cardiovascular prognosis and emerged as an independent predictor of MACEs in patients with chronic kidney disease (Citation9). Similarly, the other study involving 402 patients with symptomatic atrial fibrillation, during 20.6 months of follow-up found that elevated pre-ablation MHR was associated with an increased recurrence of atrial fibrillation after cryoballoon-based catheter ablation (Citation10). Besides that, Kundi et al. compared MHR among 135 patients with isolated CAE, 135 patients with obstructive CAD, and 135 patients with normal coronary angiograms using a cross-sectional method. They finally concluded that MHR is significantly greater in patients with CAE and associated with the severity of CAE (Citation11). Furthermore, in patients with STEMI treated with PCI, MHR was observed to be an independent predictor of stent thrombosis, and was independently correlated with in-hospital MACEs and mortality after PCI (Citation12,Citation13). However, these previous investigations were limited by the relatively small sample size and were restricted to specific cardiovascular disease entities. To the extent of our knowledge, no study has investigated the prognostic role of MHR and compared with MC directly in a large cohort of patients with high cardiovascular risk who underwent coronary angiography. In our present study, we have found that MHR is an independent predictor of MACEs occurrence after adjusting for age, hypertension, DM, and Gensini score. Nonetheless, MHR was not superior to MC in predicting the outcomes of cardiovascular disease in the ROC analysis. We proposed that the pro-inflammatory property reflected by the high relationship between MHR and hs-CRP may partly contribute to the high risk of MACEs. Therefore, the results need to be testified by large scale non-treated patients in the near future.
There were several limitations of our study. First, there was not enough cardiovascular mortality in this study to allow direct survival analysis. Second, the observational design may be another limitation. Third, we only measured the baseline HDL-C level and MC, and measurements for once may not completely reflect the trend of the blood parameters.
Conclusions
In summary, we observed MHR was independently associated with cardiovascular parameters and future MACEs in a large cohort of Chinese Han patients undergoing coronary angiography. Specifically, our data for the first time suggested that the value of MHR was not superior to MC in predicting future MACEs.
Funding information
This work was partly supported by National Natural Science Foundation (81070171, 81241121), Specialized Research Fund for the Doctoral Program of Higher Education of China (20111106110013), Capital Special Foundation of Clinical Application Research (Z121107001012015), Capital Health Development Fund (2011400302), and Beijing Natural Science Foundation (7131014) awarded Dr. Jian-Jun Li, MD, PhD.
Acknowledgements
We are grateful to the field staff and the participants of our study.
Disclosure statement
The authors have no conflict of interests.
References
- Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685–95.
- Libby P. Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol. 2012;32:2045–51.
- Li JJ, Zhang YP, Yang P, Zeng HS, Qian XW, Zhang CY, et al. Increased peripheral circulating inflammatory cells and plasma inflammatory markers in patients with variant angina. Coron Artery Dis. 2008;19:293–7.
- Kim J, Song TJ, Park JH, Lee HS, Nam CM, Nam HS, et al. Different prognostic value of white blood cell subtypes in patients with acute cerebral infarction. Atherosclerosis. 2012;222:464–7.
- Ates AH, Canpolat U, Yorgun H, Kaya EB, Sunman H, Demiri E, et al. Total white blood cell count is associated with the presence, severity and extent of coronary atherosclerosis detected by dual-source multislice computed tomographic coronary angiography. Cardiol J. 2011;18:371–7.
- Hansson GK. Inflammatory mechanisms in atherosclerosis. J Thromb Haemost. 2009;7:328–31.
- Tardif JC, Gregoire J, L'Allier PL, Ibrahim R, Lesperance J, Heinonen TM, et al. Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: a randomized controlled trial. JAMA. 2007;297:1675–82.
- Murphy AJ, Woollard KJ, Hoang A, Mukhamedova N, Stirzaker RA, McCormick SP, et al. High-density lipoprotein reduces the human monocyte inflammatory response. Arterioscler Thromb Vasc Biol. 2008;28:2071–7.
- Kanbay M, Solak Y, Unal HU, Kurt YG, Gok M, Cetinkaya H, et al. Monocyte count/HDL cholesterol ratio and cardiovascular events in patients with chronic kidney disease. Int Urol Nephrol. 2014;46:1619–25.
- Canpolat U, Aytemir K, Yorgun H, Sahiner L, Kaya EB, Cay S, et al. The role of preprocedural monocyte-to-high-density lipoprotein ratio in prediction of atrial fibrillation recurrence after cryoballoon-based catheter ablation. Europace. 2015;17:1807--15.
- Kundi H, Gok M, Kiziltunc E, Cetin M, Cicekcioglu H, Cetin ZG, et al. Relation between monocyte to high-density lipoprotein cholesterol ratio with presence and severity of isolated coronary artery ectasia. Am J Cardiol. 2015;116:1685–9.
- Karatas MB, Canga Y, Ozcan KS, Ipek G, Gungor B, Onuk T, et al. Monocyte to high-density lipoprotein ratio as a new prognostic marker in patients with STEMI undergoing primary percutaneous coronary intervention. Am J Emerg Med. 2016;34:240–4.
- Cetin EH, Cetin MS, Canpolat U, Aydin S, Topaloglu S, Aras D, et al. Monocyte/HDL-cholesterol ratio predicts the definite stent thrombosis after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Biomark Med. 2015;9:967–77.
- Zhang Y, Li S, Zhu CG, Guo YL, Wu NQ, Xu RX, et al. Risk factors, coronary severity, outcome and ABO blood group: a Large Chinese Han Cohort Study. Medicine (Baltimore). 2015;94:e1708.
- Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51:606.
- Li JJ, Li S, Zhang Y, Xu RX, Guo YL, Zhu CG, et al. Proprotein convertase subtilisin/kexin type 9, C-reactive protein, coronary severity, and outcomes in patients with stable coronary artery disease: a Prospective Observational Cohort Study. Medicine (Baltimore). 2015;94:e2426.
- Fan J, Watanabe T. Inflammatory reactions in the pathogenesis of atherosclerosis. J Atheroscler Thromb. 2003;10:63–71.
- Yang RH, Liu YF, Wang XJ, Liang JG, Liu JC. Correlation between high density lipoprotein and monocyte subpopulations among stable coronary atherosclerotic heart disease patients. Int J Clin Exp Med. 2015;8:16969–77.
- Mestas J, Ley K. Monocyte-endothelial cell interactions in the development of atherosclerosis. Trends Cardiovasc Med. 2008;18:228–32.
- Woollard KJ, Geissmann F. Monocytes in atherosclerosis: subsets and functions. Nat Rev Cardiol. 2010;7:77–86.
- Palmerini T, Coller BS, Cervi V, Tomasi L, Marzocchi A, Marrozzini C, et al. Monocyte-derived tissue factor contributes to stent thrombosis in an in vitro system. J Am Coll Cardiol. 2004;44:1570–7.
- Glezeva N, Horgan S, Baugh JA. Monocyte and macrophage subsets along the continuum to heart failure: misguided heroes or targetable villains? J Mol Cell Cardiol. 2015;89:136--45.
- Ansell BJ, Navab M, Hama S, Kamranpour N, Fonarow G, Hough G, et al. Inflammatory/antiinflammatory properties of high-density lipoprotein distinguish patients from control subjects better than high-density lipoprotein cholesterol levels and are favorably affected by simvastatin treatment. Circulation. 2003;108:2751–6.