Abstract
Aims. The purpose of the present study was to compare the costs of home blood pressure (BP) telemonitoring (HBPM) with the costs of conventional office BP monitoring. In a randomized controlled trial, 105 hypertensive patients performed HBPM and 118 patients received usual care with conventional office BP monitoring during 6 months. Costs were quantified from the healthcare perspective. Non-parametric simulations were performed to quantify the uncertainty around the mean estimates and cost-effectiveness acceptability curves were made. Major findings. Systolic and diastolic daytime and night-time ambulatory BP (ABP) were reduced in both groups. The uncertainty around the incremental cost effectiveness ratio point estimates was considerable for both systolic and diastolic ABP. For systolic ABP, the difference in cost effectiveness ratio between the two groups was 256 Danish kroner (DKK)/mmHg [95% uncertainty interval, UI −860 to 4544]. For diastolic ABP, the difference in cost effectiveness ratio between the two groups was 655 DKK/mmHg [95% UI −674 to 69315]. Medication and consultation costs were lowest in the intervention group, but were offset by the cost of the telemonitoring equipment. Conclusions. Cost-effectiveness analysis showed that telemonitoring of home BP was more costly compared with usual monitoring of office BP. The cost-effectiveness result is surrounded with considerable uncertainty.
Trial registration: ClinicalTrials.gov identifier: NCT282334.
Background
Hypertension is one of the most common chronic conditions in the Western countries. The prevalence has been estimated as high as 44% on average in some European countries and 28% in North America (Citation1). Recent observational studies in the Danish adult population have estimated the prevalence of hypertension to be 5% on average in the 40–50 age group with increasing rates to around 20% in the 60+ age group (Citation2,Citation3). Lowering BP significantly reduces cardiovascular morbidity and mortality as proven in numerous clinical trials. Nevertheless, BP is controlled in only one third of adults with hypertension (Citation4) to an optimal level, as recommended in guidelines (Citation5,Citation6). Various factors play a part in the inadequate BP control. Patients’ non-adherence to prescribed medication has been cited as a major and important obstacle, but healthcare professionals also fail to attain BP targets and to some extent fail to utilize out-of-office BP measurements (Citation7). Ambulatory BP monitoring (ABPM) and home BP monitoring (HBPM) has proven superior to office BP measurements in the diagnosis of hypertension (Citation8,Citation9) and control of high BP (Citation10,Citation11). Both ABPM and HBPM provide better prognostic information than monitoring of office BP (Citation2,Citation3,Citation12).
In the USA, high BP is the most common chronic medical problem prompting visits to primary healthcare providers (Citation7). The cost of treating hypertension is high as is its complications. The American Heart Association estimated that the total cost in the United States in 2003 would be $50.3 billion – $37.2 billion in direct medical costs and $13.1 billion in indirect costs owing to lost productivity related to morbidity and mortality (Citation7). Thus, improved BP control is needed. A large amount of resources is allocated to treatment and control of hypertension, and some research has been done to obtain more effective and cost-effective ways to achieve better BP control. A Belgian study led to less intensive drug treatment for hypertension and marginally lower costs, when antihypertensive treatment was based on HBPM (Citation13). Other studies have suggested that telemonitoring of home BP may be a feasible and cost effective method (Citation10,Citation14). We have recently shown that antihypertensive treatment based on telemonitoring of home BP was as effective as treatment based on usual monitoring of office BP in lowering ABPM in a primary care setting over a period of 6 months (Citation15). Alongside that study, we performed an economic evaluation of the direct healthcare costs allocated to control and treatment of hypertension.
The purpose of the present study is to compare the costs of telemonitoring of home BP with the costs of conventional office BP monitoring.
Patients and methods
Design
The study was a randomized, controlled, unblinded trial of 6 months’ duration with comparison of direct healthcare costs of antihypertensive treatment based on telemonitoring of home BP (intervention group) and conventional office BP monitoring (control group).
Ethics
The study was approved by the local ethics committee. ClinicalTrials.gov identification number is NCT 00282334. All participants provided written informed consent before entering the study.
Enrolment
Between April 2004 and April 2006, nine general practitioners consecutively recruited the study participants among their patient population.
Participants
Inclusion criteria were: age 20–80 years, both men and women, newly diagnosed or treated hypertension but not controlled hypertension with elevated office BP (>150/95 mmHg or systolic BP > 150 mmHg and diastolic BP < 90 mmHg). Exclusion criteria were: 24-h ambulatory BP monitoring (ABPM) ≤125/80 mmHg, atrial fibrillation (ECG at randomization), and lack of mental or physical capacity to perform HBPM. The withdrawal criterion was: withdrawal of consent to participate.
Randomization
A random number generator produced a random allocation sequence. Allocations were transferred to numbered, sealed, opaque envelopes and opened sequentially by the participants after enrolment at the Department of Medical Research.
Procedures
Intervention group
Patients in the intervention group were provided HBPM equipment. This equipment included a validated (Citation16), semiautomatic oscillometric BP measuring device (Omron 705 IT, Omron Matsusaka Co., Ltd., Japan) connected to a personal digital assistant (Hewlett Packard iPAQ Pocket PC, Hewlett-Packard Company, Houston, TX, USA) with a software interface developed for BP measurement (Bang & Olufsen Medicom, Struer, Denmark and CIM Electronics, Hasselager, Denmark). BP measurements were transferred to a central server by a PDA-embedded mobile phone unit. Doctors accessed their patients’ BP measurements on a secure home page. Each patient could access their own BP measurements on this web site, where they could also communicate with their general practitioner by e-mail. For patients with no internet access, the PDA could record and send spoken messages to the general practitioner, who could respond by written messages to the PDA.
Patients measured their BP between 09:00 and 20:00 h three times a week during the first 3 months and once a week during the last 3 months. Each BP measurement consisted of three readings with 1-min intervals. General practitioners instructed their patients in correct BP measuring technique (Citation5). The goal was to achieve target home BP for each patient. Target home BP was BP < 135/85 mmHg for patients without diabetes and lower if diabetic, as recommended in current guidelines (Citation5).
Control group
The frequency of office visits was decided by the patients’ usual doctor according to usual practice. Office BP was measured with the same type BP device as used for HBPM. The goal was to achieve target office BP for each patient. Target BP was BP<140/90 mmHg for patients without diabetes and <130/80 mmHg if diabetic, as recommended in current guidelines (Citation5).
Antihypertensive treatment
In both groups, the antihypertensive treatment was instituted and/or changed at the discretion of the patients’ general practitioner according to current guidelines.
Assessment of costs
As the monitoring is seen as a permanent intervention, the ideal cost measure would be the long run marginal costs. We used the conventional method of measuring average total costs as an approximation for assessment of long run marginal costs, which we were not able to measure (Citation17). Resource utilization was divided into four categories: medication costs (antihypertensive medication costs), consultation costs (office visits), costs of equipment and costs related to telemonitoring of home BP. Unit costs were assigned Danish prices as of August 2007. Costs are given in Danish kroner (DKK), 1 DKK = €0.13.
Medication costs
For each patient, the actual prescriptions and doses of antihypertensive medication were used. The length of treatment (in weeks) was also included in the total cost. A price per day for each used drug was obtained from an online database on medication costs (Citation18) using the most recent resale prices, including the pharmacist dispensing fee. The price per day was then multiplied by the number of days that the drug(s) was given. Since medications were prescribed during the study from 2004 through 2006, present prices were regulated by the net price index in order to determine the prices of each of the years in question.
Consultation costs
The standard cost of an office visit was used as negotiated by the Danish National Health Service and the Danish Medical Association. The standard basic fee per patient was included in the cost for a 6-month period.
Costs of equipment
These costs were determined based on the following assumptions:
relevant to the HBPM costs were the costs of the BP measuring device, PDA including mobile phone unit, data transfer to and from mobile phones, and server hosting (web site);
the HBPM equipment was depreciated over 4 years using the annuity method, with an interest rate of 5% (Citation17) providing an equivalent annual cost;
It was assumed that the HBPM equipment could be re-used for about eight times over a period of 4 years. It was also assumed that the equipment could have a resale value of 300 DKK after the study period.
Costs related to telemonitoring
The cost of HBPM consisted of the instruction in HBPM by doctors and the electronic telemonitoring costs. These costs were determined based on the following assumptions:
Patients were given instructions on how to perform home BP measurements and how to use the HBPM equipment by the general practitioner after randomization during a visit for 15 min.
Costs related to data transfer to and from mobile phones were converted to present prices with the same net price index as used for price regulation of medication costs.
Server hosting costs were given in present prices and based on the maximum number of patients it would be possible to monitor with the equipment produced to the study (150/6 months).
Effect variable
The primary effect variable was cost-effectiveness ratio. It was assessed as incremental cost-effectiveness ratio (ICER), expressed as the cost of lowering systolic and diastolic ABPM by 1 mmHg.
Analyses
Costs were quantified from the healthcare perspective. This perspective only takes medical costs into account (either paid for by the Danish National Health Service or by the patients themselves). Data were analyzed according to the intention-to-treat principle. Missing data, as a result of incompleteness, were then substituted by the total group mean. In order to assess whether the results were robust to a change in the method of handling missing data, an analysis based on complete case analysis was also performed. Statistical significance level was set at p < 0.05. Results are given as mean (SD) or median (interquartile range) as appropriate.
Non-parametric bootstrap simulations (2000 replications) were conducted to evaluate the uncertainty around the incremental costs, incremental effects and ICERs (Citation19). From these data, 95% uncertainty intervals (UI) for cost and effect differences were calculated. In a bootstrap simulation, a sample of cost and effect pairs of equal size of the original sample is selected a number of times at random with replacement. For each pair, the differences in costs and in outcome were measured. These simulations are presented in a cost-effectiveness plane and yield information concerning the joint distribution of the cost and effect differences. Cost effectiveness acceptability curves (CEAC) were made showing the probability that telemonitoring is cost effective at various cost levels. Analyses were performed using the SPSS 13.0 software; the bootstrap simulations were generated using Stata 9.0.
Results
The study group
summarizes the flow of patients through the study. In total, 244 patients were included in the study by the general practitioners. Before randomization, eight patients were excluded: seven patients had AMBP ≤125/80 mmHg and one patient was unwilling to participate. No follow-up data were available for eight patients in the telemonitoring group and five patients in the control group. The intervention group comprised 105 patients, 54 women and 51 men, 55 ± 12 years (mean ± SD). The control group comprised 118 patients, 59 women and 59 men, 57 ± 12 years. In both groups, about half was diagnosed with hypertension within 1 year prior, 60/113 (53%) in the intervention group and 56/113 (50%) in the control group (information not provided in 10 patients). There were no differences in BP, age and gender between patients who completed the study and patients who did not attend follow-up.
Main BP results
After 6 months, daytime ABPM was reduced by 11.9/6.2 mmHg in the intervention group and 9.6/5.4 mmHg in the control group with no significant differences between the groups. Reductions in systolic and diastolic night-time ABPM were also similar in the two groups (Citation15).
Costs related to antihypertensive medication
In both groups, the total number of antihypertensive drugs increased during the study to two drugs per patient on average (Citation15). The actual costs related to antihypertensive treatment were calculated as described above. Analysis showed that medication costs were lower during telemonitoring of home BP than during usual BP monitoring. shows that antihypertensive medication amounted to 471 DKK in the intervention group and 628 DKK in the control group, p = 0.030. The mean number of medications was, however, the same in the two groups at follow-up, but it would seem as patients receiving usual care were treated with more expensive medications. shows the type of antihypertensive medications prescribed at baseline and follow-up. At baseline, the distribution of antihypertensive medications did not differ between the two groups. At follow-up, significantly more patients were treated with angiotensin 2 (AT2)-antagonists in the control group than in the intervention group.
Table I. Healthcare costs related to 6 months’ of blood pressure monitoring in the two treatment groups.
Table II. Prescribed antihypertensive medications at baseline and after 6 months in two treatment groups.
Costs related to blood pressure monitoring (consultation/telemonitoring)
The standard consultation fee was 133 DKK. The standard basic fee per patient received by the general practitioner was 143 DKK per 6 months. This fee was included in the cost calculations in both groups.
Intervention group. Instruction in HBPM was given during one scheduled office visit at the beginning of the study. During the rest of the study period, the HBPM equipment was used. The number of doctor–patient telecommunications in the telemonitoring group was 7 (Citation3–12), median (interquartile range). Costs related to HBPM were server hosting and mobile phone data transfer between the HBP monitor and the central server. As shown in , the total cost of HBPM in the intervention group was 2090 DKK, of which more than half was allocated to equipment costs.
Control group. Median number of office visits in the control group was 4 (Citation3–6). The mean costs related to BP monitoring visits to the doctor's office were 751 (326) DKK accounting for more than half of the total BP monitoring costs of 1379 (796) DKK, as stated in .
Costs of equipment
HBPM equipment was calculated to an equivalent semi-annual cost of 944 DKK. The total cost per HBPM unit was 6700 DKK and comprised the cost of PDA, mobile phone unit and SD card with BP-measuring interface software. As mentioned above, the HBPM equipment was depreciated over 4 years using the annuity method (5% interest rate) (Citation17).
Total costs
As shown in , the total cost of HBPM in the intervention group was 2090 DKK, which composed 944 DKK for cost of equipment and the rest was 1146 DKK. The total costs in the control group were 1379 DKK.
Cost-effectiveness
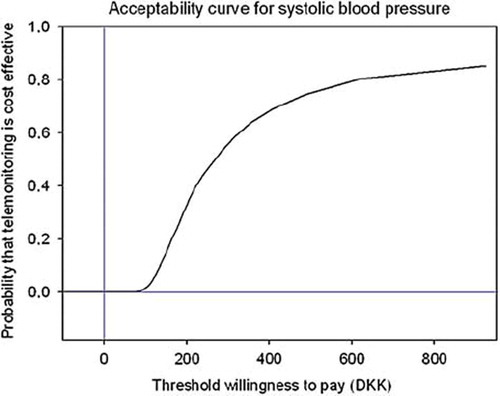
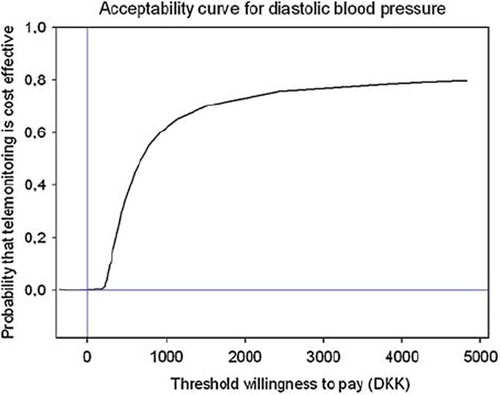
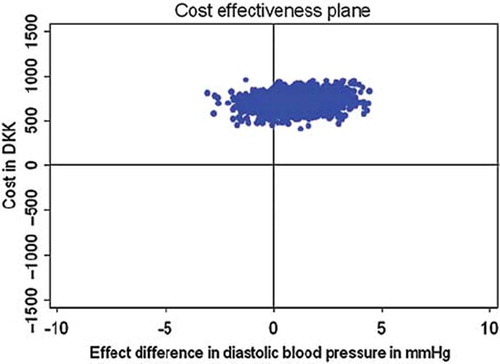
From the healthcare perspective, the cost savings of telemonitoring of home BP obtained by lower consultation and medication costs were offset by the cost of the HBPM equipment. The uncertainty around the ICER point estimates was considerable for both systolic and diastolic ambulatory BP. For systolic ABPM, the difference in cost effectiveness ratio between the two groups was 256 DKK/mmHg and the 95% UI ranged from −860 to 4544. The uncertainty around this outcome is visualized in the cost-effectiveness plane in . For diastolic ABPM the difference in cost-effectiveness ratio between the two groups was 655 DKK/mmHg and the 95% UI ranged from −674 to 69315. The uncertainty around this outcome is illustrated in the cost-effectiveness plane in . For both systolic and diastolic ABPM the major part of the replicates are placed in the north-east quadrant of the cost-effectiveness plane. This indicates that intervention is more effective but also more costly than conventional office BP monitoring. The choice therefore depends on the maximum amount one is willing to pay for a unit reduction in BP. The derived cost-effectiveness acceptability curves are presented in and . It appears from the curves that there is a probability of 50% that the cost of home telemonitoring for systolic BP costs less than 268 DKK and for diastolic BP less than 681 DKK.
Figure 2. Cost effectiveness plane for systolic ambulatory blood pressure monitoring (ABPM) and total cost related to blood pressure monitoring in DKK per patient per 6 months. Cost effectiveness plane constructed with 2000 bootstrap replications, showing the uncertainty around the point estimate of cost effectiveness of antihypertensive treatment based on home blood pressure monitoring (HBPM) vs usual care from the healthcare perspective. A positive effect difference indicates a larger drop in systolic ABPM in the HBPM group, whereas a negative effect difference indicates a larger drop in systolic ABPM in the control group.
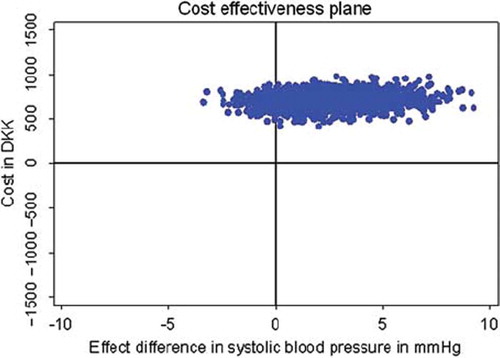
Figure 3. Cost effectiveness plane for diastolic ambulatory blood pressure monitoring (ABPM) and total cost related to blood pressure monitoring in DKK per patient per 6 months. Cost effectiveness plane constructed with 2000 bootstrap replications, showing the uncertainty around the point estimate of cost effectiveness of antihypertensive treatment based on home blood pressure monitoring (HBPM) vs usual care from the healthcare perspective. A positive effect difference indicates a larger drop in diastolic ABPM in the HBPM group, whereas a negative effect difference indicates a larger drop in diastolic ABPM in the control group.
Discussion
In the present study, we demonstrated that the use of telemonitoring with home BP measurement was more expensive than conventional office BP monitoring in the treatment and control of patients with arterial hypertension. However, the telemonitoring equipment was designed and developed for the study, and its cost was a major contributor to the cost in the intervention group. The costs of medication and consultation were lower in the intervention group than in the control group.
Our study was done from a healthcare perspective. A societal perspective analysis was not performed, as the intervention would only have a small impact on non-healthcare costs. Furthermore, by including only the direct healthcare costs and omitting indirect healthcare costs, i.e. loss of production because of patients’ absence from work, the study would be more general. We attempted to evaluate the cost-effectiveness of intervention under real-world conditions. Firstly, hypertensive patients were recruited from several primary care practices, and patients and general practitioners were fairly typical. Secondly, the intervention was compared with current standard treatment and control as general practitioners determined the frequency of office visits and types and doses of antihypertensive drugs.
The cost of home BP telemonitoring has been assessed by other studies (Citation10,Citation14,Citation20,Citation21). The majority of these studies were performed from the patient or healthcare perspective. Comparisons between studies are difficult because of different study designs and effect variables. In a small, unrandomized study of uncontrolled hypertension, Bondmass et al. (Citation20) estimated the inclusive cost of the system and method used in the study at US$3.50 per patient per day during a 3-month period. In a small study of nurse-managed telephone-linked HBPM, Artinian et al. (Citation21) calculated the cost of telemonitoring at US$1.50 per patient per day including only the cost of equipment, shipping of equipment, telephone training and teletransmission of data. Rogers et al. (Citation10) have published the results of a larger, randomized controlled trial with a study design comparable with the design of the present study and showed that HBPM with automated transmission of data to general practitioners via service center costs of US$24.95 per patient per month (Citation10). These costs are in line with the results in the present study. Friedmann et al. (Citation14) calculated the cost per mmHg decrease in diastolic BP and found that per 1 mmHg decrease in diastolic BP the cost was US$7.39. The cost per patient for 6 months’ use was US$32.50 (Citation14). However, none of the studies included a comparison of cost between the intervention and control group. In our study, the HBPM equipment was the main cost contributor in the intervention group. Consultation and medication costs were lower in the telemonitoring group than in the control group, but this was offset by the cost of telemonitoring. If the telemonitoring equipment could be produced at a lower cost than in the present study, the cost-effectiveness ratio would be altered in favor of home BP telemonitoring.
Surprisingly, the costs of medication were higher in the control group than in the intervention group. At baseline, the distribution of antihypertensive medications did not differ between the two groups. However, significantly more patients were treated with AT2-antagonists in the control group at follow-up than in the intervention group. As AT2-antagonists are more expensive in Denmark compared with other antihypertensive agents, it would explain the higher medication costs in the control group. It cannot be excluded that general practitioners have intensified treatment during the study by prescribing more antihypertensive medication than they would have done, had they not participated in a study.
As expected, the costs of consultation were lowest in the telemonitored group. The cost of an office visit can be calculated in different ways. We chose to use the standard cost of an office visit as negotiated by the Danish National Health Service and the Danish Medical Association, as this cost is readily available. This standard cost represents the cost that the National Health Service had for each office visit. We then chose to add the basic fee received by the general practitioner per patient registered in the practice. However, this basic fee does not only cover consultations regarding BP control, but also other consultations in the same period. Furthermore, the standardized fee is a result of negotiation and therefore based on approximations and calculations of typical time consumption and office costs. Another method could therefore have been to calculate the basic fee proportionally into the consultations fee. This method would result in a slightly higher increment, but only around 25 DKK, as consultations costs in the control group would increase. Yet another alternative method could have been to use standardized values as suggested by Oostenbrink et al. (Citation22). The true cost of an office visit may not, however, be represented by any of the above-mentioned methods, but will almost always be based on assumptions. It must also be noted that medication costs are VAT included, while equipment and office fees are not. However, as VAT is included in both treatment groups the cost-effectiveness ratios are only slightly affected. Our analysis clearly showed a pronounced reduction in consultation costs during telemonitoring compared with conventional antihypertensive treatment.
Our cost-effectiveness analysis showed that the major part of the replicates was placed in the north-east quadrant of the cost-effectiveness plane for both systolic and diastolic ABPM. This indicates that telemonitoring is more effective and also more costly than conventional BP treatment and monitoring. The choice of monitoring modality therefore depends on the maximum amount one is willing to pay per unit of reduced BP. It seems straightforward that development of cheaper telemonitoring equipment would be a way to improve the cost-effectiveness ratio in favor of telemonitoring.
The study has some limitations regarding the evaluation of the cost-effectiveness ratio. Firstly, by imputing the group mean for missing values, the variation is reduced, and the degree of uncertainty has been underestimated. Therefore, the uncertainty interval around the cost difference may be too small. Secondly, though there are no strong reasons to suppose that the effectiveness of HBPM would be different in other countries, transferability of costs to other countries is problematic, because of marked differences in social insurance systems across countries (Citation23). Thirdly, the price level regarding medication may also differ between countries. As a consequence, the cost-effectiveness results can only be transferred to other healthcare systems with considerable reservations. Fourthly, the assessment of long-term marginal costs would be the preferred method of cost calculation but the average total costs can be used as an approximation (Citation17). Finally, it cannot be ruled out that the number of consultations in the control group were higher than usual practice and thereby masking the true difference in costs related to BP monitoring between the groups. Furthermore, our study was as previously stated done from a healthcare perspective and did not include any indirect costs.
Conclusions
In conclusion, the cost-effectiveness analysis showed that telemonitoring of home BP was more effective but also more costly compared with usual monitoring of office BP within a time horizon of 6 months. The cost-effectiveness result is, however, surrounded with considerable uncertainty and does not favor one method over the other. Our analysis showed that the costs of equipment for home BP telemonitoring were very high. Telemonitoring as a new principle for BP treatment and control may be a promising alternative to existent clinical practice, if the costs to equipment could be reduced.
Authors’ contributions
LBM carried out the study, analyzed data and drafted the manuscript. TC interpreted data. PK participated in the design of the study. EBP conceived of the study, participated in its design and interpreted data. All authors read and approved the final manuscript.
Acknowledgements
The authors thank the laboratory technicians at the Department of Medical Research for skillful and committed assistance. General practitioners Lars Dudal Madsen, Allan Raft, Benny Johannessen, Niels Christian Bendtsen, Bent Drechsler, Poul Erik Hven, Michael Hoffmann, Kurt Ebbensgaard and Bent Larsen are thanked for trustingly recruiting patients from their practices. Kristian Larsen is thanked for statistical assistance. The study was funded by grants from Ringkjøbing County, the Danish Ministry of Science, and the Danish Heart Foundation (Grant Number 07-4-B340-A1446-22372).
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampoli S, Joffres MR, . Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43:10–17.
- Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure and mortality. A population-based study. Hypertension. 2005;45:499–504.
- Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure monitoring and risk of cardiovascular disease: A population based study. Am J Hypertens. 2006;19:243–250.
- Ong KL, Cheung BMY, Man YB, Lau CP, Lam KSL. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75.
- The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC). 2007 Guidelines for the Management of Arterial Hypertension. J Hypertens. 2007;25:1105–1187.
- Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA. 2003;289:2560–2572.
- Elliott WJ. The economic impact of hypertension. J Clin Hypertens. 2003;5(3 Suppl 2):3–13.
- Møller DS, Dideriksen A, Sørensen S, Madsen LD, Pedersen EB. Accuracy of home blood pressure measurement in the diagnosis of hypertension. J Hum Hypertens. 2003;17: 549–554.
- Rogers MAM, Buchan D, Small D, Stewart CM, Krenzer BE. Telemedicine improves diagnosis of essential hypertension compared with usual care. J Telemed Telecare. 2002;8: 244–349.
- Rogers MAM, Small D, Buchan DA, Butch CA, Stewart CM, Krenzer BE, . Home monitoring service improves mean arterial pressure in patients with essential hypertension. Ann Intern Med. 2001;134:1024–1032.
- Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: Meta-analysis of randomized trial. BMJ. 2004;329:145–150.
- Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, . Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: A population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–975.
- Staessen JA, Den Hond E, Celis H, Fagard R, Keary L, Vandenhoven G, ., for the Treatment of Hypertension Based on Home or Office Blood Pressure (THOP) Trial Investigators. Antihypertensive treatment based on blood pressure measurement at home or in the physician's office: A randomized controlled trial. JAMA. 2004;291: 955–964.
- Friedmann RH, Kazis LE, Jette A, Smith MB, Stollerman J, Torgerson J, Carey K. A telecommunications system for monitoring and counseling patients with hypertension. Impact on medication adherence and blood pressure control. Am J Hypertens. 1996;9:285–292.
- Madsen LB, Kirkegaard P, Pedersen EB. Blood pressure control during telemonitoring of home blood pressure. A randomized controlled trial during six months. Blood Pressure. 2008;17:78–86.
- El Assaad MA, Topouchian JA, Asmar RG. Evaluation of two devices for self-measurement of blood pressure according to the international protocol: The Omron M5-I and the Omron 705IT. Blood Press Monit. 2003;8:127–133.
- Drummond MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. 3rd. Oxford: Oxford University Press; 2005.
- Danish Medicines Agency (Lægemiddelstyrelsen). Medicine prices on-line service. http://laegemiddelstyrelsen.dk/1024/visLSArtikel.asp?artikelID=864.html. Accessed August 13, 2007.
- Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: A non-parametric approach to confidence interval estimation. Health Econ. 1997;6:327–340.
- Bondmass M, Bolger N, Castro G, Avitall B. The effect of home monitoring and telemanagement on blood pressure control among African Americans. Telemed J. 2000;6:15–23.
- Artinian NT, Washington OGM, Templin TN. Effects of home telemonitoring and community-based monitoring on blood pressure control in urban African Americans: A pilot study. Heart Lung. 2001;30:191–199.
- Oostenbrink JB, Koopmanschap MA, Rutten FFH. Standardisation of costs. The Dutch manual for costing in economic evaluations. Pharmacoeconomics. 2002;20:443–454.
- Welte R, Feenstra T, Jager H, Leidl R. Decision chart for assessing and improving the transferabilty of economic evaluation results between countries. Pharmacoeconomics. 2004;22:857–876.