Abstract
Background. Auscultatory measurement using a sphygmomanometer has been the predominant method for clinical estimation of blood pressure, but it is now rapidly being replaced by oscillometric measurement. Objective. To compare blood pressure by auscultatory and oscillometric measurements in patients ≥ 80 years. Method. 100 patients had blood pressure measured by auscultation with a sphygmomanometer and by an electronic device using the oscillometric method. For each patient the mean of two blood pressures with each method measured within 15 min were compared. Results. The mean age of participants was 85.8 years; 55.8% were women. The correlation coefficient for systolic blood pressure was 0.88 and for diastolic 0.79. Differences between auscultatory and oscillometric values were less than 10 mmHg in 70.6% of systolic blood pressures and in 83.2% for diastolic. Arrhythmia and hypertension did not influence the results, and there was no correlation between the magnitude of the differences and the level of blood pressure. Conclusion. Agreement between oscillometric and auscultatory measurements of blood pressure in octogenarians was found to be less than required by validation protocols. However, semi-automatic equipment, which is observer-independent, may be used even in the very elderly, particularly if multiple readings are performed.
Introduction
Blood pressure-related cardiovascular diseases are prevalent causes of death and disability in all populations and all age groups. Reduction of elevated blood pressure reduces this morbidity and mortality effectively (Citation1,Citation2). Reliable assessment of blood pressure is vitally important, and for this purpose, auscultatory measurement using a sphygmomanometer has been the predominant method. There are, however, disadvantages attached to this technique. It requires specific training and accuracy not always performed in clinical practice to the same degree as in the clinical trials having established the importance of blood pressure levels. Furthermore, mercury is highly toxic, which has led to strategies for its replacement with other techniques (Citation3). Two alternatives to the mercury sphygmomanometer are currently available, namely other utensils using the auscultatory method with aneroid manometers or pressure transducers, and oscillometric devices.
Mercury manometers are increasingly replaced by semi-automatic and automatic oscillometric devices, which by individual evaluation have been shown to be accurate and recommended for clinical use (Citation4). They are, however, assumed to have limited accuracy in cases of cardiac arrhythmia and in patients with stiff arteries (Citation5), such as diabetics and the elderly (Citation6–8).
The aim of the present study was to compare blood pressure measured in octogenarians by auscultatory and oscillometric techniques.
Methods
One hundred consecutive patients aged 80 years or more admitted to the Department of Geriatric Medicine, Odense University Hospital were included in the study after informed consent. Blood pressure was measured by one person according to guidelines (Citation9) after proper training. A sphygmomanometer (Accoson Freestyle, Accoson Works, Harlow, UK) mounted with a cuff (TriCUFF, AJ Medical KB, Sweden) automatically assuring proper size was used for auscultatory measurements. The A&D UA 767PC (A&D Company, Ltd, Tokyo, Japan) with normal or small cuffs as required was used for oscillometric measurements. Measurements were performed within a 15-min period after 10 min of rest in the sitting or supine position. Auscultatory (aus) and oscillometric (osc) blood pressures were measured in the following order with at least 30-s intervals: BP1 (aus), BP2 (aus), BP3 (osm), BP4 (osc), BP5 (osc) and BP6 (aus). The pulse was checked manually for irregularity and arrhythmia diagnosed by ECG. Arm circumference and comorbidity were recorded.
The means of BP2 and BP6 representing auscultatory and BP4 and BP5 representing oscillometric measurements were calculated for each patient. The differences between auscultatoric and oscillometric means were grouped as follows: very accurate 0–5 mmHg (group 1), slightly inaccurate 6–10 mmHg (group 2), moderately inaccurate 11–15 mmHg (group 3) and very inaccurate >15 mmHg (group 4) (Citation9).
Results
One hundred patients were included in the study. Five were subsequently excluded because of erroneous oscillometric measurements. Four of these had irregular pulse and three atrial fibrillation; thus 95 patients were included in the analysis. Their median age was 85 years (78–101 years); 53 were females. Twenty-two had irregular pulse: 14 atrial fibrillation, four sinus arrhythmia and one pace rhythm. In the remaining three, ECG was not available.
shows blood pressure in the whole group by the two methods: systolic 121 and 120 mmHg and diastolic 63 and 64 by auscultation and oscillometry, respectively. The correlation between pressures measured by the two methods is shown in . The correlation coefficient for systolic blood pressure was 0.88 and for diastolic 0.79. The difference between auscultatory and oscillometric measurements was less than 10 mmHg in 70.6% of the patients for systolic and 83.2 for diastolic pressures () and differences were positive as well as negative (). There was no significant difference between the number of patients with small differences (group 1) with and without arrhythmia and hypertension as shown in . There was no correlation between the difference between pressures by the two methods and blood pressure levels (correlation coefficient for systolic 0.06 and for diastolic 0.18) ().
Table I. Blood pressure by method.
Figure 1. Correlation between auscultatory (aus) and oscillometric (osc) blood pressures. Systolic blood pressure, r = 0.88; diastolic blood pressure, r = 0.79.
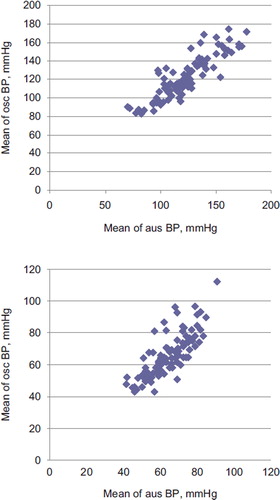
Table II. Differences between auscultatory and oscillometric measurements.
Figure 2. Difference between auscultatory (aus) and oscillometric (osc) blood pressures vs blood pressure.
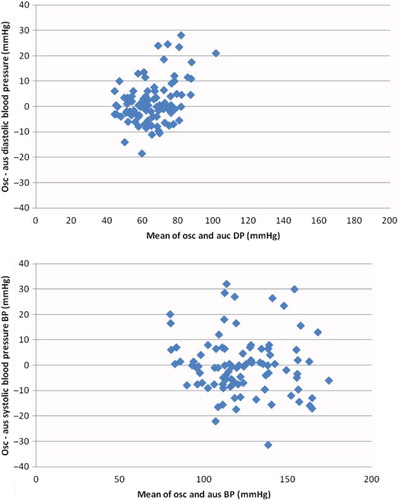
Table III. Fractions of patients with very accurate (group 1) measurements according to co-morbidity.
Seventeen of the patients (18%) had arm circumference smaller than 22 cm, and thus required a small cuff.
Discussion
Oscillometric blood pressure measurement has been found to be unreliable in patients with cardiac arrhythmias and arterial stiffness as in diabetes mellitus and advanced age. Overestimation of systolic as well as diastolic blood pressure is associated with arterial stiffness, pulse pressure and age (Citation5,Citation10). Also, small arm circumference has been found to be associated with inaccurate oscillometric readings (Citation10).
The oscillometric device used in this study was validated in a research setting and rated A/A by the British Hypertension Society protocol (Citation11). In the present clinical setting, differences of systolic as well as diastolic pressure were more frequent at all levels, not meeting the requirements of the validation protocol. This underlines the importance of evaluation of individual oscillometric devices in the clinical field and in particular populations.
The present study comparing oscillometric with auscultatory blood pressure measurements in very elderly patients showed a correlation with differences less than 10 mmHg in 71% for systolic and 83% for diastolic blood pressures compared with >90% required by the validation protocol used for the tested device. Differences of no clinical significance (< 5 mmHg) were found in only 43% of systolic and 61% of diastolic pressures vs 80% required by the validation protocol for A/A grading (Citation12). Such inferior performance in clinical practice is found in other studies. Accuracy is, however, improved by multiple readings (Citation13).
The frequency of accurate readings was relatively low but independent of cardiac arrhythmia and hypertension for both systolic and diastolic blood pressure. In the majority of cases, the agreement was within 10 mmHg.
It is important to notice that 18% of the octogenarians had arm circumference small enough to require a smaller than normal cuff size in order to avoid underestimation of blood pressure (Citation14).
It is a potential limitation of this study that it is not performed strictly according to the validation protocol; thus all measurements are performed by the same observer, which might overestimate the agreement between the two techniques. Also, the study population did not include patients with grade 3 hypertension.
This study of oscillometric compared with auscultatory blood pressure measurements discloses larger differences than allowed in validation protocols, but we suggest that the advantage of no observer dependence, and therefore elimination of last digit preference, may make the oscillometric measurement acceptable and perhaps preferable in the clinical setting even with very elderly patients, particularly if multiple readings are used.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Ezzati M, Lopez AD, Rodgers A, Van der Horn S, Murray CJL. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–1360.
- Blood Pressure Lowering Treatment Trialists’ Collaboration. Effect of different blood-pressure-lowering regimens on major cardiovascular events: Results of prospectly-designed overviews of randomised trails. Lancet. 2003;362:1527–1535.
- Scientific Committee on Emerging and Newly Identified Health Risks (SCENIHR). Mercury sphygmomanometers in healthcare and the feasibility of alternatives. European commission, directorate general for ‘health and consumers’. http://ec.europa.eu/health/ph_risk/committees/04_scenihr_opinions_en.htm#2.
- O'Brien E, Asmar A, Beilin L, Imai Y, Mallion JM, Mancia G . European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–848.
- Popele NM, Bos WJW, Beer NAM, van der Kuip DAM, Hofman A, Grobbee DE, Witteman JCM. Arterial stiffness as underlying mechanism of disagreement between an oscillometric blood pressure monitor and a sphygmomanometer. Hypertension. 2000;36:484–488.
- Miller ST, Elam JT, Graney MJ, Applegate WB. Discrepancies in recording systolic blood pressure of elderly persons by ambulatory blood pressure monitor. Am J Hypertens. 1992; 5:16–21.
- O'Brien E, Mee F, Atkins N, O'Malley K. Technical aspects of ambulatory blood pressure monitoring in the elderly. Cardiol Elderly. 1993;1:464–469.
- Staessen JA, Fagard R, Thijs L, Amery A. A consensus view on the technique of ambulatory blood pressure monitoring. Hypertension. 1995;26:912–918.
- O'Brian E, Pickring T, Asmar R . Working group on blood pressure monitoring of European Society of Hypertension international protocol for validation of blood pressure devices in adults. Blood Press Monit. 2002;7:3–17.
- Stergiou GS, Lourida P, Tzamouranis, Baibas NM. Unreliable oscillometric blood pressure measurement: Prevalence, repeatability and characteristics of the phenomenon. J Human Hypertens. 2009;23:794–800.
- Rogoza AN, Pavlova, TS, Sergeeva, MV. Validation of A&D UA–767 device for the self-measurement of blood pressure. Blood Press Monit. 2000;5:227–231.
- O'Brien E, Petrie J, Littler W, de Swiet M, Padfield PL, O'Malley K . The British Hypertension Society protocol for the evaluation of automated and semi-automated blood pressure measuring devices. J Hypertens. 1990;8:607–619.
- Wan Y, Heneghan C, Stevens R, McManus RJ, Ward A, Perera R, Thomson M . Determining which automatic digital blood pressure device performs adequately: A systematic review. J Human Hypertens. 2010;24:431–438.
- Beevers G, Lip GY, O'Brien E.ABC of hypertension: Blood pressure measurement. Part II-conventional sphygmomanometry: Technique of auscultatory blood pressure measurement. BMJ. 2001;322:1043–1047.